Abstract
Purpose
The objective of this study was to determine factors associated with respiratory insufficiency and long term ventilator-support in newborn with omphalocele.
Methods
Medical records of neonates with omphalocele in the neonatal intensive care unit (NICU) in Seoul National University Children's Hospital between April 2000 and March 2016 were reviewed retrospectively.
Results
A total of 44 neonates were enrolled. Infants intubated within 24 hours after birth (early intubated group, n=21) and not intubated within 24 hours after birth (late intubated group n=23) were compared. Duration of ventilator care, duration of total parenteral nutrition administration, duration of NICU stay and mortality rate were higher in the early intubated group. The early intubated group had lower gestational age, lower birth weight, lower 1min and 5min Apgar score and higher mortality rate with longer duration of mechanical ventilator support than late intubated group. Persistent pulmonary hypertension and small for gestational age were related to the duration of ventilator support.
Conclusion
It is important to predict and prevent of respiratory insufficiency and prolongation of invasive mechanical ventilation in neonates with omphalocele. It is needed to diagnose pulmonary hypertension and respiratory failure after birth in early stages. Further prospective large cohort studies are needed to determine the pathophysiology of respiratory insufficiency and ventilator dependency of neonates with omphalocele reducing morbidity.
Figures and Tables
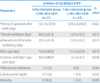
Table 1
Demographics of Study Population

Table 2
Clinical Courses of Study Population
References
1. Benjamin B, Wilson GN. Anomalies associated with gastroschisis and omphalocele: analysis of 2825 cases from the Texas Birth Defects Registry. J Pediatr Surg. 2014; 49:514–519.

2. Biard JM, Wilson RD, Johnson MP, Hedrick HL, Schwarz U, Flake AW, et al. Prenatally diagnosed giant omphaloceles: short- and long-term outcomes. Prenat Diagn. 2004; 24:434–439.

3. Christison-Lagay ER, Kelleher CM, Langer JC. Neonatal abdominal wall defects. Semin Fetal Neonatal Med. 2011; 16:164–172.

4. Hershenson MB, Brouillette RT, Klemka L, Raffensperger JD, Poznanski AK, Hunt CE. Respiratory insufficiency in newborns with abdominal wall defects. J Pediatr Surg. 1985; 20:348–353.

5. Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM. CDC definitions for nosocomial infections, 1988. Am J Infect Control. 1988; 16:128–140.

6. Tassin M, Descriaud C, Elie C, Houfflin Debarge V, Dumez Y, Perrotin F, et al. Omphalocele in the first trimester: prediction of perinatal outcome. Prenat Diagn. 2013; 33:497–501.

7. Corey KM, Hornik CP, Laughon MM, McHutchison K, Clark RH, Smith PB. Frequency of anomalies and hospital outcomes in infants with gastroschisis and omphalocele. Early Hum Dev. 2014; 90:421–424.

8. Edwards EA, Broome S, Green S, Douglas C, McCall E, Nuthall G, et al. Long-term respiratory support in children with giant omphalocele. Anaesth Intensive Care. 2007; 35:94–98.

9. Ein SH, Rubin SZ. Gastroschisis: primary closure or Silon pouch. J Pediatr Surg. 1980; 15:549–552.

10. Frolov P, Alali J, Klein MD. Clinical risk factors for gastroschisis and omphalocele in humans: a review of the literature. Pediatr Surg Int. 2010; 26:1135–1148.

11. Henrich K, Huemmer HP, Reingruber B, Weber PG. Gastroschisis and omphalocele: treatments and long-term outcomes. Pediatr Surg Int. 2008; 24:167–173.

14. Kitchanan S, Patole SK, Muller R, Whitehall JS. Neonatal outcome of gastroschisis and exomphalos: a 10-year review. J Paediatr Child Health. 2000; 36:428–430.

15. Mann S, Blinman TA, Douglas Wilson R. Prenatal and postnatal management of omphalocele. Prenat Diagn. 2008; 28:626–632.

16. McNair C, Hawes J, Urquhart H. Caring for the newborn with an omphalocele. Neonatal Netw. 2006; 25:319–327.

17. Mitanchez D, Walter-Nicolet E, Humblot A, Rousseau V, Revillon Y, Hubert P. Neonatal care in patients with giant ompholocele: arduous management but favorable outcomes. J Pediatr Surg. 2010; 45:1727–1733.

18. Panitch HB. Pulmonary complications of abdominal wall defects. Paediatr Respir Rev. 2015; 16:11–17.

19. Stoll C, Alembik Y, Dott B, Roth MP. Risk factors in congenital abdominal wall defects (omphalocele and gastroschisi): a study in a series of 265,858 consecutive births. Ann Genet. 2001; 44:201–208.
20. Stoll C, Alembik Y, Dott B, Roth MP. Omphalocele and gastroschisis and associated malformations. Am J Med Genet A. 2008; 146A:1280–1285.

21. Towne BH, Peters G, Chang JH. The problem of "giant" omphalocele. J Pediatr Surg. 1980; 15:543–548.

22. Tsakayannis DE, Zurakowski D, Lillehei CW. Respiratory insufficiency at birth: a predictor of mortality for infants with omphalocele. J Pediatr Surg. 1996; 31:1088–1090.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download