Abstract
Among the various types of congenital meniscal anomalies, the double-layered lateral meniscus is extremely rare. The double-layered meniscus consists of both the upper additional and the lower normal meniscus. As the upper additional meniscus is mobile, it can be easily displaced, while the lower lateral meniscus is usually normal in shape and volume.
A 42-year-old woman suffering from pain and locking of her left knee underwent Magnetic resonance imaging (MRI) examination and an arthroscopic surgery. A rare meniscal abnormality was seen in her left knee, which presented as a double-layered lateral meniscus with displacement. It was remarkable that the upper additional meniscus was displaced over the intercondylar eminence of the tibia and it mimicked a bucket-handle tear. Even though it is rare, it is necessary to consider the possibility of displaced double-layered meniscus in the differential diagnosis of a bucket-handle tear. Here, we report the MRI and arthroscopic findings of a displaced double-layered lateral meniscus, which was similar to the bucket-handle tear.
Various different types of meniscal abnormalities have been reported in the literature. Among them, the occurrence of a double-layered lateral meniscus is extremely rare. The double-layered lateral meniscus includes both the upper additional and the lower normal meniscus (1) (Fig. 1). As the upper additional meniscus is mobile, although very rare, it can be displaced and flipped over the intercondylar eminence of tibia, mimicking the bucket-handle tear. In the English literature, there is only one previously published report of a displaced double-layered lateral meniscus that mimicked the bucket-handle tear (2). Here, we describe a rare case of displaced double-layered lateral meniscus mimicking the bucket-handle tear, where a displaced upper additional meniscus was observed in the intercondylar notch of the knee.
A 42-year-old woman presented with a 12-month history of pain and locking in her left knee. She had no history of injury or inflammation in that area and was otherwise healthy. Upon physical examination, a positive McMurray's test and lateral side tenderness in the left knee were observed. Neurovascular examination was normal. Laboratory data, including the erythrocyte sedimentation rate and C-reactive protein levels, were unremarkable. Additionally, the plain film radiographs of both her knees were normal. To evaluate abnormalities in the meniscus, cartilage or ligament, MRI of the left knee was performed using a 3.0-T scanner (Magnetom Skyra, Siemens, Erlangen, Germany). On coronal and sagittal proton density weighted images, a displaced meniscal fragment was noted over the intercondylar eminence of tibia, which originated from the lateral meniscus, and two layered meniscal structures were also noted in the lateral femorotibial compartment of the left knee (Fig. 2). Our initial diagnostic impression was a bucket-handle tear of the lateral meniscus.
Hence, the patient underwent arthroscopic surgery on the left knee. During arthroscopic evaluation of the lateral compartment, a fragment of lateral meniscus was found to be displaced medially toward the intercondylar notch, as in a bucket-handle tear, and the displaced meniscal fragment was mobile and easily reduced by using the arthroscopic probe.
The lateral compartment of the knee was examined in detail after reduction of a displaced meniscal fragment. Upon arthroscopy, a displaced meniscal fragment with semicircular shape was observed over the original lateral meniscus, which extended from the posterior horn to mid body of the lower lateral meniscus. Its anterior edge was in contact with the upper surface of mid body of the lower meniscus, and its posterior and peripheral portions were connected to the joint capsule. A lower lateral meniscus was undamaged and looked completely normal in shape and volume, along with a smooth and intact margin, as in a normal meniscus (Fig. 3). Subsequently, we completely removed this upper additional meniscus.
Histological findings of the resected upper meniscus showed multiple layers of dense collagen fibers with normal organization, and linearly arranged fibro-chondrocytes, corresponding to a typical meniscal structure (Fig. 4).
Based on these arthroscopic, MRI and histological findings, we concluded that this unusual anomaly was a double-layered meniscus. In addition, an upper additional meniscus was displaced which mimicked a bucket-handle tear.
The patient's symptoms disappeared after arthroscopically removing the upper additional meniscus.
Many reports in the past have described the various types of congenital meniscal anomalies. These can be classified into different pathologic entities, according to relative size, shape and attachment. Among them, discoid meniscus is the most common morphological anomaly (3).
Other less common anomalies include a ring-shaped meniscus, congenital absence of the menisci, partial deficiency of the meniscus, abnormal band formation, hypoplastic lateral meniscus and a double-layered lateral meniscus (145). These meniscal anomalies occur far more frequently and variously in the lateral meniscus than in the medial meniscus (56). Such variations are likely due to multifactorial causes with congenital and developmental influences, but clinical features, pathology, and epidemiology of these variations are still unknown (2). Among these variations, the double-layered meniscus as observed in our case is an extremely rare anomaly of the lateral meniscus, in which an upper additional meniscus was overlying the normal lateral meniscus (1).
Bailey and Blundell (7) reported the case of a partially duplicated lateral meniscus in a 5-year-old girl, which attached to the mid-lateral surface of lateral femoral condyle extending from the posterior horn to the anterior horn of the lateral meniscus. Similarly, Suzuki et al. (1) reported two cases of double-layered lateral meniscus, with one meniscus overlying the other.
Subsequently, a few authors have described similar cases of double-layered lateral meniscus.
In these cases, it was characteristic that the upper additional semicircular meniscus lay marginal and parallel to the lower normal lateral meniscus and it was thinner and more mobile than the lower normal lateral meniscus. Further, it extended from the posterior horn to midbody or the anterior horn of the lower normal meniscus and was attached to lateral surface of the lateral femoral condyle (289).
In our case, an upper accessory meniscus was extending from the posterior horn to mid body of the lower normal meniscus; and its peripheral edge was not connected to the lower meniscus. These findings are in agreement with previous reports by other authors (128910).
Moreover, the upper additional meniscus in our case was displaced and flipped over the intercondylar eminence of tibia, mimicking the bucket-handle tear; the overlapping double-layered meniscal structure was also similar to the horizontal meniscal tear.
Therefore, differential diagnosis of the displaced double-layered meniscus as observed in our case, should include bucket-handle tear and horizontal meniscal tear. In a typical bucket-handle tear, the two ends of the bucket-handle meniscal fragment are continuous in the medial margin of the meniscus. Whereas, in a double-layered meniscus, the upper additional meniscus is in contact with the upper or lateral surface of the lower normal meniscus. Furthermore, the width and volume of the remaining lower meniscus are within the normal range; its margin and surface are smooth and glossy despite removal of the upper additional meniscus. Moreover, there are no tears or degenerative changes in the remaining lower meniscus. The shape of the resected upper additional meniscus is similar to the usual meniscus. Meanwhile, a bucket-handle tear is usually associated with trauma (2810). The comparisons between a displaced double-layered lateral meniscus and a bucket-handle tear are summarized in Table 1.
Although it is difficult to distinguish a displaced double-layered lateral meniscus from a bucket-handle meniscal tear, considering the above findings and features can eliminate a bucket-handle tear from the differential diagnosis.
Also in our case, after resection of the upper meniscal structure, the volume and morphology of the lower lateral meniscus were within the normal range as well as its margin and surface were smooth, intact and glossy, and there were no ligamentous abnormalities in the knee joint.
To our knowledge, as yet there is only one previously published report of a displaced double-layered lateral meniscus mimicking the bucket-handle tear (2). The MRI and arthroscopic findings of this previous report were similar to our case.
Regarding differentiation from a horizontal meniscal tear, the cleavage of a horizontal meniscal tear is usually irregular. Whereas, in a double-layered meniscus, the margins of the upper and lower meniscus are sharp, smooth and regular. In addition, the volume of remaining lower meniscus is normal, which suggests that the abnormality is not due to a horizontal tear (8).
Therefore, the differential diagnosis of a displaced double-layered meniscus can be achieved using the information above, even though it is often misdiagnosed as a bucket-handle tear or horizontal tear of the meniscus.
In the MRI findings of our case, there was a redundant meniscal fragment overlying the intercondylar eminence of tibia, which is typically interpreted as a displaced meniscal tear such as the bucket-handle tear. During arthroscopy, this displaced meniscal fragment was proved to be the upper additional meniscus overlying the normal lateral meniscus. It was successfully removed after arthroscopic surgery and the patient's symptoms improved significantly thereafter.
In conclusion, the upper additional meniscus of the double-layered lateral meniscus can be displaced and flipped over the intercondylar eminence of tibia, mimicking the bucket-handle tear. Therefore, it is important to consider the possibility of a displaced double-layered lateral meniscus in the differential diagnosis of a bucket-handle tear.
Figures and Tables
 | Fig. 1A schematic illustration of the double layered lateral meniscus, which is characteristic that the upper additional meniscus overlays the normal lateral meniscus. ACL = anterior cruciate ligament, AH = anterior horn, LTP = lateral tibial plateau, NLM = normal lateral meniscus, PCL = posterior cruciate ligament, PH = posterior horn, UALM = upper additional lateral meniscus |
 | Fig. 2Left knee MRI of a 42-year-old female presenting pain. A coronal proton density (PD) weighted spin-echo image (TR/TE, 2180/11) shows a double layered lateral meniscus, which includes the upper additional meniscus (black arrows) overlying the lower normal lateral meniscus (a, b) and a displaced meniscal fragment (white arrows) over the intercondylar eminence of tibia, mimicking the bucket-handle tear (b-d). A sagittal PD weighted spin-echo image (TR/TE, 2450/11) also shows the upper additional meniscus (black arrows) overlying the normal lateral meniscus (e) and a displaced upper additional meniscus (white arrows) over the intercondylar eminence of tibia (f). |
 | Fig. 3Arthroscopic view of the lateral compartment shows that the upper additional meniscus overlying the normal lateral meniscus is displaced toward the intercondylar notch and mimics the bucket-handle tear; while the shape, margin and volume of the lower lateral meniscus is completely normal. These findings are suggesting a displaced double-layered meniscus. AHLM = anterior horn of lateral meniscus, LFC = lateral femoral condyle, LTP = lateral tibial plateau, PHLM = posterior horn of lateral meniscus |
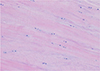 | Fig. 4Histology of the resected upper meniscus shows dense collagen fibers in multiple layers with normal organization, and fibro-chondrocytes that are linearly arranged, consistent with a typical meniscal tissue (H&E stain, × 200). |
Table 1
Summarized Comparisons between a Displaced Double-Layered Lateral Meniscus and a Bucket-Handle Tear

References
1. Suzuki S, Mita F, Ogishima H. Double-layered lateral meniscus: a newly found anomaly. Arthroscopy. 1991; 7:267–271.
2. Lee KW, Yang DS, Choy WS. Dislocated double-layered lateral meniscus mimicking the bucket-handle tear. Orthopedics. 2013; 36:e1333–e1335.
3. Dickhaut SC, DeLee JC. The discoid lateral-meniscus syndrome. J Bone Joint Surg Am. 1982; 64:1068–1073.
4. Karahan M, Erol B. Accessory lateral meniscus: a case report. Am J Sports Med. 2004; 32:1973–1976.
5. Saygi B, Yildirim Y, Senturk S, Sezgin Ramadan S, Gundes H. Accessory lateral discoid meniscus. Knee Surg Sports Traumatol Arthrosc. 2006; 14:1278–1280.
6. Clark CR, Ogden JA. Development of the menisci of the human knee joint. Morphological changes and their potential role in childhood meniscal injury. J Bone Joint Surg Am. 1983; 65:538–547.
7. Bailey WH, Blundell tge. An unusual abnormality affecting both knee joints in a child. Case report. J Bone Joint Surg Am. 1974; 56:814–816.
8. Okahashi K, Sugimoto K, Iwai M, Oshima M, Fujisawa Y, Takakura Y. Double-layered lateral meniscus. J Orthop Sci. 2005; 10:661–664.
9. Wang Q, Liu XM, Liu SB, Bai Y. Double-layered lateral meniscus. Knee Surg Sports Traumatol Arthrosc. 2011; 19:2050–2051.
10. Takayama K, Kuroda R, Matsumoto T, et al. Bilateral double-layered lateral meniscus: a report of two cases. Knee Surg Sports Traumatol Arthrosc. 2009; 17:1336–1339.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download