Abstract
The neonatal mortality rate has been consistently maintained at 1.1 deaths per 1,000 live births in Japan, which is the lowest level in the world. In addition, long-term survival and prognosis of extremely preterm infants, including neonates born at 22-23 weeks of gestation, has continued to improve. In order to provide high-quality medical care, we had constructed a perinatal transport network, 104 Level 3 perinatal centers, and 292 Level 2 perinatal centers as of 2016. To make additional progress in improving outcomes for high-risk infants, we developed a research database system, ‘Neonatal Research Network Japan (NRNJ)’ in 2003. Analysis through this database system enables comparison between various randomized controlled trials, domestically and internationally. To improve quality of care at neonatal intensive care units (NICU), we developed another unique project “INTACT” (Improvement of NICU Practice & Team Approach Cluster-Randomized controlled Trial) in 2011. In this project, we aim to correct the disparity in clinical skills, techniques, and knowledge which exists between facilities, and provide a more equalized, high-quality standard of neonatal care. The neonatal cardiopulmonary resuscitation (NCPR) training program is another strategy which helps maintain our clinical quality. With these challenges, (NRN database, INTACT RC traial, and NCPR program), we will strive towards reaching our goal of “intact survival” of all newborn babies.
The annual number of live births in Japan has gradually decreased to around one million. However, the percentage of neonates born at high-risk of mortality has been increasing. Notably, recent trends show a higher proportion of low-birth-weight infants (LBWI) at 9.6% of all births (in 2015).1 This poses serious problems from both the short- and long-term perspectives, especially when considering the developmental origins of health and disease (DOHaD) theory. In contrast to Japan, only 5.5% of children born in Korea are classified as LBWI.1 Several factors are thought responsible for the higher rate of LBWI in Japan, including the typically higher age at which mothers give birth for the first time.
On the other hand, the survival rate of high-risk infants has markedly improved in our country. The neonatal mortality rate has been consistently maintained at 1.1 deaths per 1,000 live births, which is the lowest level in the world. In addition, the long-term survival and the prognosis of extremely preterm infants, including neonates born at 22-23 weeks of gestation,2 have continued to improve. In order to provide high-quality medical care, the perinatal transport network was established in 1996, which includes 104 Level 3 perinatal centers, and 292 Level 2 perinatal centers, and NICU beds served approximately 30 per 10,000 births as of 2016.
To further advance the practice of neonatal medicine, we developed a strategy based on three aspects, “Research”, “Clinical Medicine”, and “Education”. To promote the research, we built a neonatal database. To improve the clinical medicine, we designed a quality improvement program. To broaden the education, we established a neonatal cardiopulmonary resuscitation training program.
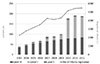
To make additional progress in improving outcomes for high-risk infants, in 2003 we developed a research database system, Neonatal Research Network Japan (NRNJ). The database of the NRNJ provides a wealth of information, including data on mortality, morbidity, perinatal factors, and outcomes at 1.5 and 3 years of age in very-low-birth-weight infants (VLBWI). Analysis using the information in this database system enables comparisons between various randomized controlled trials (RCTs), domestically and internationally. The number of facilities and registered infants in this database has been increasing, currently, more than 200 facilities participate and 4,000 infants are registered (Fig. 1). In this database, more than 70% of VLBWI born in Japan are covered. We have analyzed the outcome data concerning VLBWI and preterm infants, and more than 20 papers have been published including reports on RCTs.4 For international comparisons, the NRNJ is participating in the International Network for Evaluation (iNeo).5 iNeo stands for “International Network for Evaluation of Outcome of Neonates”. This is a quality improvement project that engages in collaborative comparisons of population-based international health services for neonatal care.
To improve the quality of NICU care, in 2011 we developed another unique project: the Improvement of NICU practice and Team Approach Cluster-Randomized controlled Trial (INTACT). This project aims to correct the disparity in clinical skills, techniques, and knowledge that exists between facilities and to provide a more equalized, high-quality standard of neonatal care.
INTACT is a cluster RCT for the evaluation of the specific intervention program. This program, the Quality Improvement Program on Neonatal Care (QIPNC) consists of four processes, “Facility profiling”, “Action Plan”, “Onsite Workshops”, and “Monitoring of the Progress”. In the facility-profiling process, we profile the strengths and weaknesses of the hospitals and provide feedback. In the action plan step, we develop and implement the effective action plans. In the onsite workshops area, we hold the educational workshops and give presentations on clinical practice guidelines. Finally, in the monitoring of progress step, we audit the status of the action plans and provide advice. This trial started in 2011 and the results will become available in 2017.
The neonatal cardiopulmonary resuscitation (NCPR) training program is based on the guidelines of the International Liaison Committee on Resuscitation (ILCOR) is another strategy that helps maintain our clinical quality. The NCPR project, which was launched in 2007 and encompasses 21 core training centers in the nation to date, has already organized more than 7,700 seminars and has awarded certificates to 60,000 participants. There are several factors that have allowed the NCPR program to spread nationwide throughout Japan. First, the establishment of training sites at 21 locations throughout the country allows neonatal care professionals to participate in the program at a location that is as close to their place of work as possible. The training sites mainly train instructors. By having instructors in each region, a variety of courses can now be held nationwide. Furthermore, in addition to offering a choice of courses tailored to individual proficiency levels, other resources are provided, including self-taught e-learning and the ability to improve skills through follow-up courses have been provided. Additional resources, such as the sale of standard textbooks and DVDs, rental of materials, and an instructor registration and dispatch system, support the project, which allows this program to spread.
Evidence regarding neonatal resuscitation practices is being transmitted worldwide from Japan. In particular, umbilical cord milking for preterm infants, which has been promoted primarily by Professor Hosono et al., is also being cited in international research reports.7 In the ILCOR resuscitation recommendations revised in 2010, therapeutic hypothermia is described as the standard treatment for moderate to severe neonatal hypoxic ischemic encephalopathy (HIE). In 2010, sufficient evidence did not exist concerning the neuroprotective effects of therapeutic hypothermia. To establish the evidence and facilitate improvements in indication criteria, cooling methods and combination therapies, a national registry of hypothermia therapy for neonatal encephalopathy was established. Data analysis during the first three years of the registry demonstrated that the mortality rate of neonates who underwent cooling was considerably lower than that reported in previous studies.8 The mission of the NCPR project is that “staff who acquire the neonatal resuscitation technique should attend all deliveries in their role as a newborn care staff.” Nationwide implementation of this project and its continuation are quite important to ensure safe deliveries in Japan, where a declining birth rate has been an issue. In 2015, a system overhaul was undertaken, which included shortening the certification period.
In addressing these challenges, we strive towards reaching our goal of “intact survival” of all newborn babies. Research, quality improvement and education are vital to reaching this goal. International cooperation will also become increasingly important.
Figures and Tables
Acknowledgements
The author is grateful to all members involved in the NRNJ, INTACT and NCPR program in JAPAN.
References
1. Health at Glance 2015 OECD Indicators. accessed on 20 January 2017. Available at http://www.oecd.org/health/health-systems/health-at-a-glance-19991312.htm.
2. Ishii N, Kono Y, Yonemoto N, Kusuda S, Fujimura M;, Japan . Outcomes of infants born at 22 and 23 weeks’ gestation. Pediatrics. 2013; 132:62–71.

3. Neonatal Research Network Database Japan (in English). accessed on 20 January 2017. Available at http://plaza.umin.ac.jp/nrndata/indexe.htm.
4. Nakamura T, Yonemoto N, Nakayama M, Hirano S, Aotani H, Kusuda S, et al. Early inhaled steroid use in extremely low birth weight infants: a randomized controlled trial. Arch Dis Child Fetal Neonatal Ed. 2016; F1–FF.
5. Shah PS, Lui K, Sjörs G, Mirea L, Reichman B, Adams M, et al. Neonatal Outcomes of Very Low Birth Weight and Very Preterm Neonates: An International Comparison. J Pediatr. 2016; 177:144–152.
6. Neonatal Cardio-Pulmonary resuscitation. Japan Society of Perinatal and Neonatal Medicine (in Japanese). accessed on 20 January 2017. Available at http://www.ncpr.jp/.
7. Ghavam S, Batra D, Mercer J, Kugelman A, Hosono S, Oh W, et al. Effect of placental transfusion in extremely low birth weight infants: meta-analysis of long-and short-term outcomes. Transfusion. 2014; 54:1192–1192.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download