Abstract
Arachnoid cysts (AC) are intraarachnoidal cerebrospinal fluid collections, and account for 1% of all intracranial space-occupying lesions. Intracystic hemorrhage of the AC can occur spontaneously, but this is an extremely rare event. Herein, we present a case of hemorrhagic AC in a nontraumatic patient in the left middle cranial fossa. We also performed relevant literature review on this disease.
Arachnoid cysts (AC) are cerebrospinal fluid collections surrounded by an arachnoid membrane. They are mostly of developmental anomalies and represent 1% of all intracranial space-occupying lesions (1). Although ACs are usually asymptomatic, they may present clinical symptoms by complications such as rupture with subdural hematoma, intracystic hemorrhage, and acute cyst expansion (2). ACs with intracystic hemorrhage in the absence of head trauma are extremely rare. In this paper, we present a case of hemorrhagic AC, and also performed a relevant literature review on this disease.
A 22-year-old man visited our hospital with a 3-day history of severe headache and vomiting. Although he received medical treatment for his symptoms, there was no improvement. He had no previous history of any neurological or medical disorders. There was also no history of recent trauma. Physical examination and laboratory studies revealed no specific abnormalities including external wound. A careful neurological examination revealed no focal sign. Therefore, brain CT and intracranial CT angiography were performed to evaluate intracranial lesion such as intracranial hemorrhage or mass lesion. CT scans revealed a well-circumscribed, hyperattenuating, extraaxial lesion in the left middle cranial fossa, suggesting acute hematoma (Fig. 1). The ipsilateral middle cerebral artery and its branches showed upward displacement by the lesion. And there was no visible vascular derangement such as steno-occlusive lesion or aneurysm in the major intracranial arteries. The preoperative impression was an acute hematoma with underlying AC. The patient underwent a fenestration of the cyst wall through a left frontotemporal craniotomy. After opening the dura, the hematoma was exposed lining by arachnoid membrane. When neurosurgeon punctured the lesion, the intracystic pressure was very high. Then, the operation composed a removal of intracystic hemorrhage and fenestration of the cyst and adjacent cisterns. Histopathological examination of the cystic wall was consistent with arachnoid membrane. After surgery, the patient did not complain of headache, and was discharged 2 weeks postoperatively without any complications. On follow-up MR imaging after 8 days, residual AC demonstrated as purely cystic mass with complete resolution of intracystic hemorrhage (Fig. 2).
ACs form 1% of the non-traumatic brain lesions and are generally considered to be congenital lesions resulting from a developmental error of meninges (13). They are most frequently found in the middle fossa with a rate of 50-65%, and it might be explained by the maldevelopment of the Sylvian fissure which is the fusion failure of the arachnoid linings in the frontotemporal lobes (4). Less frequently, ACs are seen in the suprasellar and quadrigeminal cisterns, posterior fossa, cerebral convexities, and interhemispheric fissures (1). ACs have a slight predilection for the left side with male predominance, and they usually asymptomatic (5). Although the natural course of ACs is still under debate, some investigators classified ACs as static or dynamic according to the potential possibility of progressive enlargement (6). There are fewer than 30 cases of AC associated with both intracystic hemorrhage and ipsilateral subdural hematomas, and only 1 case had a visible bleeding focus which was ruptured aneurysm (7). In this paper, we present a rare case of nontraumatic intracystic hemorrhage as complication of AC.
Dyke and Davidoff (5) first reported the hemorrhagic complication of AC in 1938. The first possible mechanism of this event could explained by a tear in the arachnoid membrane, resulting in the rupture of bridging veins, unsupported blood vessels around the cyst wall, and leptomeningeal vessels in the base of the cyst (8). Another mechanism presumably explains that the preexisting AC may enlarge over time as a result of fluid accumulation from the cystic wall, and then the increased internal pressure may cause cystic rupture. Therefore, in this event, AC presents as an extraaxial hematoma with associated vascular disruption (910). In clinical practice, it can be difficult to distinguish ACs from extraaxial hemorrhages because intracystic hemorrhage can mask the preexisting AC on radiologic examinations. The principle treatment for a patient with a hemorrhagic AC is a surgery, including membranectomy and cyst fenestration to adjacent cisterns. To prevent recurrence, wide resection of membrane can be performed.
In the present case, the preexisting AC showed intracystic hemorrhage with no history of head trauma, and the lesion was filled with fresh blood and clots during surgery. Despite of surgical cyst fenestration for preventing complications, residual AC was noted in our patient.
In conclusion, complications of AC may occur spontaneously and these can present the acute life-threatening clinical manifestations. Fortunately, the brisk use of neuroimaging studies such as CT and MR imaging has increased the diagnostic rate of ACs as well as the detection of their possible complications. Therefore, we suggest that clinical awareness of spontaneous intracystic hemorrhage is important to make an accurate radiologic decision in cases with ACs, especially if there is a cyst enlargement on follow-up imaging studies.
Figures and Tables
Fig. 1
A 22-year-old man presented with acute onset severe headache and vomiting. Initial non-enhanced (a) and enhanced (b) brain CT images reveal a hyperdense extraaxial mass in the left middle cranial fossa, suggesting acute hematoma. Intracranial CT angiography (c) shows an upward displacement of the left middle cerebral artery and its branches by the extraaxial hematoma (arrows). And there is no significant vascular derangement in the major intracranial arteries.

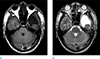
Fig. 2
On follow-up MR imaging after 8 days postoperatively, the intracystic hemorrhage shows a complete resolution on T1-weighted image (a) and T2-weighted image (b). Although cyst fenestration was performed during surgery, residual arachnoid cyst is still noted in the left middle cranial fossa. MR images also reveal small amount of resolving postoperative subdural hemorrhage (early subacute stage) in the left anterior temporal and bilateral occipital convexities.
References
1. Wester K. Peculiarities of intracranial arachnoid cysts: location, sidedness, and sex distribution in 126 consecutive patients. Neurosurgery. 1999; 45:775–779.
2. Sommer IE, Smit LM. Congenital supratentorial arachnoidal and giant cysts in children: a clinical study with arguments for a conservative approach. Childs Nerv Syst. 1997; 13:8–12.
3. Rengachary SS, Watanabe I, Brackett CE. Pathogenesis of intracranial arachnoid cysts. Surg Neurol. 1978; 9:139–144.
4. Cincu R, Agrawal A, Eiras J. Intracranial arachnoid cysts: current concepts and treatment alternatives. Clin Neurol Neurosurg. 2007; 109:837–843.
5. Davidoff LM, Dyke CG. RelapsingJuvenilechronic subdural haematoma: a clinical and roentgenographic study. Bull Neurol Inst NY. 1938; 7:95111.
6. Passero S, Filosomi G, Cioni R, Venturi C, Volpini B. Arachnoid cysts of the middle cranial fossa: a clinical, radiological and follow-up study. Acta Neurol Scand. 1990; 82:94–100.
7. Huang D, Abe T, Kojima K, et al. Intracystic hemorrhage of the middle fossa arachnoid cyst and subdural hematoma caused by ruptured middle cerebral artery aneurysm. AJNR Am J Neuroradiol. 1999; 20:1284–1286.
8. Galassi E, Piazza G, Gaist G, Frank F. Arachnoid cysts of the middle cranial fossa: a clinical and radiological study of 25 cases treated surgically. Surg Neurol. 1980; 14:211–219.
9. Kondziolka D, Bernstein M, ter Brugge K, Schutz H. Acute subdural hematoma from ruptured posterior communicating artery aneurysm. Neurosurgery. 1988; 22:151–154.
10. Ergun R, Okten AI, Beskonakli E, Anasiz H, Ergungor F, Taskin Y. Unusual complication of arachnoid cyst: spontaneous rupture into the subdural space. Acta Neurochir (Wien). 1997; 139:692–694.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download