Abstract
Osteonecrosis (ON) is a common comorbidity in gout; however, avascular ON of multiple sites is unusual. Multifocal ON is defined as osteonecrotic lesions affecting three or more separate anatomic sites. We report a case of a 31-year-old woman diagnosed with gout, who had multifocal ON. Initially, she was treated with benzbromarone, colchicine, and meloxicam. Two years later, she developed severe tophi and was diagnosed with chronic renal failure. Magnetic resonance imaging (MRI) of both legs revealed bilateral ON of the femoral head. She underwent bilateral hip replacement surgeries. After two years, she had pain and limited movements in the left shoulder, with tophi identified via dual-energy computed tomography. Despite management with non-steroidal anti-inflammatory drugs, colchicine, and prednisolone, she had persistent shoulder pain. MRI of the left shoulder revealed ON. She therefore underwent left shoulder replacement surgery. Following the case report, we review the literature on multifocal ON with gout.
Osteonecrosis (ON) is believed to be caused by ischemia of the juxta-articular bone. Multifocal ON is defined as a disease affecting three or more joints, with overall incidence of ~3% among patients diagnosed with ON [1]. Common comorbidities associated with multifocal ON include systemic lupus erythematosus, renal disorders, inflammatory bowel disorder, and coagulopathies [1].
Gout has been associated with cardiovascular and renal diseases. Previous evidence on these associations and those involving other comorbidities such as metabolic syndrome have emerged and have been established to explain the importance of asymptomatic hyperuricemia [2].
However, multifocal ON in patients with gout has not been reported in Korea. We present a case of a 31-year-old woman diagnosed with gout, who had multifocal ON involving three joints (both hip joints and left shoulder joint), with a review of the literature.
A 31-year-old woman was diagnosed with gout, alcoholic hepatitis, and medullary nephrocalcinosis in December 2008 when she presented with acute erythematous swelling in the right great toe. At this time, there were no femoral lesions on plain radiographs. She did not visit our hospital after treatment, but visited in June 2009 because of recurrent gout attacks and large multiple tophi on both hands (Figure 1A, B). She started taking benzbromarone 50 mg, colchicine 0.6 mg, and meloxicam 7.5 mg daily, but continuously consumed 100 mL of alcohol twice a week. She had intermittent acute gout flares and then developed multiple tophi on both hands and feet. She gradually experienced left hip pain, tenderness, and limitations in her movements. Her motor and sensory functions were normal, and the dorsalis pedis pulse of both lower extremities was intact. Unfortunately, left hip radiograph showed collapsed femoral head and joint space narrowing (Figure 2A). The left hip replacement surgery was conducted in December 2009. We observed multifocal areas of periarticular gouty tophi causing fibrosis and degeneration in the surgical biopsy specimens of the left hip joint (Figure 2B). She had the right hip replacement surgery due to ON in August 2010 (Figure 2C).
From December 2010, she had mild left shoulder pain; active left shoulder arthritis on the bone scan images and inhomogeneous sclerotic change in the left humeral head on the shoulder radiographs were detected (Figure 3A). Further, uric acid deposition in the left acromion was observed on the dual-energy computed tomography (DECT) image (Figure 3B).
Because she had severe hyperuricemia (13.9 mg/dL), she was treated with methylprednisolone and naproxen initially, and then with a maintenance treatment with febuxostat, low dose prednisolone and naproxen, under the diagnosis of acute gout flare. Pain was alleviated with rest initially, but did not improve adequately with rest or medication.
Her left shoulder pain, which had an insidious onset and was slowly progressive, became severe, and she could not elevate her left arm. There was no history of trauma, radiation exposure, unexplained fever, skin lesions, bleeding tendency, and thrombophlebitis. Her physical examination revealed restriction of the left shoulder motions in all ranges with no abnormal neurologic signs on both extremities. Her radial pulse was normal.
After the acute stage, the results of the complete blood cell count and peripheral blood smear showed mild macrocytic anemia (hemoglobin, 9.9 g/dL) probably due to chronic liver disease. She had normal white blood cell and platelet counts, activated partial thromboplastin time, and prothrombin time. The erythrocyte sedimentation rate and C-reactive protein level were also normal. She also had normal aspartate aminotransferase/alanine aminotransferase and uric acid levels but elevated blood urea nitrogen (BUN)/creatinine levels (BUN, 50.7 mg/dL; creatinine, 2.14 mg/dL). Since 2011, she had hyperlipidemia (total cholesterol, 337 mg/dL; triglyceride, 499 mg/dL; high density lipoprotein, 46 mg/dL; and low density lipoprotein, 195 mg/dL). Serologic test results for human immunodeficiency virus, herpes simplex virus, Epstein-Barr virus, and cytomegalovirus were negative. The work-up for autoimmune diseases showed negative results for anti-nuclear antibody and anti-neutrophil cytoplasmic antibody and a mild elevation in the rheumatoid factor level (RF, 10.2 IU/mL).
Thus, we performed MRI on her left shoulder to evaluate possible aggravations of ON. Expectedly, we found an advanced avascular necrosis of the humeral head (Figure 3C and 3D). Finally, she underwent a left shoulder replacement surgery.
She had a maintenance treatment with febuxostat 40 mg and benzbromarone 50 to 100 mg daily and has remained stable without further complications for 4 years.
ON refers to the cellular death of bone components due to interruptions in the blood supply, resulting in pain, bone destruction, and loss of function [3]. The hip joint is the site most commonly affected by multifocal ON, followed by the knee, shoulder, ankle, elbow, and wrist. Bilaterality is common, including 98% of the affected hips, 87% of the affected knees, and 83% of the affected shoulders [1]. It is generally agreed that the disease would involve bilateral hips in more than 50% of the cases at the time the diagnosis was established, and 50% of them would progress to the advanced stage within 3 years and require major surgical procedures [45]. Our patient had a definite ON affecting three anatomical sites (both hip joints and left shoulder joint), and a bone scan of both knees had a negative result (data not shown). Thus, the features were typical of a multifocal ON.
The Collaborative ON Group Study confirmed that steroids are the primary cause of multifocal ON in 91% of the cases [1]. The duration of corticosteroid therapy, total cumulative dose, and highest daily dose have been independently associated with the development of ON [6]. Our patient also took prednisolone intermittently during acute flare-ups of gouty arthritis; however, the dose was too low to induce ON, and she already had ON in the left hip joint before taking therapeutic doses of steroid.
Further, alcohol abuse (>400 mL per week) is considered as another major risk factor of ON attributed to bone marrow stem cells or lipid metabolism abnormalities. Patients with alcohol-induced ON were significantly older than patients with idiopathic ON (average age, 49 years vs. 40 years), were men (97%), and presented with collapsed femoral heads (90%) [7]. Chronic alcohol intake is a common cause of ON; however, multifocal ON is relatively rare. In 1990, Orlić et al. [8] reported an incidence of ON in 5.3% of alcoholics, with 6.1% of these being multifocal. In our case, the patient consumed up to 200 mL of alcohol per week. Although she had a history of alcohol abuse and alcoholic hepatitis, her alcohol abuse was controlled to <200 mL of alcohol per week, after her neuropsychiatric admission in 2007. Her abdominal X-ray in 2008 showed a normal shape of both hip joints.
With these, it is difficult to conclude that both steroid use and alcohol abuse are the main causes of the multifocal ON in our patient. Maybe steroid use and alcohol ingestion had some synergistic effects on gout-induced degeneration and ON. Moreover, blood examination showed no abnormalities, including autoantibodies levels and clotting profile, hemoglobinopathies, and viral infections. She also did not have a history of dive, inborn error of metabolism, pancreatitis, pregnancy, radiation, smoking, and thrombophlebitis. Although she had hyperlipidemia, lipid levels were not sufficient to cause severe multifocal ON. However, we could identify that she had frequent and large variations in her uric acid level during the long-term follow-up. Further, tophi-induced degenerations in the hip joint were observed during operation, and the biopsy specimen and uric acid deposition in the left shoulder via DECT were also checked. These findings indicated that the main cause of the multifocal ON in our patient was gout.
In 1955, Mauvoisin and colleagues [9] were the first to report the occurrence of avascular necrosis of the femoral head in a patient with clinical gout. Subsequently, a number of authors have reported an increased incidence of gout and/or hyperuricemia in patients with femoral head necrosis [10]; however, multifocal ON is relatively rare.
The causes of ON include interruption of the vascular supply as a result of local trauma or non-traumatic systemic conditions [3]. The epidemiology of ON suggests that the pathogenesis is multifactorial. Kenzora [11] introduced the concept of accumulative cell stress theory. He postulated that when multiple stress factors are present, the osteocytes are unable to recover from chronic damage, become overwhelmed, and die. This theory stems from epidemiologic data that show a higher rate of steroid-induced ON in systemically ill patients. The incidence of ON when steroids, which are the most common agent of ON, are the only triggering factor present is low.
Our patient also had multifocal etiologies, not only hyperuricemia/gout but also steroid use, alcohol ingestion, hyperlipidemia, and chronic renal failure, which can damage the cells of many organ systems; these are factors influencing the accumulated stress of the osteocytes. Because of multiple triggers, the osteocytes may become more distressed, which appears to be acute gout flares; steroid administration produces the overwhelming stress, leading to irreversible damages and cell death. The exact mechanism of cell stress may involve direct toxic effects of “poisons” in the body, such as alcohol or uric acid, in addition to indirect stresses, such as steroids, that affect the osteocytes by altering the lipid metabolism or by causing bone cell death.
Pain is usually the presenting symptom. It may be mild initially or vague in cases of insidious onsets when the diagnosis is not suspected. Range of motion is well preserved at the beginning of the disease, but gradually deteriorates. In symptomatic patients, ON has been traditionally diagnosed using conventional radiographs and radionuclide bone scans. MRI has been proven a more sensitive tool for detecting ON at earlier stages and in asymptomatic locations. Despite the technological improvements in diagnostic radiology, detection of ON remains difficult owing to the lack of early clinical symptoms. As with many other insidious diseases, anticipation and vigilance can help detect patients who may be experiencing this “silent” disease [3].
The natural history of ON is variable but is dependent primarily on the size of the infarcted segment and the site of occurrence with a high morbidity and disability. By the time the condition of a patient progresses to end-stage ON, hemiarthroplasty or total replacement may be the only therapeutic option. Because ON occurs mainly in young patients who are generally very active and the treatment options for advanced diseases are limited, the importance of early diagnosis and assessment of populations at risk should be emphasized. If we can detect ON in the early stage, we can use non-operative treatments, such as bisphosphonates, vasodilators, and statins, and less invasive operative treatments, such as core decompression and osteotomy.
Thus, physicians should consider the possibility of ON in patients with gout who have complaints of insidious onset, slowly progressive pain in the hip, knee, and shoulder over a period which was relieved by rest initially but became nonresponsive to rest or medication; further, physicians should also check and perform suitable imaging studies.
Gout has been associated with cardiovascular and renal diseases. However, the multifocal ON in our patient with gout is the first case reported in Korea. We wish to share our experience on the patient who had multifocal ON in the hip and shoulder as an unusual presentation with gout treated with joint replacement surgeries. In patients with gout, all symptomatic joints with progressive pain should be evaluated via radiographs with suspicion of ON.
Figures and Tables
Figure 1
(A) Multiple tophi on both hands (arrows). (B) Dualenergy computed tomography image demonstrating uric acid deposits (green color) on the proximal interphalangeal joints of the right hand.

Figure 2
(A) Anteroposterior hip radiograph showing osteonecrosis of the left hip joint. The left hip joint shows a collapsed femoral head and joint space narrowing compared with the right hip joint (Ficat Stage IV). (B) Intra-operative left hip joint image showing a gout tophi-induced degeneration (arrow). (C) Anteroposterior hip radiograph showing osteonecrosis of the right hip joint.

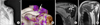
Figure 3
(A) Anteroposterior left shoulder joint radiograph showing a collapsed deformity with inhomogeneous sclerotic changes in the left humeral head. (B) Dual-energy computed tomography image showing a uric acid deposition in the left acromion. (C) T2-weighted magnetic resonance image of the left shoulder joint. High signal intensity in the humeral head (arrows) suggests a necrotic area. Multiple rounded and oval nodular lesions in the glenohumeral joint with dark signal intensity in all sequences indicate osteophytes (arrowheads). The findings are suggestive of advanced stage of avascular necrosis of the humeral head (Ficat Stage III). (D) T1-weighted magnetic resonance image showing a low signal intensity (arrows), which suggests.
References
1. Symptomatic multifocal osteonecrosis. A multicenter study. Collaborative Osteonecrosis Group. Clin Orthop Relat Res. 1999; (369):312–326.
2. Sattui SE, Singh JA, Gaffo AL. Comorbidities in patients with crystal diseases and hyperuricemia. Rheum Dis Clin North Am. 2014; 40:251–278.
3. Assouline-Dayan Y, Chang C, Greenspan A, Shoenfeld Y, Gershwin ME. Pathogenesis and natural history of osteonecrosis. Semin Arthritis Rheum. 2002; 32:94–124.
4. Choi IH, Pizzutillo PD, Bowen JR, Dragann R, Malhis T. Sequelae and reconstruction after septic arthritis of the hip in infants. J Bone Joint Surg Am. 1990; 72:1150–1165.
5. Li W, Fan Q, Ma B, Ren M, Li H, Gou Y, et al. [An animal model of Perthes disease and an experimental research of VEGF expression]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2008; 22:814–819.
6. Calvo-Alén J, Alarcón GS, Tew MB, Tan FK, McGwin G Jr, Fessler BJ, et al. Systemic lupus erythematosus in a multiethnic US cohort: XXXIV. Deficient mannose-binding lectin exon 1 polymorphisms are associated with cerebrovascular but not with other arterial thrombotic events. Arthritis Rheum. 2006; 54:1940–1945.
7. Zsernaviczky J, Dressler D. [Gout, pseudo-gout or hyperlipoproteinemia? (author's transl)]. Z Orthop Ihre Grenzgeb. 1976; 114:243–247.
8. Orlić D, Jovanović S, Anticević D, Zecević J. Frequency of idiopathic aseptic necrosis in medically treated alcoholics. Int Orthop. 1990; 14:383–386.
9. Mauvoisin F, Bernard J, Gemain J. Tomographic aspects of the hips in gout. Rev Rhum Mal Osteoartic. 1955; 22:336–337.
10. Mielants H, Veys EM, DeBussere A, van der Jeught J. Avascular necrosis and its relation to lipid and purine metabolism. J Rheumatol. 1975; 2:430–436.
11. Kenzora JE. Ischemic necrosis of femoral head. Part I. Accumulative cell stress: a hypothesis for the etiology of idiopathic osteonecrosis. Instr Course Lect. 1983; 32:242–252.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download