Abstract
Schwannomas are mostly solid tumors, some of which may contain cystic degenerations or hemorrhages. However, a schwannoma seen as a purely hemorrhagic cystic tumor is very rare. A 63-year-old woman was referred to the hospital due to a slow-growing mass (present for about 5 years) on her right thigh. She complained about vague pain but without neurologic symptoms such as numbness or tingling sensations. MR images showed an oval lesion with defined margins surrounded by the rectus femoris, vastus lateral, and the vastus intermedius. It was characterized as a multilocular cystic lesion composed of hemorrhagic fluid. In addition, the benign hemorrhagic cystic lesion was differentially diagnosed by radiological techniques as a hemorrhagic ganglion cyst. The lesion was surgically excised and, based on pathological features, was diagnosed as being a schwannoma. We report a purely hemorrhagic cystic schwannoma located in an intermuscular plane.
A schwannoma is a benign peripheral nerve sheath tumor arising from Schwann cells. Most schwannomas are solid tumors and cystic degeneration and hemorrhage can be seen (1). A benign schwannoma can display degenerative changes, such as hyalinization, hemorrhaging, calcification, and cyst formation. These changes are usually partially visible in the tumors (123456). Few reports have described a purely cystic schwannoma (2457).
A 63-year-old woman was referred to our institution for a mass on the right thigh. She first noticed the mass five years prior to seeking medical assistance and reported that it had gradually increased in size during that period. The patient reported the onset of vague, mildly intense pain that had started four days prior to her visit. The patient could not recall any traumatic event prior to the onset of the symptoms. In addition, the patient did not complain of any sensory changes e.g., numbness or motor weakness, and her medical history was otherwise unremarkable.
Clinical examination revealed an oval-shaped and tender mass (dimensions of 3.0 × 4.0 cm) on the anterior aspect of the proximal thigh. The mass was firm and did not move upon palpation. No other masses were found. Initial radiographs of the hips and pelvic area demonstrated normal bone alignment without any osseous abnormalities.
Magnetic resonance imaging (MRI) demonstrated a well-defined oval cystic lesion (dimensions of 4.3 × 3.5 × 3.0 cm) in the intermuscular plane between the vastus lateralis and the vastus intermedius at the proximal one-third of the femoral level (Fig. 1a). Modified proton density images showed that the lesion was multilocular in appearance with several septa. Each one of the locules showed fluid-fluid level compatibility with its hemorrhagic content (Fig. 1a). The lesion was surrounded by a low-signal margin on the modified proton density image (Fig. 1b). The lesion was surrounded by a rim of fat (split-fat sign) on the sagittal image (Fig. 1b). The contrast-enhanced T1-weighted images showed capsular enhancements (Fig. 1c). The lesion was preoperatively identified as being a non-tumorous benign hemorrhagic cyst and this diagnosis included a description as a hemorrhagic ganglion cyst or a chronic hematoma. The diagnosis of hematoma can be ruled out due to the absence of trauma in the medical history. The first aspect of the treatment plan was surgical excision of the lesion.
The lesion was located deep in the rectus femoris muscle and could be surgically approached by opening the fascia. The mass was easily excisable. However, no nerve fibers were visibly connected to the lesion. The oval-shaped lesion dimensions were 4.5 × 3.0 × 2.5 cm (Fig. 2a). Additionally, the gross anatomy of the lesion could be described in terms of being covered by a yellow-tinged grayish capsule. The inner surface of the cystic lesion had a brown appearance and the lesion contained a reddish hematoma. The tumor did not appear to have any solid components (Fig. 2b).
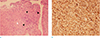
The pathological features of the lesion was consistent with that of a neurogenic tumor, schwannoma. Antoni A regions were punctuated by nuclei arranged in stacked alignments known as palisades (Fig. 3a). The tightly organized Antoni A regions intermingled with the Antoni B regions which were relatively less cellular and contained more loosely arranged cells (Fig. 3a). The immunohistochemical staining for a biomarker of cells of neural cell crest origin i.e., the S-100 protein was positive (Fig. 3b). As a result, a pathologic diagnosis was made that the lesion was a schwannoma.
Schwannomas can be classified by their anatomical locations e.g., intermuscular, intramuscular, subcutaneous, and intraosseous schwannomas (789). Symptoms of schwannomas are pain at rest, tenderness, “Tinel-like” signs, sensory disturbances, and motor weaknesses (89).
In this case, the schwannoma was located in an intermuscular plane, between the vastus lateralis and the vastus intermedius muscles. It may be difficult to identify the neurogenic origin based on a physical examination because the patient did not have any symptoms like sensory disturbances, “Tinel-like” signs, or motor weakness, which can accompany a schwannoma.
Magnetic resonance imaging (MRI) scans can be more useful in the preoperative diagnosis of the schwannoma than physical examinations (178).
The following imaging characteristics describe the neurogenic origin of the tumors and are consistent with a diagnosis of schwannomas: 1) The “split-fat sign,” ie, the lesion is surrounded by a rim of fat; this appearance is related to the displacement of the fat that normally surrounds the neurovascular bundle (78). 2) As a schwannoma is a neurogenic tumor, entering and exiting nerve roots are commonly visualized at both ends of a fusiform mass. However, the entry and exit signs are not always seen when the affected nerve is a small muscular branch (78). 3) The low-signal margin also can be seen on T1 and T2-weighted images; this margin corresponds to the epineurium surrounding the schwannoma (138). 4) The “target sign,” in which the lesion shows a thin, peripheral hyper-intense rim and a central lower-signal-intensity on T2-weighted images (38). The target sign correlates to a histologic analysis of the lesion. The central area of low signal intensity corresponds to the fibrocollagenous tissue and the surrounding area of high signal intensity correlates to the presence of more myxomatous tissue (38).
In this case, the lesion was totally surrounded by fat tissue and encapsulated in the low-signal margin. These nonspecific imaging findings were characteristic of schwannomas (1368).
Schwannomas are mostly solid tumors, and the histologic hallmarks of schwannoma are the presence of Antoni A and Antoni B regions. Antoni A areas are composed of spindle cells and more organized. Antoni B regions are characterized by hypocellular, less organized features and the presence of more myxoid tissue in each area (1389). The characteristic imaging finding of a “target sign” corresponds to the central low-signal intensities of the Antoni A regions and the peripheral high signal intensities of the Antoni B regions (38). Schwannomas commonly undergo degenerative changes including cyst formation, calcification, hemorrhages, and fibrosis (138). The irregular appearance of any schwannoma can be attributed to irregular mixtures of Antoni A and Antoni B regions with variable degrees of degenerative changes. Homogeneous patterns are occasionally visible on MRI scans (8). In summary, schwannomas can be identified as three patterns on T2-weighted MRI scans ie, the target sign, inhomogeneous, and homogeneous patterns (38). However, a purely cystic appearance is rare in schwannomas and these masses can be described as being benign cyst-like solids or partly solid lesions based on the degree of degenerative changes (345).
MRI scans analyzed in this study showed that the patient had a tumor which did not have a partly solid lesion. Instead, the mass could be described as a purely hemorrhagic cystic tumor with no connected nerve fibers. It is, therefore, difficult to diagnose the lesion as a schwannoma based on imaging findings. The differential diagnosis may include cystic masses such as a ganglion cyst with a hemorrhage and a hematoma.
In summary, we report an unusual imaging finding of a purely hemorrhagic cystic tumor in the intermuscular plane which we identified as a schwannoma. Awareness of these characteristics will be helpful for the radiologist in early diagnosis and optimal management of the condition.
Figures and Tables
Fig. 1
Schwannoma in a 63-year-old woman. (a) An axial modified proton density image (TR/TE = 2500/33) shows an oval cystic lesion with fluid-fluid level (black arrow). The lesion is surrounded by rectus femoris (*, star shape), vastus lateralis (black arrowhead), and vastus intermedius (white arrowhead) muscles. (b) A sagittal modified proton density image (TR/TE = 2500/33) shows an oval multilocular cystic lesion with low-signal margin. The lesion is surrounded by a rim of fat (split-fat sign) (white arrowheads). (c) Fat-suppressed contrast enhanced T1-weighted axial image (TR/TE = 989/18) shows thin rim enhancement of the cystic mass.

Fig. 2
Photograph of surgical resection specimen of a schwannoma. (a) On gross finding, the lesion is an oval shape and the capsule is yellow-tinged grayish color. (b) Reddish hematoma is noted in the cystic lesion and the surface of the lumen is brown.

Fig. 3
Photomicrograph of a histologic specimen of schwannoma. (a) Pathologic specimen (original magnification, × 100; Hematoxylin-Eosin stain) shows the Antoni A region (not seen in this image) intermingled with the Antoni B region (white arrowhead) in a schwannoma. Wavy, tightly organized nuclear palisades known as Verocay bodies (black arrowheads) occupy the center of a highly cellular field. (b) Pathologic specimen (original magnification, × 200; S-100 stain) shows the universally S-100 stained cells of a schwannoma.
References
1. Murphey MD, Smith WS, Smith SE, Kransdorf MJ, Temple HT. From the archives of the AFIP. Imaging of musculoskeletal neurogenic tumors: radiologic-pathologic correlation. Radiographics. 1999; 19:1253–1280.
2. Ogose A, Hotta T, Koda H, Umezu H, Higuchi T. Images in rheumatology. Hemorrhagic schwannoma with purely cystic appearance in the shoulder. J Rheumatol. 2001; 28:2558–2559.
3. Bermejo A, De Bustamante TD, Martinez A, Carrera R, Zabia E, Manjon P. MR imaging in the evaluation of cystic-appearing soft-tissue masses of the extremities. Radiographics. 2013; 33:833–855.
4. Wu D, Ba Z, Huang Y, Zhao W, Shen B, Kan H. Totally cystic schwannoma of the lumbar spine. Orthopedics. 2013; 36:e679–e682.
5. Lee HA, Jeon SJ, Choi SS, Kim HW, Kim HS. A purely cystic giant sacral schwannoma mimicking a bone cyst: a case report. J Korean Soc Radiol. 2014; 71:1–5.
6. Lin J, Martel W. Cross-sectional imaging of peripheral nerve sheath tumors: characteristic signs on CT, MR imaging, and sonography. AJR Am J Roentgenol. 2001; 176:75–82.
7. Kwon BC, Baek GH, Chung MS, Lee SH, Kim HS, Oh JH. Intramuscular neurilemoma. J Bone Joint Surg Br. 2003; 85:723–725.
8. Shimose S, Sugita T, Kubo T, et al. Major-nerve schwannomas versus intramuscular schwannomas. Acta Radiol. 2007; 48:672–677.
9. Knight DM, Birch R, Pringle J. Benign solitary schwannomas: a review of 234 cases. J Bone Joint Surg Br. 2007; 89:382–387.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download