Abstract
Angiotensin receptor blockers are contraindicated drugs during pregnancy because of their potential fetotoxicity, including oligohydramnios, anuria, renal tubular dysplasia, limb contractures, cranial ossification defects, prolonged patent ductus arteriosus, and even in utero death. It is believed that these abnormalities are associated with drug-mediated fetal hypotension. We report a case of skull ossification defects, pneumothorax, renal parenchymal disease, congenital calcaneovalgus foot, and inferior vena cava thrombosis in a neonate born to a hypertensive woman who had continued use of an angiotensin receptor blocker during her pregnancy.
Use of angiotensin converting enzyme inhibitors or angiotensin receptor antagonists (ARBs) in the second and third trimesters of pregnancy has been associated with oligohydramnios, anuria, renal tubular dysplasia, limb contractures, cranial ossification defects, prolonged patent ductus arteriosus, and even in utero death. It is believed that these abnormalities are associated with drug-mediated fetal hypotension.123456
We report a case of skull ossification defects, pneumothorax, renal parenchymal disease, congenital calcaneovalgus foot, and inferior vena cava (IVC) thrombosis in a neonate born to a hypertensive woman who had continued use of ARBs during her pregnancy.
A newborn infant (birth weight 3.2 kg, expected Ballard score gestational age [GA] 40 weeks, spontaneous vaginal delivery) was transferred to our hospital for evaluation of impalpable skull bones.
His mother was a 35-year-old woman with chronic hypertension treated with valsartan (an ARB) and had moderate mental retardation. She was not aware of her pregnancy and had continued use of her antihypertensive drugs throughout her pregnancy and visited an emergency room with abdominal pain, which turned out to be labor pain. A male infant was born through spontaneous vaginal delivery and his expected Ballard score was GA 40 weeks.
On neonatal intensive care unit admission, the baby showed a heart rate of 113 bpm, respiratory rate of 61 bpm, blood pressure of 65/35 mmHg, and body temperature of 36.6℃, with mild chest retraction. Body profile measurements included birth weight 3,160 g (25-50th percentile), height 49 cm (50-75th percentile), and head circumference 32 cm (10-25th percentile). His skull was not palpable over the frontal, temporal, parietal, and occipital areas, and these clinical findings were confirmed on skull radiography (Fig. 1A). A brain computed tomography (CT) scan showed a membranous neurocranium, but with under-developed ossification (Fig. 2). A neurosurgeon recommended using a helmet to avoid trauma, but the mother was unable to comply due to economic problems.
Spontaneous and mild pneumothorax but no lung hypoplasia was seen on the chest radiography and respiratory distress was treated by noninvasive respiratory support for 2 days (Fig. 3). Urine output was fair, but hyponatremia (Na 133 mmol/L), elevated blood urea nitrogen (38.75 mg/dL), elevated creatinine (1.05 mg/dL), and mild metabolic acidosis (capillary blood gas analysis; pH 7.311, pCO2 29.3 mmHg, pO2 67 mmHg, HCO3 14.8 mmol/L, BE –11 mmol/L) were observed. Proteinuria was also noted (spot urine protein/creatinine ratio=9.17). Sonographic examination revealed the kidneys to be increased in size and increased renal cortical echogenicity. The laboratory and image findings suggested parenchymal renal disease. After conservative management such as oral sodium and sodium bicarbonate replacement, the laboratory test results had improved.
Because IVC thrombosis was detected accidently by abdominal ultrasonography, abdominal CT and inferior vena cavography was performed. The common iliac vein was not observed and the IVC was completely obstructed, and therefore all of the venous flow from the lower extremities was draining to the azygos vein through collateral vessels to the superior vena cava (Fig. 4). Owing to his asymptomatic status and the conrisks associated with treatment of thromboembolism, we decided to closely observe the patient rather than actively treating his IVC thrombosis.
Following conservative management and observation for 2 months, his skull bones were noted to be fully developed (Fig. 1B), and he showed correction of his abnormal laboratory findings. The patient continued to visit the outpatient clinic in our hospital for periodic re-evaluation of his kidney function and IVC thrombosis. It should be noted that he was asymptomatic and his laboratory findings had become normal. However, increased renal cortical echogenicity and IVC thrombosis continued. His body profile measurements at his 24 months' of age were weight 9.7 kg (<3rd percentile), height 81.8 cm (5th percentile), and head circumference 46.5 cm (5-10th percentile). On the Korean Development Screening Test for Infants & Children (K-DST), his development was generally delayed for his age.
ARBs are contraindicated drugs during pregnancy because of their potential fetotoxicity. They are known to reduce fetal renal blood flow and cause ischemic kidney injury, such as renal tubular dysgenesis, anuria, oligohydramnios, and anhydramnios.5 Anuria-associated oligohydramnios may cause fetal limb contractures, craniofacial deformation, and pulmonary hypoplasia.7 Barr and Cohen6 found possible links between calvarial underdevelopment, especially the membranous skull bones, and renal tubular dysgenesis. They suggested that this “kidney-skull connection” caused by angiotensin converting enzyme (ACE) inhibition may be due to intrauterine hypotension and/or chronic hypoxia. Hypocalvaria can be secondary to poor perfusion of plate-like bone structures in the skull.
For other cases of exposure to ACE inhibitors or ARBs during the second and third trimesters of pregnancy, complications such as oligohydramnios, renal failure, neonatal hypotension, bony deformity, and skull ossification defects have been reported. Also, limb contracture, patent ductus arteriosus, respiratory distress syndrome, lung hypoplasia and apnea, and even in utero death have been seen. In most cases, treatment was conservative therapy for each symptom.8
In our case, the fetus was exposed to ARBs throughout the pregnancy, and the newborn showed various ARB-related symptoms, such as skull ossification defects, pneumothorax, respiratory distress, and renal parenchymal disease. His congenital calcaneovalgus foot, which was not reported in previous cases, is thought to result from oligohydramnios due to ARB use during pregnancy. These suggest that maternal use of ARBs throughout pregnancy has a significantly large effect on fetal development. Although the IVC thrombosis confirmed by abdominal CT is thought to be unrelated to ARB use, further studies are needed to determine the association between IVC thrombosis and the use of ARBs.
Although these fetotoxic effects of ARBs are well known and several cases of hypocalvaria have been reported, the distinctiveness of our study was the imaging we performed. Ours was the first case in which hypocalvaria in the patient was confirmed using a skull CT, that was further reconstructed using 3-dimensional graphics.
Usually, physicians educate pregnant women to discontinue the use of ARBs when pregnancy is confirmed. However, in our case, the fetus was exposed to ARBs throughout pregnancy. Both his parents had moderate mental retardation, and were not aware of the patient's mother's pregnancy. She therefore continued the use of antihypertensive drugs including valsartan (an ARB). They were economically disadvantaged. With limited-to-no knowledge about medical care, they were easily exposed to the risks of an unplanned pregnancy and did not seek medical attention during the mother's pregnancy. The patient's mother received medical treatment at a clinic for hypertension through a drug prescription, but her physician did not recognize her pregnancy. Physicians need to reflect on the fact that this unfortunate event happened in a medically advanced country like Korea, and therefore they need to obtain a careful and detailed medical history while treating vulnerable classes, such as the disabled and economically disadvantaged young adults.
Because the sexuality of disabled women is suppressed socially, sex education provided to them is limited. Therefore, it is necessary to accept the sexual and reproductive needs of disabled women and provide comprehensive sex education. ccording to the ‘Research on Pregnancy and Childbirth Support Policy for the Promotion of Maternal Rights for Women with Disabilities’,9 intellectually disabled women have low understanding of books on sex education, pregnancy, and childbirth, and have limited understanding of the content of the medical consultations. Therefore, it is necessary to develop an easy-to-read book that meets the needs of women with intellectual disabilities, and additional customized education is needed to achieve a clear understanding on their part.
In addition, it has been identified that the average number of women accessing antenatal care among the intellectually disabled women is less than that in the general population in Korea.9 This is thought to be due to a lack of understanding of the importance of antenatal care and economic difficulties.
In the UK, a ‘midwife system’ is used for antenatal care at the national level for every woman, and if additional care is required, such as for maternal complications or disability, a more specialized medical system consisting of an obstetrician and other physicians is available. In this way, advanced countries have well-equipped human resources and economic support systems for vulnerable women, and Korea needs to move in the right direction.
At the age of the infant was 24 months, weight, height, and head circumference of the patient were all below the 10th percentile, and overall developmental delay was evident on the K-DST. It is unclear whether this is a genetic effect, a drug effect, or an effect of inadequate parenting.
In conclusion, it is our opinion that greater attention, sex education, and protection of the socially vulnerable women are needed at the individual physician level and at the national level. Also, attention needs to be directed not only toward antenatal consultations during pregnancy but also towards proper child rearing by intellectually disabled women.
Figures and Tables
Fig. 1
Left lateral plain skull radiograph. (A) Poor ossification of frontal, temporal, parietal, and occipital bones at birth. (B) Fully developed skull bones at 2 months' of age.
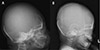
Fig. 2
Three-dimensional computed tomography volume rendering images of the skull showing poor ossification of the frontal, temporal, parietal, and occipital bones. Wide cranial sutures are noted.

References
1. Diav-Citrin O, Shechtman S, Halberstadt Y, Finkel-Pekarsky V, Wajnberg R, Arnon J, et al. Pregnancy outcome after in utero exposure to angiotensin converting enzyme inhibitors or angiotensin receptor blockers. Reprod Toxicol. 2011; 31:540–545.

2. Pryde PG, Sedman AB, Nugent CE, Barr M Jr. Angiotensin-converting enzyme inhibitor fetopathy. J Am Soc Nephrol. 1993; 3:1575–1582.

3. Easterling TR, Carr DB, Davis C, Diederichs C, Brateng DA, Schmucker B. Low-dose, short-acting, angiotensin-converting enzyme inhibitors as rescue therapy in pregnancy. Obstet Gynecol. 2000; 96:956–961.

4. Boix E, Zapater P, Picó A, Moreno O. Teratogenicity with angiotensin II receptor antagonists in pregnancy. J Endocrinol Invest. 2005; 28:1029–1031.

5. Barr M Jr. Teratogen update: angiotensin-converting enzyme inhibitors. Teratology. 1994; 50:399–409.

6. Barr M Jr, Cohen MM Jr. ACE inhibitor fetopathy and hypocalvaria: the kidney-skull connection. Teratology. 1991; 44:485–495.

7. Schaefer C. Angiotensin II-receptor-antagonists: further evidence of fetotoxicity but not teratogenicity. Birth Defects Res A Clin Mol Teratol. 2003; 67:591–594.

8. Shotan A, Widerhorn J, Hurst A, Elkayam U. Risks of angiotensin-converting enzyme inhibition during pregnancy: experimental and clinical evidence, potential mechanisms, and recommendations for use. Am J Med. 1994; 96:451–456.

9. Seo HJ, Bae SH, Lee KM. Research on pregnancy and childbirth support policy for the promotion of maternal rights for women with disabilities. Korea: Korea Disabled People's Development Institute;2016.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download