Abstract
Purpose
Chlormadinone acetate (CMA) therapy for benign prostatic hyperplasia (BPH) may lower the serum prostate specific antigen (PSA) level. However, little is known about the effect of CMA on the total or free serum PSA levels of PSA. Such information would be important since PSA testing is useful for prostate cancer screening. Thus, we prospectively studied the effect of CMA therapy on the total and free serum PSA levels.
Materials and Methods
The patients with lower urinary tract symptoms (LUTS) and BPH who were aged over 50 years were treated with 50mg CMA for 6 months. Men with a PSA level greater than 10ng/ml were excluded to reduce the likelihood of including cases of occult prostate cancer. Those with suspicious findings on the digital rectal examination and serum PSA testing were biopsied to rule out prostate cancer. α-blocking agents were permitted to treat the men with LUTS. Serum levels of the total and free PSA were measured at the study baseline and after approximately 3 and 6 months. The prostate volume (PV) was assessed by transrectal ultrasonography.
Results
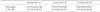
The analysis included 170 patients with a mean age of 67.9 years, a baseline PV of 47.3ml and a baseline total PSA of 4.1ng/ml. The total PSA levels declined from 4.1ng/ml at baseline to 2.0ng/ml after 6 months of treatment (50.7% decrease, p<0.01). The mean percent free PSA (21% to 22% at baseline) was not significantly altered by CMA treatment. The PSA levels and PV at baseline did not affect the rate of decline of PSA.
Figures and Tables
 | Fig. 1Influence of chlormadinone acetate on prostate-specific antigen according to the prostate volume in the men with benign prostatic hyperplasia. |
References
1. Lowe FC, McConnell JD, Hudson PB, Romas NA, Boake R, Lieber M, et al. Long-term 6-year experience with finasteride in patients with benign prostatic hyperplasia. Urology. 2003. 61:791–796.
2. Roehrborn CG, Bruskewitz R, Nickel JC, McConnell JD, Saltzman B, Gittelman MC, et al. Sustained decrease in incidence of acute urinary retention and surgery with finasteride for 6 years in men with benign prostatic hyperplasia. J Urol. 2004. 171:1194–1198.
3. Pannek J, Marks LS, Pearson JD, Rittenhouse HG, Chan DW, Shery ED, et al. Influence of finasteride on free and total serum prostate specific antigen levels in men with benign prostatic hyperplasia. J Urol. 1998. 159:449–453.
4. Guess HA, Gormley GJ, Stoner E, Oesterling JE. The effect of finasteride on prostate specific antigen: review of available data. J Urol. 1996. 155:3–9.
5. Lee SE. Diagnosis of prostate cancer. Korean J Urol. 2004. 45:197–208.
6. Matzkin H, Barak M, Braf Z. Effect of finasteride on free and total serum prostate-specific antigen in men with benign prostatic hyperplasia. Br J Urol. 1996. 78:405–408.
7. Debruyne F, Barkin J, van Erps P, Reis M, Tammela TL, Roehrborn C. Efficacy and safety of long-term treatment with the dual 5 alpha-reductase inhibitor dutasteride in men with symptomatic benign prostatic hyperplasia. Eur Urol. 2004. 46:488–494.
8. Okada H, Kawaida N, Ogawa T, Arakawa S, Matsumoto O, Kamidono S. Tamsulosin and chlormadinone for the treatment of benign prostatic hyperplasia. Scand J Urol Nephrol. 1996. 30:379–385.
9. Shibata Y, Fukabori Y, Ito K, Suzuki K, Yamanaka H. Comparison of histological compositions and apoptosis in canine spontaneous benign prostatic hyperplasia treated with androgen suppressive agents chlormadinone acetate and finasteride. J Urol. 2001. 165:289–293.
10. Murakoshi M, Ikeda R, Fukui N, Nakayama T. Relationship between prostatic atrophy and apoptosis in the canine spontaneous benign prostatic hyperplasia (BPH) following chlormadinone acetate (CMA). Tokai J Exp Clin Med. 2001. 26:71–75.
11. Harada M, Kinoshita M, Moriyama M, Kondo I, Nakahashi M, Kumagai H, et al. Histological evaluation of benign prostatic hyperplasia treated by long-term administration of chlormadinone acetate (CMA). Prostate. 1994. 25:147–155.
12. Gormley GJ, Stoner E, Bruskewitz RC, Imperato-McGinley PC, Walsh PC, McConnell JD, et al. The effect of finasteride in men with benign prostatic hyperplasia. N Engl J Med. 1992. 327:1185–1191.
13. Brawer MK, Lin DW, Williford WO, Jones K, Lepor H. Effect of finasteride and/or terazosin on serum PSA: results of VA Cooperative Study #359. Prostate. 1999. 39:234–239.
14. Balk SP, Ko YJ, Bubley GJ. Biology of prostate-specific antigen. J Clin Oncol. 2003. 21:383–391.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download