Abstract
Purpose
Postoperative wound infection accounts for approximately 15% of all hospital infections. Methicillin-resistant Staphylococcus aureus (MRSA) infections are 14% of the domestic hospital infections and this is increasing in incidence over time. The aim of this study was to retrospectively evaluate the relationship between wound dehescence after urologic surgery and MRSA infection.
Materials and Methods
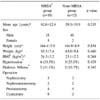
Thirty patients (25 males and 5 females) who experienced wound dehescence after urologic surgery were subdivided into two separate groups; the MRSA group and non-MRSA group, and they were retrospectively analyzed via a chart review according to the age of the patients, the associated disease, the hepatic or renal functional status, the admission duration, the use of preoperative antibiotics and the number and duration of inserted catheters.
Results
The mean age of the MRSA group and the non-MRSA group was 62.6±12.4 years and 59.3±19.9 years, respectively (p=0.235). The elapsed operative time in the MRSA group and non-MRSA group was 355.8±99.5 minutes and 305.8±90.2 minutes, respectively (p=0.021). Contrary to 35.2±23.6 days of catheter duration in the MRSA group, that of the non-MRSA group was 14.6±8.5 days (p=0.007). The tendency for MRSA infection was observed for an increased duration of drain placement, a decreased hepatic or renal function and the preoperative antibiotic use. The extent of admission was obviously longer for the MRSA group (39.6±23.5 days) than for the non-MRSA group (28.9±9.9 days) (p=0.013).
References
1. Heinzelmann M, Scott M, Lam T. Factors predisposing to bacterial invasion and infection. Am J Surg. 2002. 183:179–190.
2. Ericsson CD, Duke JH Jr, Pickering LK. Clinical pharmacology of intravenous and intraperitoneal aminoglycoside antibiotics in the prevention of wound infections. Ann Surg. 1978. 188:66–70.
3. Ridgeway S, Wilson J, Charlet A, Kafatos G, Pearson A, Coello R. Infection of the surgical site after arthroplasty of the hip. J Bone Joint Surg Br. 2005. 87:844–850.
4. Dodds Ashley ES, Caroll DN, Engemann JJ, Harris AD, Flowler VG Jr, Sexton DJ, et al. Risk factor for postoperative mediastinitis due to methicillin-resistant staphylococcus aureus. Clin Infect Dis. 2004. 38:1555–1560.
5. Kim HS, Park CK. Clinical observation of the postoperative wound infection. J Korean Surg Soc. 1988. 35:271–282.
6. Nasim A, Thompson MM, Naylor AR, Bell PR, London NJ. The impact of MRSA on vascular surgery. Eur J Vasc Endovasc Surg. 2001. 22:211–214.
7. Nosocomial Infection Surveilance Committee of the Korean Society for Nosocomial Infection Control. 1996 National nosocomial infection surveillance in Korea. KOSNIC. 1997. 2:157–176.
8. Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999 Hospital Infection Control Practice Advisory Committee. Infect Control Hosp Epidemiol. 1999. 20:250–278.
9. Barber M. Methicillin-resistant Staphylococci. J Clin Pathol. 1961. 14:385–393.
10. Morgan M, Evans-Williams D, Salmon R, Hosein I, Looker DN, Howard A. The population impact of MRSA in a country: the national survey of MRSA in Wales, 1997. J Hosp Infect. 1997. 44:227–239.
11. Peltroche-Llacsahuanga H, Haase G, Lutticken R. Methicillin-resistant Staphylococcus aureus (MRSA) - clinical implications. Chirurg. 1998. 69:801–805.
12. Weed HG. Antimicrobial prophylaxis in the surgical patients. Med Clin North Am. 2003. 87:59–75.
13. Polk HC Jr. Postoperative wound infection: prediction of some responsible organisms. Am J Surg. 1973. 126:592–594.
14. Samad A, Banerjee D, Carbarns N, Ghosh S. Prevalence of methicillin-resistant Staphylococcus aureus colonization in surgical patients, on admission to a Welsh hospital. J Hosp Infect. 2002. 51:43–46.
15. Davis NC, Cohen J, Rao A. The incidence of surgical wound infection: a prospective study of 20,822 operations. Aust N Z J Surg. 1973. 43:75–80.
16. Robson MC, Steed DL, Franz MG. Wound healing: biologic features and approaches to maximize healing trajectories. Curr Probl Surg. 2001. 38:72–140.
17. Lister J, Herschfeld JJ. Joseph Lister and the principle of antiseptic surgery. 1867. Bull Hist Dent. 1988. 36:120–126.
18. Todd JC. Wound infection: etiology, prevention, and managementm including selection of antibiotics. Surg Clin North Am. 1968. 48:787–798.
19. KOSNIC Health Technology Project Team. Prospective estimation of extra health care costs and hospitalization due to surgical infection in Korean hospital. KOSNIC. 1999. 4:193–204.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download