Abstract
We report a case of tenosynovial giant cell tumor with severe bone erosion in the right fifth finger of a 46-year-old man. Throughout this case review, we describe the imaging findings of tenosynovial giant cell tumor with severe bone erosion and review the literatures regarding osseous lesions caused by tenosynovial giant cell tumor and their significance related to the differential diagnosis and patient treatment.
Tenosynovial giant cell tumor is a part of the spectrum of benign synovial proliferative lesions. The patients are usually adults and the peak incidence is the third to the fifth decades of life. The majority of these lesions occur in the hands and wrists. The characteristic MR imaging finding of tenosynovial giant cell tumor is hypointense signal intensity seen on T1- and T2-weighted images. Osseous abnormalities associated with tenosynovial giant cell tumor include pressure erosion, cystic change and degenerative change (1). However, severe bone involvement by tenosynovial giant cell tumor has infrequently been reported. This case report intends to describe tenosynovial giant cell tumor showing severe bone erosion and to review the literatures regarding bone lesions and their clinical significance such as the relationship between bone erosion and prognosis of tenosynovial giant cell tumor.
A 46-year-old man presented with a mass in the proximal phalanx level of his right fifth finger. The mass lesion was first detected as soft-tissue swelling 15 months previously, and the patient explained that the mass was slowly growing. He had experienced discomfort, such as a pulling sense of his skin, for two weeks before visiting the hospital. He had no history of trauma or cancer. On physical examination, there was no remarkable finding except for the soft-tissue mass in his right fifth finger, and he complained of no pain or tenderness in this finger. The mass was firm and showed a lobulated contour. The function of the PIP joint of the fifth finger was normal. Plain radiographs showed a soft-tissue mass showing a bulging contour in the proximal phalanx level of his right fifth finger. And intramedullary and cortical cystic lesions together with cortical erosion and trabeculation were detected. However, definite cortical perforation or cortical destruction was not found (Fig. 1). On MR imaging, the mass revealed an irregular margin, and circumferential growth surrounding the flexor digitorum tendon. Bone involvement by a soft-tissue mass and its intraosseous extension, when seen on MR images, is more aggressive than bone lesions seen on plain radiographs. The mass showed slightly hyperintense signal intensity to muscle on T1- and T2-weighted images (Fig. 2). However, dark signal intensity on T2-weighted images was seen in the periphery of the mass (Fig. 2b). A bone scan showed a mild increase in uptake in the right fifth finger (Fig. 3). According to these features, we suspected a tenosynovial giant cell tumor as this is a common benign soft-tissue tumor in the hand and shows slow growth. The differential diagnosis included fibroma and the possibility of desmoid-type fibromatosis and soft tissue sarcoma due to the severe bone invasion seen on MR images. Eventually, radical excision of the mass was performed. According to the intraoperative findings, the tumor had a yellowish color, a multi-lobulated contour, circumferential growth surrounding the proximal phalanx of the right fifth finger, and an ill-defined margin with adjacent bone and soft tissue. On pathologic examination, the tumor was proven to be a tenosynovial giant cell tumor which consisted of a polymorphous population of mononuclear stromal cells with small, round, spindle, rentiform nuclei, epithelioid macrophages with abundant eosinophilic cytoplasm, and vesicular nuclei and osteoclast-like giant cells (Fig. 4).
Tenosynovial giant cell tumor, also termed nodular tenosynovitis, is a benign, synovial, proliferative disease and one of the most common soft-tissue masses in the hand. Most patients are adults and present with a slowly growing and painless soft tissue-mass. The mass is mobile under the skin, although it is attached to deeper structures. The histological finding includes synovial proliferation with scattered multinucleated giant cells, macrophages, fibroblasts, and xanthoma cells (1). Varying amounts of hemosiderin may be observed. Because of the hemosiderin contents, tenosynovial giant cell tumor shows decreased signal intensity on both T1- and T2-weighted images. These features may be useful for differentiating it from other soft-tissue tumors occurring in the hand (2).
From the review of previous reports, bone lesion and intraosseous invasion by tenosynovial giant cell tumor have not been given attention and the focus was on the imaging findings of plain radiographs in the published reports. On the radiographs of patients with tenosynovial giant cell tumor, osseous abnormalities included pressure erosions, cystic change, and degenerative change (1). Uriburu et al. (3) reported 15 patients with tenosynovial giant cell tumor showing intraosseous growth in the digits. The most frequently involved site was phalanges among the affected digits. Typical radiographic findings include intraosseous lucency, cortical thinning, a subtle rim of perilesional bone sclerosis, and a coarse rim. Intraosseous lucency was seen in all of the patients. And in six patients, the bone lesion was a multilocular lesion in which the locule was separated from adjoining bones by normal or condensed bone trabeculae. De Schepper et al. (4) reported six patients with tenosynovial giant cell tumor. Three of these six patients showed a sharply marginated cortical lesion, one had a cortical defect and pressure erosion and two had an expansile intramedullary lesion of geographic destruction.
The differential diagnosis of tenosynovial giant cell tumor in the finger can include any soft tissue mass with low signal intensity seen on both T1- and T2-weighted images. Typical tenosynovial giant cell tumor shows a similar imaging finding with fibroma of the tendon sheath. However, fibroma of the tendon sheath is a rare benign tumor and bone involvement secondary to remodeling or extrinsic erosion in the finger is very uncommon (5). Atypical tenosynovial giant cell tumor with severe bone erosion can be differentiated from demoid-type fibromatosis and soft tissue sarcoma such as fibrosarcoma and undifferentiated sarcoma. Desmoid-type fibromatoses are usually intermuscular masses of deep soft tissue and characteristically grow along fascial planes (6). And in general, soft tissue sarcomas in the hand show an ill-defined margin, relatively large size, and heterogeneous signal intensity on T2-weighted images (7). However, actually distinguishing between a tenosynovial giant cell tumor and a soft tissue sarcoma using imaging finding is difficult.
Because an intraosseous bone lesion of tenosynovial giant cell tumor is related to the tumor recurrence and prognosis, complete resection of tenosynovial giant cell tumor is very critical for treating the disease and incomplete resection due to bone erosion or invasion by the tumor may be a significant risk factor for local tumor recurrence in the hand (8). Jalgaonkar et al. (9) recommended that curettage of the bone should be done in patients with osseous erosion in order to prevent recurrence. And Lu et al. (10) reported the case of artificial finger joint replacement in a patient with tenosynovial giant cell tumor as well as bone destruction that did not show complications such as tumor recurrence or joint dislocation. Therefore, diagnostic imaging, including radiography, CT and MRI, are all important for patients with tenosynovial giant cell tumor showing severe bone erosion. And from our review of past reports, CT and MRI have an important role for clearly demonstrating the intraosseous component of tenosynovial giant cell tumor. Through review of our case we can learn imaging finding of tenosynovial giant cell tumor with severe bone erosion and the application of imaging findings to clinical practice.
Figures and Tables
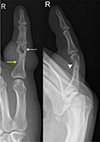 | Fig. 1Plain radiographs show a soft-tissue density showing bulging contour in the proximal phalanx level of the right fifth finger as well as intramedullary and cortical cystic lesions (white arrow) with trabeculation (yellow arrow) and cortical erosion (arrowhead) in the proximal phalanx. |
 | Fig. 2Coronal T1-weighted image (a) reveals a soft-tissue tumor associated with an intraosseous lesion. On the axial T2-weighted image (b), the tumor is seen to grow surrounding the flexor digitorum tendon (white arrow) and show severe bone erosion. There is dark signal intensity (yellow arrows) in the periphery of the mass. On axial gadolinium-enhanced T1-weighted image with fat saturation (c), enhancement of the tumor is seen. |
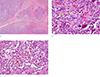 | Fig. 4Photomicrograph shows the multinodular growth pattern of the tumor with fibrous septa and stromal fibrosis (a, Hematoxylin & Eosin, × 40). The tumor is composed of a polymorphous population of mononuclear stromal cells (yellow arrows) with small round, spindle, rentiform nuclei, epithelioid macrophages (red arrows) with abundant eosinophilic cytoplasm, vesicular nuclei and osteoclast-like giant cells (black arrow). Mitotic figure is also noted (blue arrow) (b, Hematoxylin & Eosin, × 400). Sheets and clusters of xanthoma cells are frequently observed. Xanthoma cells (foamy macrophages) have copious, vacuolated cytoplasm and central nuclei. Siderophages (hemosiderin-laden macrophages) are also noted. (c, Hematoxylin & Eosin, × 400). |
References
1. Kransdorf MJ, Murphey M. Imaging of soft tissue tumors. 3rd ed. Philadelphia: Lippincott Williams & Wilkins, a WOLTERS KLUWER business;2014. p. 461–466.
2. De Beuckeleer L, De Schepper A, De Belder F, et al. Magnetic resonance imaging of localized giant cell tumour of the tendon sheath (MRI of localized GCTTS). Eur Radiol. 1997; 7:198–201.
3. Uriburu IJ, Levy VD. Intraosseous growth of giant cell tumors of the tendon sheath (localized nodular tenosynovitis) of the digits: report of 15 cases. J Hand Surg Am. 1998; 23:732–736.
4. De Schepper AM, Hogendoorn PC, Bloem JL. Giant cell tumors of the tendon sheath may present radiologically as intrinsic osseous lesions. Eur Radiol. 2007; 17:499–502.
5. Southwick GJ, Karamoskos P. Fibroma of tendon sheath with bone involvement. J Hand Surg Br. 1990; 15:373–375.
6. McDonald ES, Yi ES, Wenger DE. Best cases from the AFIP: extraabdominal desmoid-type fibromatosis. Radiographics. 2008; 28:901–906.
7. Chung WJ, Chung HW, Shin MJ, et al. MRI to differentiate benign from malignant soft-tissue tumours of the extremities: a simplified systematic imaging approach using depth, size and heterogeneity of signal intensity. Br J Radiol. 2012; 85:e831–e836.
8. Hamdi MF, Touati B, Zakhama A. Giant cell tumour of the flexor tendon sheath of the hand: analysis of 27 cases. Musculoskelet Surg. 2012; 96:29–33.
9. Jalgaonkar A, Dhinsa B, Cottam H, Mani G. Giant cell tumours of tendon sheath of hand: causes and strategies to prevent recurrence. Hand Surg. 2011; 16:149–154.
10. Lu H, Shen H, Chen Q, Shen XQ, Wu SC. Artificial finger joint replacement due to a giant cell tumor of the tendon sheath with bone destruction: a case report. Oncol Lett. 2015; 10:3502–3504.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download