Abstract
Purpose
Extraosseous Ewing's sarcoma (EOE) of the rectum is extremely rare: only three cases have been reported in the literature and none of these reports described their imaging findings in detail. Herein, we describe the tumor imaging and pathological features in detail.
Materials and Methods
We report a case of rectal EOE in a 72-year-old female who received local excision and was provisionally diagnosed with a rectal submucosal spindle cell tumor. We used immunohistochemistry, histopathology, and fluorescence in situ hybridization to characterize the tumor and provide a definitive diagnosis of EOE.
Results
MRI revealed a well-demarcated submucosal tumor with heterogeneous enhancement and hemorrhagic foci in rectum. EOE was diagnosed by positive staining of tumor cells for CD99 and Fli-1 by immunohistochemistry and the presence of the EWSR1 gene translocation by fluorescence in situ hybridization. Although the patient underwent radiation treatment and surgery, the tumor recurred after 4 months as revealed by computed tomography and magnetic resonance imaging.
Ewing's sarcoma is a relatively rare, small round cell sarcoma that shows unique molecular findings and various degrees of neuroectodermal differentiation (1). It arises in the bones most frequently, but approximately 10-20% of cases are extraskeletal (1). EOE most commonly occurs in children and young adults and typically involves the extremities, paravertebral region, retroperitoneum, and chest wall (2). To the best of our knowledge, only three cases of EOE arising from the rectum have been reported in the literature (3). However, the imaging features of the tumors were not well described. In the current study, we report an EOE case that presented as a rectal submucosal tumor, and describe the imaging and pathologic findings in detail. This study was approved by the Institutional Review Board of our institution and a waiver of informed consent was obtained.
A 72-year-old woman was referred to our institution for further treatment of a rectal submucosal tumor after local excision. Initially, colonoscopy (Fig. 1) and rectal MRI (Fig. 2) at the outside clinic demonstrated a subepithelial tumor measuring approximately 4 cm in the lower rectum. The mass was well-demarcated and showed heterogeneous enhancement. A focal hemorrhage was suspected at the rectal luminal surface. The initial differential diagnosis included gastrointestinal stromal tumor, neuroendocrine tumor and leiomyoma. Transanal local excision was performed at the outside clinic and microscopic examination revealed a malignant spindle cell tumor (Fig. 3a), although a specific diagnosis was not reached. Additional analysis of the surgical specimen was performed at our institution. Immunohistochemistry demonstrated cytoplasmic membrane-positive CD99 and nucleus-positive Fli-1 staining of the tumor cells (Fig. 3b, c). Staining for CD45, CD31, CD34, S-100, HMB-45, Melan-A, and cytokeratin (AE1/AE3) were all negative, which excluded the possibility of other malignant small round cell tumors. Fluorescence in situ hybridization using the Vysis EWSR1 Break Apart Probe Kit (Abbott Molecular, Seoul, Korea) demonstrated the EWSR1 gene translocation, which documented the pathological diagnosis of Ewing's sarcoma (Fig. 3d).
Six months after local excision, computed tomography (CT) detected a local recurrence of the tumor measuring 5.2 cm at the previous local excision site (Fig. 4a), without evidence of metastasis. Preoperative pelvic irradiation (6.5 Gy) was performed to reduce the size of the mass. The rectal magnetic resonance imaging (MRI) obtained 2 months after the completion of radiotherapy showed that the mass had decreased to a 1.8 cm-deep ulcerative lesion. The mass demonstrated markedly low T2 signal intensity (Fig. 4b), which we assumed to represent fibrotic change. Contrast enhanced T1-weighted images displayed little, if any, enhancement (Fig. 4c). Subsequent abdominoperineal resection, posterior vaginectomy, and total abdominal hysterectomy with bilateral salpingo-oophorectomy was performed, and the pathology report documented the recurrence of Ewing's sarcoma with a clear resection margin. However, a huge intraperitoneal mass was detected by CT only 4 months after surgery and subsequently patient received only supportive care.
The Ewing's family of tumors includes osseous Ewing's sarcoma, EOE, and primitive neuroectodermal tumor, which in common show densely packed, small, round blue cells without distinct cell borders upon microscopic examination (4). Positive staining for CD99 and Fli-1 proteins by immunohistochemistry are important clues for diagnosis (5). This disease entity shows the characteristic chromosomal translocation between the TET/FET (TLS/FUS, EWSR1, and TAF15) and E26 transformation-specific (ETS) gene families. In particular, the EWSR1 gene rearrangement has been reported in over 90% of Ewing's sarcoma cases (56).
EOE can arise in any location from head to toe and usually presents as a bulky mass that displaces, encases, or invades adjacent organs (4). The most commonly reported locations for EOE are the paravertebral region, lower extremities, chest wall, retroperitoneum, pelvis and hip, and upper extremities (7). The imaging features of EOE are non-specific, but bulky soft tissue masses with adjacent bony invasion can indicate the possibility of this disease entity (8).
In the abdomen, relatively frequent locations of EOE include the gall bladder, abdominal wall, rectovaginal septum, vagina, uterus, cervix, ovaries, esophagus, jejunum, ileum, common hepatic duct and pancreas (3). However, EOE arising from the rectum is extremely rare. To the best of our knowledge, only three cases of rectal Ewing's sarcoma have been reported in the literature (3), and the imaging features of the tumors were poorly described.
In the current study, we report a case of rectal Ewing's sarcoma that presented as a submucosal tumor upon colonoscopy and rectal MRI. The mass showed intermediate T2 signal intensity with suspected internal hemorrhagic foci on MRI. After contrast agent injection, the mass displayed rich but heterogeneous enhancement. Since these imaging features match with the imaging features of more prevalent tumors such as gastrointestinal stromal tumor or neuroendocrine tumor (9), it is challenging to make the accurate diagnosis based solely on the imaging features. Due to the rarity of rectal EOE, reaching the correct pathological diagnosis could also be extremely challenging even if surgical resection has been conducted. We believe that the imaging findings we report here could provide with supportive information to reach the correct diagnosis.
EOE may have distinct clinicopathological features, a higher risk of tumor recurrence, and a tendency to develop early metastasis compared to osseous Ewing's sarcoma (210). Our patient developed local tumor recurrence and abdominal metastasis shortly after local excision and abdominoperineal resection, respectively.
In conclusion, we described a case of an extremely rare EOE that arose in the rectum, and which presented as a submucosal tumor on imaging studies. Although challenging, the effort to achieve the correct diagnosis is important as EOE of the rectum has a poor prognosis and requires aggressive treatment.
Figures and Tables
 | Fig. 2Rectal MRI: (a) Precontrast T1-weighted axial image, (b) T2-weighted oblique axial image, and (c) contrast-enhanced T1-weighted axial and (d) contrast-enhanced T1-weighted coronal image revealed a well-defined submucosal mass measuring approximately 4 cm in the lower rectum. The mass (arrows) showed heterogeneous enhancement with a focal hemorrhage (arrowheads). |
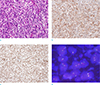 | Fig. 3Microscopic examination of the local excised specimen. (a) Hematoxylin and Eosin stain (× 200). Immunohistochemistry of (b) CD99 (× 200) and (c) Fli-1 (× 100). (d) Fluorescence in situ hybridization demonstrated the EWSR1 gene translocation, which confirmed the pathological diagnosis of Ewing's sarcoma (× 1000). |
 | Fig. 4Preoperative imaging studies of the locally recurrent mass. Comparison of (a) CT obtained when the locally recurrent mass (arrow) was detected, and (b, c) MRI obtained 2 months after pelvic irradiation indicated that the size of the mass had partially decreased after irradiation. (b) Upon T2-weighted oblique axial imaging, markedly low T2 signal intensity (black arrow) of the residual lesion suggested that extensive fibrotic change had occurred. (c) Contrast enhanced T1-weighted axial image showed minimal enhancement (white arrow) within the residual lesion. |
References
1. Fletcher CD, Bridge JA, Hogendoorn P, Mertens F. WHO classification of tumours of soft tissue and bone. 4th ed. Lyon, France: International Agency for Research on Cancer;2013.
2. Vardy J, Joshua AM, Clarke SJ, Yarrow PM, Lin BP. Small blue cell tumors of the rectum. Case 1. Ewing's sarcoma of the rectum. J Clin Oncol. 2005; 23:910–912.
3. Aboumarzouk OM, Coleman R, Goepel JR, Shorthouse AJ. PNET/Ewing's sarcoma of the rectum: a case report and review of the literature. BMJ Case Rep. 2009; 2009:pii: bcr04.2009.1770.
4. Javery O, Krajewski K, O'Regan K, et al. A to Z of extra-skeletal Ewing sarcoma family of tumors in adults: imaging features of primary disease, metastatic patterns, and treatment responses. AJR Am J Roentgenol. 2011; 197:W1015–W1022.
5. Kim SK, Park YK. Ewing sarcoma: a chronicle of molecular pathogenesis. Hum Pathol. 2016; 55:91–100.
6. Wei S, Siegal GP. Round cell tumors of bone: an update on recent molecular genetic advances. Adv Anat Pathol. 2014; 21:359–372.
7. Murphey MD, Senchak LT, Mambalam PK, Logie CI, Klassen-Fischer MK, Kransdorf MJ. From the radiologic pathology archives: ewing sarcoma family of tumors: radiologic-pathologic correlation. Radiographics. 2013; 33:803–831.
8. Huh J, Kim KW, Park SJ, et al. Imaging features of primary tumors and metastatic patterns of the extraskeletal ewing sarcoma family of tumors in adults: a 17-year experience at a single institution. Korean J Radiol. 2015; 16:783–790.
9. Kim H, Kim JH, Lim JS, et al. MRI findings of rectal submucosal tumors. Korean J Radiol. 2011; 12:487–498.
10. Angervall L, Enzinger FM. Extraskeletal neoplasm resembling Ewing's sarcoma. Cancer. 1975; 36:240–251.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download