Abstract
Purpose
The purpose of this study was to compare the grade of fatty degeneration and atrophy of rotator cuffs on immediate postoperative MRI to those on preoperative MRI in patients with rotator cuff tears.
Materials and Methods
Seventy patients were included in this study, who received arthroscopic rotator-cuff repair and underwent both preoperative magnetic resonance imaging (MRI) and immediate postoperative MRI in our institution. Fatty degeneration of rotator cuffs and the atrophy of supraspinatus muscles were evaluated with T1 oblique sagittal images in the Y-shaped view. Fatty degeneration was evaluated using a Goutallier classification system, and the atrophy of supraspinatus muscles was evaluated using a modified tangent sign and a visual occupation ratio.
Results
From 70 patients, a total of 100 tendons were repaired: 18, 69, and 13 tendons were treated for subscapularis, supraspinatus, and infraspinatus, respectively. The Goutallier grades (P = 0.012), modified tangent signs (P = 0.000), and visual occupation ratios (P = 0.000) of supraspinatus muscles were significantly decreased in immediate postoperative MRIs when compared to preoperative MRIs. In immediate postoperative MRIs, the Goutallier grades of supraspinatus muscles were decreased by one grade in 18.8% (n = 13) of the patients, and the atrophy of supraspinatus muscles was improved by one grade in 26.1% (n = 18) for modified tangent signs and 21.7% (n = 15) for visual occupation ratios. However, fatty infiltration by the Goutallier grades of subscapularis (P = 1.000) and infraspinatus (P = 0.157) muscles were not significantly changed after arthroscopic surgery.
Fatty degeneration and the atrophy of rotator cuffs are important prognostic factors to predict the clinical and surgical outcomes of rotator-cuff repair (123). The classification system to assess the fatty infiltration of rotator cuffs was introduced by Goutallier et al. (4) in 1994, using axial image from computed tomography (CT). Fuch et al. (5) adapted this classification system to magnetic resonance imaging (MRI) using T1-weighted oblique sagittal images. Many studies have raised significant concern for the reliability and accuracy of Goutallier classification based on MRI (678), but it is a simple and easily understood method for assessing the fatty degeneration of rotator cuffs as well as the most widely used classification system used currently. The atrophy of supraspinatus muscles has been evaluated by tangent signs (8) and occupation ratios (29) in the Y-shaped view (i.e., the most lateral image where the scapular spine is in contact with scapular body).
Immediate postoperative MRIs have been performed within 2 to 4 days after the arthroscopic repair of rotator cuffs in our institution. In our experience, the severity of fatty degeneration or the atrophy of rotator cuffs in immediate postoperative MRIs looked quite different from those in preoperative MRIs. If the fatty degeneration or the atrophy of rotator cuffs are different between pre- and immediate postoperative MRIs, these differences should be considered when we compare the outcome of rotator cuffs in the follow-up studies.
The purpose of our study is to compare the fatty degeneration and atrophy of rotator cuffs in immediate postoperative MRIs to those of preoperative MRIs.
Our Institutional Review Board has approved this retrospective study and waived the requirement for patients' informed consent as all MRIs were obtained following our clinical protocols; patient confidentiality was maintained.
Between January and December of 2015, 125 patients underwent arthroscopic shoulder surgery for rotator cuff tears; they also underwent immediate postoperative MRIs. We excluded 55 patients from the study, 49 of which had received preoperative MRIs in other institutions; 6 of the 55 patients had limited coverage or severe motion artifact in their immediate postoperative MRIs because of pain. In the end, 70 subjects were included in this study.
We included a total of 100 tendons from 70 patients, 46 of whom were female (mean age, 64.7 years; age range, 49-79) and 24 of which were male (mean age, 62.5 years; age range, 21-79). The preoperative MRI was arthrographic for 59 patients and non-arthrographic for 11 patients. The average interval between pre- and postoperative MRIs was 34 days, ranging between 4 and 102 days.
The MRIs were performed with a 3.0T scanner (Achieva 3.0T; Philips Medical Systems, Eindhoven, The Netherlands) equipped with a dedicated shoulder coil. For each patient, the affected arm was placed at the side of the body in the supination position. Assessments of fatty degeneration and the atrophy of rotator cuffs were made on T1-weighted oblique sagittal images obtained on a plane perpendicular to the long axis of the supraspinatus tendon (repetition time/echo time, 530/20 ms; matrix, 356 × 258; slice thickness, 4 mm; inter-slice gap, 0.4 mm; field of view, 16 cm; flip angle, 90°; and echo train length, 3). The preoperative shoulder MRI was either non-arthrographic or arthrographic MRI with the same protocol as immediate postoperative MRI, as described above. Jo et al. (10) have shown that the difference between these protocols (i.e., arthrographic MRI in preoperative evaluation and non-arthrographic MRI in postoperative evaluation) has little effect on the assessments of fatty degeneration and rotator-cuff atrophy; hence, we included all patients who had undergone either arthrographic or non-arthrographic MRIs for preoperative evaluation. Fluoroscopically guided intraarticular injection was done for MR arthrography with 10-15 ml of MR contrast material (Gadovist 1.0; Schering, Berlin, Germany) at a gadolinium concentration of 1.0 mol/L, diluted 1:400 in normal saline. All immediate postoperative MRIs were performed within 2-4 days after surgery without an intra-articular injection.
Arthroscopic procedures included the following: isolated subscapularis tendon repair in 1 patient, subscapularis and supraspinatus tendon repair in 13 patients, isolated supraspinatus tendon repair in 43 patients, supraspinatus and infraspinatus tendon repair in 9 patients, and all three tendon repair in 4 patients.
All arthroscopic procedures were performed with patients in the lateral decubitus position under general anesthesia. After the frayed edges of the torn tendon(s) were removed, tendon mobilization procedures were done, if necessary. Subscapularis tendons were debrided or fixed with a single anchor screw, as needed. Supraspinatus and infraspinatus tendons were repaired with the suture bridge technique with minimal decortication of the footprint to enhance tendon healing.
The fatty degeneration of subscapularis, supraspinatus, and infraspinatus muscles was assessed using a Goutallier classification modified by Fuchs et al. (5) on the Y-shaped view. In all three muscles, the following grading was applied according to Goutallier et al. (4): grade 0, which appears normal; grade 1, which contains some fatty streaks; grade 2, which contains more muscle than fat; grade 3, which contains as much fat as muscle; and grade 4, which contains more fat than muscle.
Atrophy of the supraspinatus muscle was assessed by modified tangent signs and visual grading for the occupation ratio (1011) (Fig. 1). The modified tangent sign was negative (grade 1) when the supraspinatus muscle crossed over the line (tangent) drawn through the superior borders of the scapular spine and the superior margin of the coracoid process. A borderline modified tangent sign (grade 2) was given when the supraspinatus muscle touched the tangent line, and a positive (grade 3) sign was given when the supraspinatus muscle was clearly below the tangent. Visual occupation ratios were categorized based on a threepoint scale: grade 1 involved minimal to mild atrophy of the supraspinatus muscle and an occupation ratio ≥ 60%; grade 2 involved moderate atrophy, 60% > an occupation ratio ≥ 40%; and grade 3 represented severe atrophy with an occupation ratio < 40% (12).
All image analyses were conducted by two fellowship-trained musculoskeletal radiologists with 11 and 12 years of experience, respectively. To evaluate interobserver and intraobserver reliability, random samples of 30 patients were reassessed in a different session by two readers who were blinded to the results of the first assessment. If there was a disagreement, the final decision was made by a consensus of the readers.
Intraobserver and interobserver agreements were assessed with linearly-weighted kappa values using MedCalc, version 16.8 (MedCalc Software; Ostend, Belgium). All other analyses were performed using SPSS software, version 20.0 (IBM; Armonk, NY, USA). The Wilcoxon signed-rank test was used to compare the pre- and postoperative Goutallier grades per each repaired tendon. Grades by tangent signs and visual occupation ratios of supraspinatus in preoperative MRI and those in postoperative MRI were also compared by a Wilcoxon signed-rank test. A P-value < 0.05 was considered significant.
The number of repaired tendons (by type) and the grades of fatty degeneration and atrophy are shown in Table 1. Interobserver and intraobserver agreement for all grading showed substantial and nearly excellent agreement, as shown in Table 2. Overall, modified tangent sign grades showed better interobserver/intraobserver agreement than visual occupation ratio grades.
The Goutallier grades of subscapularis, supraspinatus, and infraspinatus observed in pre- and postoperative MRIs are demonstrated in Figure 2. The Goutallier grades for supraspinatus muscles showed a significant decrease in immediate postoperative MRIs (P = 0.012). But, the Goutallier grades for subscapularis (P = 1.000) and infraspinatus (P = 0.157) muscles were not significantly changed in immediate postoperative MRIs. For supraspinatus muscles, fatty infiltration decreased by one grade in 13 patients, and fatty infiltration increased by one grade in 3 out of 69 patients. The supraspinatus muscles showed an improved Goutallier grade after arthroscopic surgery and were all grades 3 and 4 in preoperative MRIs. Three supraspinatus muscles, which showed more advanced fatty infiltration in postoperative MRIs, were grade 1 in the preoperative MRI.
A significant decrease of supraspinatus muscle atrophy was noted in immediate postoperative MRIs when evaluated with the modified tangent sign (P = 0.000) and the visual occupation ratio (P = 0.000) (Fig. 3). The modified tangent sign grades were one grade lower in immediate postoperative MRIs in 26.1% of the total repaired supraspinatus muscles. Two out of 3 supraspinatus muscles (66.7%) with grade 3 atrophy showed decreased modified tangent sign grades in immediate postoperative MRIs, while 16 out of 18 supraspinatus muscles (88.9%) had grade 2 atrophy on preoperative MRI. In immediate postoperative MRIs, the visual occupation ratio was one grade lower in 21.7% of the total repaired supraspinatus muscles, which were one grade lower in 72.2% (13 out of 18) in grade 2 and 66.7% (2 out of 3) in grade 3 supraspinatus muscles in preoperative MRIs, respectively. In contrast, grade 1 muscles in preoperative MRIs using a visual occupation ratio did not change in the degree of atrophy upon immediate postoperative MRIs.
Fatty degeneration and atrophy of rotator cuffs are known prognostic factors affecting the outcome of rotator-cuff repair, but the change of rotator cuffs after surgical repair is controversial among investigators. Some authors have found that fatty degeneration or atrophy is reversible after rotator-cuff repair or, at least, it is possible to prevent further degeneration or atrophy (313). However, others have reported progressive fat accumulation and atrophy of rotator cuffs regardless of the structural integrity after repair (12).
The fatty degeneration or atrophy of rotator cuffs are frequently assessed in the oblique sagittal images of postoperative MRIs, as compared to those of preoperative MRIs in previous studies. However, those results might be false positive if the differences between preoperative and immediate postoperative MRIs are overlooked. The improvement of fatty degeneration or atrophy of rotator cuffs after the arthroscopic repair of the tendon can be the result of the arthroscopic surgery itself.
In our study, the Goutallier grade of supraspinatus muscles was one degree lower in immediate postoperative MRIs in 18.8% of the patients after arthroscopic tendon repair. Furthermore, the atrophy of supraspinatus muscles was one grade lower in 26.1% with the modified tangent sign and in 21.7% with the visual occupation ratio (Fig. 1) on the immediate postoperative MRI. Jo et al. (10) reported the change in the Goutallier grade, the tangent sign grade and the occupational ratio grade were at least 1 grade in 45.5%, 35.6% and 23.7%, respectively. The general proportion of the change in supraspinatus muscles in our study were much smaller than that in the previous study by Jo et al. (10). But the trend was similar to our study that the more severely degenerated or atrophied muscles showed more changes in their appearance on a postoperative MRI. Therefore, the fatty degeneration, according to the Goutallier grade, and atrophy, according to the modified tangent sign or visual occupation ratio, of supraspinatus muscles on immediate postoperative MRIs were significantly different from those of preoperative MRIs. We can also conclude that the rotator cuff repair can affect the fatty degeneration and muscle atrophy, at least for supraspinatus on immediate postoperative MRI.
Recently, tendon retraction has gained attention as the cause of false positive muscle atrophy on preoperative MRIs. Yoo et al. (14) found that the conventional Y-shaped view is distant from the osseous origin of supraspinatus tendon, at which non-attached muscle and tendon can be freely retracted. Fukuta et al. (15) reported that supraspinatus tendon retraction has negative correlation with the cross-section area of the supraspinatus tendon. In the conventional Y-shaped view, tendon retraction can cause pseudo-atrophy of the muscle by the proximal migration of the muscle belly in preoperative MRIs. Since the torn tendon is repaired and repositioned in its anatomical location after the operation, immediate postoperative MRIs should be the baseline study that can visualize the true muscle quality in a Y-shaped view.
Tendon retraction might be one of the possible explanations of our results, showing that more frequent changes were found in muscles with a more severe degree of fatty degeneration or atrophy. If the muscles show advanced fatty degeneration and atrophy, it is reasonable to assume that those muscles had a chronic and severe degree of injury, which can be associated with severe tendon retraction. Therefore, severely degenerated muscles can have more retracted tendons and can show more changes in the appearance of the rotator cuff in the postoperative MRI Y-shaped view, as compared to preoperative MRI.
Our study has several limitations. First, we included different MRI protocols for pre- and postoperative conditions. Both arthrographic and non-arthrographic MRIs were used for preoperative evaluation, and non-arthrographic MRIs were used postoperatively. Yet, Jo et al. (10) concluded that these different protocols could be used to compare between pre- and postoperative MRIs. In addition, the contrast material in the subscapular recess in arthrographic MRIs was occasionally visible in the Y-shaped view, but this material did not disturb the grading of fatty degeneration or atrophy of rotator cuffs due to its typical location and localization in the recess. Second, we included patients with a different range of tendon tears and different degrees of retraction, and our results showed a significant difference in the supraspinatus muscle alone. This difference might be caused by the different proportions of the tendons involved; most patients included in this study had supraspinatus tendon tears. Since subscapularis tendon tears and infraspinatus tendon tears are much rarer than supraspinatus tears, it was difficult to include subscapularis tendon tears in this study. Third, there is a fundamental limitation in MR imaging, that it is very difficult to scan the exact same plane between the two MRI performed in the different time point. Because the imaging plane can be affected by the position (degree of rotation) of the arm, selected angle of oblique sagittal scan and the location of the center, we perform shoulder MRIs according to the manual in our institution to reduce these discrepancy. And we carefully selected the slice by the definition of the Y-shaped view. Finally, we also did not assess the degree of tendon retraction, which could be performed in another study in the future.
In conclusion, immediate postoperative MRIs showed a significant difference in the fatty degeneration and muscle atrophy of supraspinatus compared to preoperative MRIs. This difference should be considered when comparing post- and preoperative MRIs to assess changes of fatty degeneration and supraspinatus muscle atrophy.
This study was supported by the research fund of the Radiological Research Foundation of Korea (2011).
Figures and Tables
Fig. 1
Pre- and immediate postoperative MRIs of a 69-year-old female patient. The interval between the two MRIs was eight days. (a) The preoperative MRI shows atrophy of supraspinatus muscle; grade 2 (borderline) by the modified tangent (represented by a dashed line) sign and grade 3 (< 40%) by the visual occupation ratio. (b) The postoperative MRI shows atrophy of the supraspinatus muscle; grade 1 (negative) by the modified tangent sign and grade 2 (40-60%) by the visual occupation ratio. The occupation ratio of the cross-sectional area of the supraspinatus muscle to the supraspinatus fossa (represented by a dotted line) was assessed visually.
Fig. 2
The fatty infiltration grades of subscapularis, supraspinatus, and infraspinatus observed in pre- and postoperative MRIs are shown in a stacked bar graph. The Goutallier grades of subscapularis tendons were not changed after arthroscopic surgery. Note the decreased number of patients showing grade 3 and grade 4 fatty degeneration of the supraspinatus upon postoperative MRI.
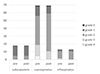
Fig. 3
Grades of supraspinatus muscle atrophy, assessed by a modified tangent sign and visual occupation ratio in pre- and postoperative MRIs, are shown in a proportional stacked bar graph. Note the decrease of proportion of patients showing grade 2 and grade 3 atrophy assessed by a modified tangent sign and visual occupation ratio upon postoperative MRIs.

Table 1
Grades of Fatty Infiltration and Atrophy in Repaired Tendons

Table 2
Intraobserver and Interobserver Agreement for the Grading System for the Fatty Degeneration of Rotator Cuffs and the Atrophy of Supraspinatus

References
1. Mellado JM, Calmet J, Olona M, et al. Surgically repaired massive rotator cuff tears: MRI of tendon integrity, muscle fatty degeneration, and muscle atrophy correlated with intraoperative and clinical findings. AJR Am J Roentgenol. 2005; 184:1456–1463.
2. Gerber C, Schneeberger AG, Hoppeler H, Meyer DC. Correlation of atrophy and fatty infiltration on strength and integrity of rotator cuff repairs: a study in thirteen patients. J Shoulder Elbow Surg. 2007; 16:691–696.
3. Thomazeau H, Boukobza E, Morcet N, Chaperon J, Langlais F. Prediction of rotator cuff repair results by magnetic resonance imaging. Clin Orthop Relat Res. 1997; 275–283.
4. Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994; 78–83.
5. Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C. Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg. 1999; 8:599–605.
6. Oh JH, Kim SH, Choi JA, Kim Y, Oh CH. Reliability of the grading system for fatty degeneration of rotator cuff muscles. Clin Orthop Relat Res. 2010; 468:1558–1564.
7. Spencer EE Jr, Dunn WR, Wright RW, et al. Interobserver agreement in the classification of rotator cuff tears using magnetic resonance imaging. Am J Sports Med. 2008; 36:99–103.
8. Zanetti M, Gerber C, Hodler J. Quantitative assessment of the muscles of the rotator cuff with magnetic resonance imaging. Invest Radiol. 1998; 33:163–170.
9. Thomazeau H, Rolland Y, Lucas C, Duval JM, Langlais F. Atrophy of the supraspinatus belly. Assessment by MRI in 55 patients with rotator cuff pathology. Acta Orthop Scand. 1996; 67:264–268.
10. Jo CH, Shin JS. Changes in appearance of fatty infiltration and muscle atrophy of rotator cuff muscles on magnetic resonance imaging after rotator cuff repair: establishing new time-zero traits. Arthroscopy. 2013; 29:449–458.
11. Lim HK, Hong SH, Yoo HJ, et al. Visual MRI grading system to evaluate atrophy of the supraspinatus muscle. Korean J Radiol. 2014; 15:501–507.
12. Deniz G, Kose O, Tugay A, Guler F, Turan A. Fatty degeneration and atrophy of the rotator cuff muscles after arthroscopic repair: does it improve, halt or deteriorate? Arch Orthop Trauma Surg. 2014; 134:985–990.
13. Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2000; 82:505–515.
14. Yoo HJ, Choi JY, Hong SH, Kim EJ, Kim SH. Quantifying rotator cuff atrophy and fatty degeneration at the supraspinatus origin in the scapular fossa. Knee Surg Sports Traumatol Arthrosc. 2015; 23:399–407.
15. Fukuta S, Tsutsui T, Amari R, Wada K, Sairyo K. Tendon retraction with rotator cuff tear causes a decrease in cross-sectional area of the supraspinatus muscle on magnetic resonance imaging. J Shoulder Elbow Surg. 2016; 25:1069–1075.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download