Abstract
A female was born at 36+5 weeks of gestation with a birth weight of 2,120 g. Apgar score was 7 at 1 minute and 9 at 5 minutes. Shortly after birth, tachypnea, chest retraction, and a severe build-up of oral secretions were noted. Her blood type was A+ and initial hemoglobin was 17.5 g/dl. Her mother was A+ blood type. Ampicillin/Sulbactam and gentamicin were started empirically. At 8th day of admission, laboratory results showed hemolytic anemia. Exchange transfusion was performed along with intravenous immunoglobulin and hydrocortisone. After 2 days, the patient's clinical and laboratory conditions improved. Column hemagglutination assay revealed that the patient's hemolysis was due to ampicillin/sulbactam.
Drug-induced immune hemolytic anemia (DIIHA) is rare, with the incidence estimated to be approximately one in 1 million, although exact data are lacking.1 The incidences of drug-induced immune thrombocytopenia and neutropenia are approximately 10-18 and 2-15 cases per million, respectively.2
Limited data are available about DIIHA in a premature infant, whose immune system is immature and not fully functional. Here, we report the case of a preterm infant who presented with severe anemia and jaundice one to two days following prophylactic administration of ampicillin/sulbactam after a tracheoesophageal fistula operation. DIIHA was diagnosed by a column hemagglutination assay and the infant was treated by exchange transfusion.
A female second born twin was born at 36+5 weeks of gestation with a birth weight of 2,120 g by Cesarean section at a local clinic. The patient's Apgar score was 7 at 1 minute and 9 at 5 minutes. Shortly after birth, tachypnea, chest retraction, and a severe build-up of oral secretions were noted. An orogastric tube could not be advanced, and the initial chest radiograph revealed that the orogastric tube was coiled, suggesting a Tracheoesophageal fistula with esophageal atresia. The patient was then referred to our neonatal intensive care unit for surgery. Her blood type was A+ and initial hemoglobin was 17.5 g/dl. TORCH and Tandem mass screening tests were within normal limits. Her mother was a 32-year-old gravida 1 para 0 woman, with preterm labor, who had A+ blood type and had received dexamethasone two times, but no antibiotics, prior to delivery.
Ampicillin/sulbactam (Ubacillin®, 120 mg/kg/day, intravenously) and gentamicin (8 mg/kg/day, intravenously) were started empirically and prophylactically in preparation for surgery on the first day of life. Although the operation to repair the fistula (Tracheoesophageal fistulization) was successful, the patient's hemoglobin level decreased and indirect/direct hyperbilirubinemia increased, first gradually and then dramatically (Hemoglobin: 18.2, 16.9 and 10.6 g/dL at 1st, 2nd and 5th day of life; Total bilirubin: 7.7 and 24 mg/dL at 2nd and 5th day of life). However, the results of direct/indirect Coombs tests were negative. Despite packed red blood cell (RBC) transfusion and intensive phototherapy, the patient's condition continued to worsen and seizures were observed at 6th day of life.
At that time, the patient's C-reactive protein (CRP) levels increased to 3.6 mg/dL (Normal range, <0.3). The antibiotics were then changed to vancomycin (20 mg/kg/day) and amikacin (13 mg/kg/day). Other laboratory studies revealed the following: hemoglobin 5 g/dL, hematocrit 14.3%, MCV/MCH/MCHC 94.7 fl/33.1 pg/35.0%, reticulocyte count 30.71%, total bilirubin 40.5 mg/dL, direct bilirubin 22.4 mg/dL, increased urobilinogen, urinary occult blood 3+, urine RBC 1-4/HPF, and negative direct/indirect Coombs tests. Peripheral blood smear showed anisocytosis 2+ and poikilocytosis 2+. The patient also demonstrated frequent oxygen desaturation and bradycardia that required mechanical ventilation. The seizure was probably due to kernicterus or hypoxia induced by acute decrease of hemoglobin, but the exchange transfusion was delayed because the patient showed melena. On the eight day of life, after improvement of melena, it was decided to perform an exchange transfusion (using twice the baby's blood volume) with a mixture of O+ RBCs and AB+ fresh frozen plasma along with intravenous immunoglobulin (IVIG, 500 mg/kg/day, 2 day course) and Hydrocortisone(Solu-cortef®, 1 mg/kg, 2 day course). On the ninth day, a further RBC transfusion was given along with testing for glucose-6 phosphate dehydrogenase (G-6-PD) deficiency, which was negative.
From the tenth day of life, 2 days following the exchange transfusion, the patient's clinical and laboratory conditions improved. She did not require further transfusion and was discharged from the hospital on the 25th day of life. Before discharge, we performed brain MRI and it showed signs of acute kernicterus as we expected. A brief clinical course, as well as the patient's hemoglobin and bilirubin levels, are presented in Fig. 1.
At discharge, her hematologic and bilirubin values were: hemoglobin, 12.6 g/dL; hematocrit, 36.9%; reticulocyte, 2.5%; total bilirubin, 2.8 mg/dL; and direct bilirubin, 2.3 mg/dL. The patient's clinical and laboratory stabilization was continued with close follow-up in the outpatient setting.
To clarify the mechanism of her aggressive hemolysis, a column hemagglutination assay (Ortho Diagnostics, Raritan, NJ, USA) was performed twice, using the patient's RBC and serum collected on the 15th and 50th days of life. The patient's sera were not reactive against untreated RBCs in the presence of vancomycin and ampicillin/sulbactam. The patient's serum obtained on the 15th day of age was strongly reactive with ampicillin/sulbactam-coated RBCs, which were obtained on the 50th day of life and treated with ampicillin/sulbactam for 30 minutes. However, this positive control serum was not reactive with ampicillin/sulbactam-coated RBCs from other donors (Fig. 2). Strangely, reactivity was weakly positive between ampicillin/sulbactam-coated RBCs from the patient (15th day of life) and the patient's serum (15th day of life) (+1). Moreover, ampicillin/sulbactam-coated RBCs (50th day of life) did not react with the patient's serum from the 50th day of life. RBCs treated with vancomycin were nonreactive after incubation with the patient's sera. In conclusion, these results suggested that our patient's hemolysis was induced by ampicillin/sulbactam.
DIIHA is a rare and serious adverse reaction that may result from drug administration.234567 The most common drugs associated with DIIHA and the potential mechanisms thought to be involved have changed over the last few decades.2 Both ampicillin and sulbactam contained in ampicillin/sulbactam accounted for 1.3 to 23% of reported cases of DIIHA.2
Suggested mechanisms involved in drug-induced immune hemolytic anemia are summarized as follows; (1) Drug-dependent antibodies will only react in vitro in the presence of the drug.2 Most penicillins and cephalosporins are capable of covalently bonding to proteins on RBC membranes, providing drug-coated RBCs for detection of certain drug antibodies in vitro.28 (2) The majority of drugs that cause acute, severe, intravascular hemolysis, and sometimes disseminated intravascular coagulation and death, seem to be involved in the so-called immune complex mechanism.9 (3) Drug-independent antibodies can be detected in vitro without adding any drug; thus, in vitro and in vivo characteristics are identical to those of RBC autoantibodies that are antibodies to the carrier protein alone.8 (4) Recently, Garratty et al. reported a "unifying hypothesis" for DIIHA that provided a model for all three types of drug antibodies.12 If drug is bound to protein on RBCs, three populations of antibodies might be found; hapten (drug), combination of hapten plus carrier protein epitopes, and carrier protein.2 (5) Another new concept, non-immune protein adsorption (NIPA), has drawn increasing interest.1011 Some drugs (β-lactamase inhibitors; sulbactam, clavulanate, and tazobactam) appear to be capable of modifying RBC membrane so that proteins (IgG, complement, albumin, and fibrinogen, among others) become non-immunologically adsorbed onto the RBC membrane.21011
In our case, hemolytic anemia developed after the use of ampicillin/sulbactam. Moreover, when ampicillin/sulbactam administration was discontinued and exchange transfusion was performed, the hemolytic anemia soon resolved. Eventually, this peculiar remission after discontinuing ampicillin/sulbactam, and ampicillin/sulbactam - coated RBC reactivity, supported the diagnosis of drug - induced hemolytic anemia. The weak positive result on the 15th day of life, as detected by a column hemagglutination assay, may have been due to dilution of the patient's RBCs by packed RBCs used in the exchange transfusion. The non-reactivity of the patient's serum obtained from the 50th day of life may be secondary to the short half-life and deficit of the absolute amount of IgG, and the concentration of IgG that falls postnatally in preterm infants.
Among above several possible mechanisms of hemolysis, drug (hapten) adsorption or drug adsorption type in "unifying mechanism" in relation to ampicillin is considered a possible mechanism in the current case. In our column hemagglutination assay, we found negative reactivity with simultaneous mixture of the patient's and donor RBCs, serum, and the drug, which suggested that an immune complex mechanism could be excluded. However, we did not obtain laboratory confirmation of such an effect due to sulbactam (β-lactamase inhibitor), which is a component of ampicillin/sulbactam and might induce non-immune protein adsorption (NIPA). Hemolysis induced by β-lactamase inhibitor-containing drugs has been proven to have a high incidence of a positive direct Coombs test.1011
In drug-induced immune hemolysis, positivity of the direct Coombs test is usually high.1213 Weaker positive direct Coombs tests are seen when the patient is off the drug for some time. The negative results in our patient may have been due to a weakening effect of the transfused blood product, IVIG, or due to late sampling time after discontinuation of the ampicillin/sulbactam, at which time the drug-coated RBCs were mostly destroyed. Similarly, Arndt et al. reported that the strength of the direct Coombs test varied from 4+ to weak+ in second- and third-generation cephalosporin associated immune hemolytic anemia.14
In summary, we conclude that the severe anemia and jaundice in this patient were due to ampicillin/sulbactam-induced hemolysis, based on the fact that the patient's serum was strongly reactive with the patient's own RBCs coated with ampicillin/sulbactam. This diagnosis was confirmed by a column hemagglutination assay.
Figures and Tables
Fig. 1
The pattern of hemoglobin and bilirubin levels according to antibiotics and other treatments. Abbreviations: Amp, ampicillin; Hb, hemoglobin (g/dL); TB, total bilirubin (mg/dL); DB, direct bilirubin (mg/dL); Reti, reticulocyte (%); IVIG, intravenous immunoglobulin; RBC, packed red blood cell transfusion; ExTF, exchange transfusion.

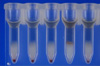
Fig. 2
The detection of RBC antibody in patient's serum. The patient's serum was obtained on the 15th day of age and the patient's RBC on the 50th day of age respectively. The serum was reactive with the patient's RBC coated with ampicillin/sulbactam. A(negative)=patient's RBC+patient's serum+ampicillin/sulbactam; B (negative)=type O blood donor 1's RBC+patient's serum+ampicillin/sulbactam; C (negative)=type O blood donor 2's RBC+patient's serum+ampicillin/sulbactam; D (4+ positive) =ampicillin/sulbactam-coated patient's RBC+patient's serum; E (negative)=ampicillin/sulbactam-coated type O blood donor 1's RBC+patient's serum; F (negative)=Ampicillin/sulbactam-coated type O blood donor 2's RBC+patient's serum.
Acknowlegement
This work was supported by the research fund of Hanyang University (HY-2008-000-0000-8123).
References
1. Arndt PA, Garratty G. The changing spectrum of drug-induced immune hemolytic anemia. Semin Hematol. 2005; 42:137–144.

2. Garratty G. Drug-induced immune hemolytic anemia. Hematology Am Soc Hematol Educ Program. 2009; 73–79.

4. Baek EJ, Lee S, Kim S, Choi HK, Kim HO. A case of immune hemolytic anemia induced by ceftizoxime and cefobactam (sulbactam/cefoperazone). Korean J Lab Med. 2009; 29:578–584.

5. Rao KV. Drug-Induced Hematologic Disorders. In : DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey L, editors. Pharmacotherapy: a pathophysiologic approach. 9th ed. New York: McGraw-Hill;2014. p. 647–661.
6. Mintzer DM, Billet SN, Chmielewski L. Drug-induced hematologic syndromes. Adv Hematol [serial online];2009. 01-12. 01(01):[24screens]. cited 2009 Jul. Available fromhttps://www.hindawi.com/journals/ah.
7. Claas FH. Immune mechanisms leading to drug-induced blood dyscrasias. Eur J Haematol Suppl. 1996; 60:64–68.

9. Mayer B, Yurek S, Salama A. Piperacillin-induced immune hemolysis: new cases and a concise review of the literature. Transfusion. 2010; 50:1135–1138.

10. Garratty G, Arndt PA. Positive direct antiglobulin tests and haemolytic anaemia following therapy with beta-lactamase inhibitor containing drugs may be associated with nonimmunologic adsorption of protein onto red blood cells. Br J Haematol. 1998; 100:777–783.

11. Leger RM, Arndt PA, Garratty G. Serological studies of piperacillin antibodies. Transfusion. 2008; 48:2429–2434.

12. Johnson ST, Fueger JT, Gottschall JL. One center's experience: the serology and drugs associated with drug-induced immune hemolytic anemia--a new paradigm. Transfusion. 2007; 47:697–702.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download