Abstract
Purpose
The recent development of posterior intravaginal slingplasty (IVS) has led to significant changes for the treatment of vaginal vault or uterine prolapse. We analyzed the efficacy of performing posterior IVS for the patients with vaginal vault and uterine prolapse.
Materials and Methods
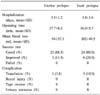
This study analyzed the treatment outcomes of 56 patients with vaginal vault or uterine prolapse and these patients were seen at our hospital from March 2004 to August 2005. The degree of prolapse was classified according to the POP-Q system. The grades were 17 cases of stage 2, 8 cases of stage 3 and 5 cases of stage 4 in the vaginal vault prolapse group, and 14 cases of stage 2, 6 cases of stage 3 and 6 cases of stage 4 in the uterine prolapse group.
Results
Fifteen cases in the vaginal vault prolapse group and 9 cases in the uterine prolapse group received combined tension-free vaginal tape (TVT) or the tension-free vaginal tape obturator system (TVT-O). The patients who received combined rectocele repair were 17 cases in the vaginal vault prolapse group and 17 cases in the uterine prolapse group. The mean operation time was 37 minutes and the mean bleeding volume was 94ml. The mean admission period was 3.5 days and the mean follow-up time was 9.5 months (1-17). Polypropylene tape was used for 56 patients without any rejection reactions or rectal perforation. Among the 30 patients operated on for vaginal vault prolapse, 24 patients were cured and 6 patients showed improvement. Among the 26 patients operated on for uterine prolapse, 23 patients were cured and 3 patients showed improvement.
Figures and Tables
 | Fig. 2The tape is inserted through the levator muscle complex and it is attached at only the insertion points of the uterosacral ligament into the vagina. T: tape, V: vagina, PS: pubic symphysis, B: bladder, R: rectum, S: sacrum, USL: uterosacral ligament, CL: cardinal ligament. Reproduced with the permission of professor Peter Petros. |
References
1. Nichols DH. Rock JA, Thomson JD, editors. Central compartment defect. TeLine's operative gynecology. 1997. 8th ed. Philadelphia: Lippincott-Raven;1006–1030.
2. Petros PE. Vault prolapse II restoration of dynamic vaginal supports by infracoccygeal sacropexy, an axial day-case vaginal procedure. Int Urogynecol J Pelvic Floor Dysfunct. 2001. 12:296–303.
3. Petros PE. New ambulatory surgical methods using an anatomical classification of urinary dysfunction improve stress, urge and abnormal emptying. Int Urogynecol J Pelvic Floor Dysfunct. 1997. 8:270–277.
4. Deval B, Haab F. What's new in prolapse surgery? Curr Opin Urol. 2003. 13:315–323.
5. Cruikshank SH. Sacrospinous fixation-should this be performed at the time of vaginal hysterectomy? Am J Obstet Gynecol. 1991. 164:1072–1076.
6. Karram M, Goldwasser S, Kleeman S, Steele A, Vassallo B, Walsh P. High uterosacral vaginal vault suspension with fascial reconstruction for vaginal repair of enterocele and vaginal vault prolapse. Am J Obstet Gynecol. 2001. 185:1339–1342.
7. Richter K. Massive eversion of the vagina: pathogensis, diagnosis, and therapy of the "true" prolapse of the vaginal stump. Clin Obstet Gynecol. 1982. 25:897–912.
8. Sundaram CP, Venkatesh R, Landman J, Klutke CG. Laparoscopic sacrocolpopexy for the correction of vaginal vault prolapse. J Endourol. 2004. 18:620–623.
9. Farnsworth BN. Posterior intravaginal slingplasty (infracoccygeal sacropexy) for severe posthysterectomy vaginal vault prolapse-a preliminary report on efficacy and safety. Int Urogynecol J Pelvic Floor Dysfunct. 2002. 13:4–8.
10. Lee KS, Choi YS, Kim JC, Lee JY, Choo MS. Initial clinical experience of posterior intravaginal slingplasty for uterine and vaginal vault prolapse. Korean J Urol. 2004. 45:Suppl 2. 119.
11. Kim DY, Kim IK, Choi S. Initial results of posterior intravaginal slingplasty for patients with vaginal vault prolapse. J Korean Continence Soc. 2004. 8:Suppl. 90.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download