Abstract
Purpose
Because vesicourethral dysfunction in myelodysplasia patients is a major cause of upper urinary deterioration and urinary incontinence, urodynamic evaluation should be performed as early as possible. We attempted to establish the proper time when videourodynamic study should be performed and which patients require early interventional therapy.
Materials and Methods
Out of the 222 patients seen in the pediatric urology department, 22 patients underwent correction of myeloplasia defect from January 2001 to September 2004. Preoperatively, the patients were assessed with videourodynamic study, and the postoperative videourodynamic studies were repeated at 2 to 6 months intervals. Four urodynamic parameters (bladder volume, compliance, detrusor activity and detrusor sphincteric synergy) were identified, graded and then added to obtain the urodynamic score.
Results
There was no statically significant difference in all urodynamic parameters between the preoperative and postoperative 2 month videourodynamic studies, but a statistically significant difference was noted in compliance between the preoperative and postoperative 6 month videourodynamic studies. The compliance was more decreased in the patients who had received surgical correction in their older age and high detrusor activity was observed for these patients on the preoperative videourodynamic study.
Figures and Tables
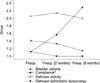 | Fig. 1Statistical analysis of the videourodynamic parameters among the urodynamic studies at different times. *statistically significant between preoperative and postoperatively 6 months. |
References
1. Bauer SB, Koff SA, Jayanthi VR. Walsh PC, Retik AB, Vaughan ED, Wein AJ, editors. Voiding dysfunction in children: neurogenic and non-neurogenic. Campbell's urology. 2001. 8th ed. Philadelphia: Saunders;2231–2281.
2. Kim KS. Kim JC, Kim HJ, Park CH, Oh SJ, Lee KS, Lee JJ, editors. Neurogenic voiding dysfunction in children. Textbook of voiding dysfunction and female urology. 2003. 1st ed. Seoul: Ilchokak;269–281.
3. Han SW. Kim JC, Kim HJ, Park CH, Oh SJ, Lee KS, Lee JJ, editors. Treatment of voiding dysfunction in children. Textbook of voiding dysfunction and female urology. 2003. 1st ed. Seoul: Ilchokak;294–305.
4. Roach MB, Switters DM, Stone AR. The changing urodynamic pattern in infants with myelomeningocele. J Urol. 1993. 150:944–947.
5. Sillen U, Hansson E, Hermansson G, Hjalmas K, Jacobsson B, Jodal U. Development of the urodynamic pattern in infants with myelomeningocele. Br J Urol. 1996. 78:596–601.
6. Meyrat BJ, Tercier S, Lutz N, Rilliet B, Forcada-Guex M, Vernet O. Introduction of a urodynamic score to detect pre- and postoperative neurological deficits in children with a primary tethered cord. Childs Nerv Syst. 2003. 19:716–721.
7. Hjalmas K. Urodynamics in normal infants and children. Scand J Urol Nephrol. 1988. 114:Suppl. 20–27.
8. Norgaard JP, Van Gool JD, Hjalmas K, Djaurhuus JC, Hellstrom AL. Standardization and definitions in lower urinary tract dysfunction in children. Br J Urol. 1998. 81:1–16.
9. Tarcan T, Bauer S, Olmedo E, Khoshbin S, Kelly M, Darbey M. Long term followup of newborns with myelodysplasia and normal urodynamic findings: Is followup necessary? J Urol. 2001. 165:564–567.
10. Kim KM, Jung YJ, Kim DK. Urodynamic evaluation of neurosurgical effect in myelodysplasia. Korean J Urol. 1998. 39:266–270.
11. Fone PD, Vapnek JM, Litwiller SE, Couillard DR, Macdonald CM, Boggan JE, et al. Urodynamic findings in the tethered spinal cord syndrome: Does surgical release improve bladder function? J Urol. 1997. 157:604–609.
12. Vernet O, Farmer JP, Houle AM, Montes JL. Impact of urodynamic studies on the surgical management of spinal cord tethering. J Neurosurg. 1996. 85:555–559.
13. Balkan E, Kilic N, Avsar I, Boyaci S, Aksoy K, Dugruyol H. Urodynamic findings in the tethered spinal cord: the effect of tethered cord division on lower urinary tract functions. Eur J Pediatr Surg. 2001. 11:116–119.
14. Kim KM, Kim KS, Choi H. Urodynamic study in children with myelodysplasia. Korean J Urol. 1992. 33:298–303.
15. Jung JY, Kim KM, Choi H. Urodynamic analysis of incontinence in children with myelodysplasia. Korean J Urol. 2000. 41:521–527.
16. McGuire EJ, Woodside JR, Borden TA, Weiss RM. Prognostic value urodynamic testing in myelodysplastic patients. J Urol. 1981. 126:205–209.
17. Bauer SB, Hallett M, Khoshbin S, Lebowitz RL, Winston KR, Gibson S, et al. Predictive value of urodynamic evaluation in newborns with myelodysplasia. JAMA. 1984. 252:650–652.
18. Hopps CV, Kropp KA. Preservation of renal function in children with myelomeningocele managed with basic newborn evaluation and close follow up. J Urol. 2003. 169:305–308.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download