Abstract
Hematologic malignancies and lymphoproliferative disorders have been reported after using tumor necrosis factor-α inhibitor in patients suffering from spondyloarthropathy. Previously reported cases were treated by using infliximab and etanercept. Usually, it takes approximately several months for leukemia or lymphoproliferative disorders to occur after the application of those agents. However, we report a case of acute myeloid leukemia that developed after short term usage of adalimumab in a patient suffering from psoriatic arthritis.
Psoriasis mainly contains erythematous and scaled skin manifestation, and is a chronic inflammatory disease that could target joints. In psoriatic arthritis, symptoms of arthritis and skin lesions can be improved by prescribing tumor necrosis factor-α (TNF-α) inhibitor. Psoriasis occasionally leads to skin cancer or lymphoproliferative disorder. However, there have been no cases described that led to acute myeloid leukemia (AML) after application of adalimumab in patient of psoriatic arthritis, while some cases of AML have been reported which occurred to patient of juvenile rheumatoid arthritis who received adalimumab. We report a 45 year-old man who developed AML after receiving adalimumab for three months, as the patient did not show response to conventional therapy to treat psoriatic arthritis.
A 45 year-old male patient who had erythematous and scaled skin lesions on his scalp for three years was treated under the impression of seborrheic dermatitis for 1 year. About two years ago, this patient began to suffer from polyarthralgia.
At that time, rheumatoid factor, anti-cyclic citrullinated peptide antibody and all anti-extractable nuclear antigen antibodies showed negative results except one positive result of FANA, for which the titer was 1:200 and was of a speckled type. In addition, the skin lesions revealed the psoriatic pattern.
There was no swelling and tenderness at the painful spots of polyarthralgia nor were there any unusual findings in physical examination. However, increased erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) were observed in the laboratory data. Enthesopathy were detected by the bone scan and minimal sclerosis at the left side was viewed on plain film of sacroiliac joint (Fig. 1).
The patient was diagnosed to have psoriatic arthritis by proving psoriasis based on the skin biopsy. After medicines such as non-steroidal anti-inflammatory drugs, methotrexate, prednisolone, and hydroxychloroquine were prescribed, symptoms including arthralgia improved.
Although back pain improved, regions of arthralgia increased and laboratory data revealed increase in ESR, CRP after nine months of prior treatment. Subsequently adalimumab was prescribed 40 mg every other week. Following that, polyarthralgia pain diminished, and psoriatic skin lesion reduced in size. Along with improved symptoms, ESR and CRP decreased.
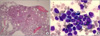
After three months from initial adalimumab application, the patient complained of dry cough. On physical examination, the breathing sound was clear. Imaging studies and laboratory data which included complete blood cell count (CBC), blood chemistries were done. Mild leukocytosis and increased ESR and CRP were observed. On chest X-ray and computed tomography, pneumonia on left lower lobe was discovered. Adalimumab and methotrexate were then stopped as pneumonia was detected, and instead, antibiotic treatment was administered. It took two weeks to cure pneumonia. After 5 weeks from discharge, anemia and 2% of immature cell were detected on laboratory finding of peripheral blood (PB) smear. Thereafter the patient was transferred to our hospital for a medical examination analyzing hematologic malignancy. On physical examination, there were no abnormal finding except swelling of right hand. Chest X-ray was taken, and lung parenchyma displayed no pneumonic infiltration. He was diagnosed with myeloblastic leukemia with maturation from bone marrow biopsy examination (Fig. 2). Chromosome analysis of bone marrow showed its abnormality of t(6;9) and t(10;16) (Fig. 3). He took chemotherapy with the prescribed idarubicin, enocitabine regimen. Neutropenia developed after chemotherapy and the patient expired by sepsis. Sepsis was initiated three weeks from initial chemotherapy.
TNF-α inhibitors are used not only for rheumatic disease but also for remission of inflammatory bowel disease and psoriasis in dermatology and gastroenterology areas. In these fields, some cases of TNF-α inhibitors-related-leukemia have been reported (1-6).
Even in these cases, leukemia appeared at least three months after treating with TNF-α inhibitor in patient who did not respond to conventional therapy. The points to be considered in this case are the following: the history of underlying psoriasis, the treatment by adalimumab, as well as its dosage and duration. A compounding problem in interpreting the relationship between the malignancy and TNF-α inhibitors is that psoriatic arthritis itself can cause malignancy regardless of TNF-α inhibitors. Until nowadays, data of dosage and duration about adalimumab-related-malignancy were not accumulated enough. One study analysed malignancies related to TNF α inhibitors, especially about infliximab and etanercept. In this study, the median time to diagnose malignancy from the start of infliximab was thirty months and the median time to diagnose malignancy from start of etanercept was twenty eight months (7).
On the basis of other studies, patients with rheumatoid arthritis were at an increased risk of lymphoma and leukemia with the standardized incidence ratio of 2.0 and 2.2, respectively (8). Uncommonly, ankylosing spondylitis accompanies hematologic malignancy. In particular, there are some cases that were accompanied by leukemia. Also, the hypothesis that HLA-B27 contributes to pathogenesis of those malignancies exists (9). In psoriasis, skin cancer and lymphoproliferative disorder are the two most commonly associated malignancies. In one study, patients of acute leukemia who already had underlying psoriasis experienced hypergranular promyelocytic leukemia as the most common type of AML in the group (10).
In other studies about malignancies which appeared after prescribing TNF-α inhibitor, malignancies associated with adalimumab were rarely reported. One case of hepatosplenic T cell lymphoma was reported which occurred after eight months of adalimumab usage to patient of ulcerative colitis (7). Not enough data has been collected to prove whether or not adalimumab causes leukemia due to its recent assimilation to mainstream drugs such as inflixmab or etanercept.
According to a systematic review and meta-analysis, the malignancies are significantly more common in patients treated with higher doses of TNF-α inhibitors than in patients who received lower doses (11).
Several chemotherapy agents such as alkylating agents and topoisomerase agents can cause therapy-related leukemia. Many hermatologic malignancies associated with chemotherapy commonly occur within 2 to 10 years after initiation of the treatment (12,13). However, in cases of TNF-α inhibitors-associated-leukemia, most of them have been reported within several months after the usage of those agents (2-6).
The most prevalent type of AML associated with psoriasis is hypergranular promyelocytic leukemia with chromosome abnormality on t(15:17). Unexpectedly in our case, AML was found only three months after application of adalimumab and AML with chromosome abnormalities were found on t(6:9) and t(10:16). Therefore, despite the short period of treatment, adalimumab may have contributed to the occurrence of AML. We propose the hypothesis that adalimumab could contribute to promote AML in patients who have psoriatic arthritis.
So far, the mechanism of possible promotion of leukemia by TNF-alpha is not well understood. There were no laboratory or imaging tools which could distinguish between the causes of leukemia; whether it developed as the natural course of underlying disease, the side effect of TNF- inhibitors, or de novo.
Figures and Tables
Figure 1
Bone scan shows multiple enthesopathy at the site of the left elbow, the lesser trochanters of both femurs, the right knee, and both ankles. Sacroiliac joint plain film indicates minimal sclerosis on the left upper side (white arrow). However, there was no definite joint space widening or erosion.

References
1. Saba NS, Kosseifi SG, Charaf EA, Hammad AN. Adalimumab-induced acute myelogenic leukemia. South Med J. 2008. 101:1261–1262.
2. Cesarini M, Vernia P, Angelucci E. Acute lymphoid leukemia in a Crohn's disease patient during treatment with adalimumab after a prolonged treatment with azathioprine and steroids. Inflamm Bowel Dis. 2010. 16:371–372.
3. Alcaín G, Andrade RJ, Queipo de Llano MP, Moreno MJ, García-Cortés M, Franquelo E. Acute leukemia after infliximab therapy. Am J Gastroenterol. 2003. 98:2577.
4. Nair B, Raval G, Mehta P. TNF-α inhibitor etanercept and hematologic malignancies: report of a case and review of the literature. Am J Hematol. 2007. 82:1022–1024.
5. Balato A, Lembo S, Cirillo T, Megna M, Raimondo A, Di Costanzo L. Anti-Tumor Necrosis Factor-α Therapy in the Management of Psoriasis and B-Chronic Lymphocytic Leukemia. Case Rep Dermatol. 2011. 3:60–63.
6. Bachmeyer C. Etanercept therapy and acute myeloid leukemia. Am J Hematol. 2008. 83:345.
7. Diak P, Siegel J, La Grenade L, Choi L, Lemery S, McMahon A. Tumor necrosis factor α blockers and malignancy in children: forty-eight cases reported to the Food and Drug Administration. Arthritis Rheum. 2010. 62:2517–2524.
8. Askling J, Fored CM, Baecklund E, Brandt L, Backlin C, Ekbom A, et al. Haematopoietic malignancies in rheumatoid arthritis: lymphoma risk and characteristics after exposure to tumour necrosis factor antagonists. Ann Rheum Dis. 2005. 64:1414–1420.
9. Au WY, Hawkins BR, Cheng N, Lie AK, Liang R, Kwong YL. Risk of haematological malignancies in HLA-B27 carriers. Br J Haematol. 2001. 115:320–322.
10. Wang Y, Mi Y, Li D, Xue Y, Bian S, Wang J. Acute leukemia association with psoriasis: a report on 100 patients from a single center in China. Am J Hematol. 2010. 85:378–379.
11. Bongartz T, Sutton AJ, Sweeting MJ, Buchan I, Matteson EL, Montori V. Anti-TNF antibody therapy in rheumatoid arthritis and the risk of serious infections and malignancies: systematic review and meta-analysis of rare harmful effects in randomized controlled trials. JAMA. 2006. 295:2275–2285.
12. Ando M, Narabayashi M, Watanabe T, Kamiya Y, Togitani K, Tanosaki R, et al. Therapy-related leukemia and myelodysplastic syndrome in breast cancer patients treated with cyclophosphamide or anthracyclines. Jpn J Clin Oncol. 1999. 29:28–32.
13. Jang GD, Kim SW, Suh CW, Kim EK, Bahng HS, Jeong YH, et al. A case of treatment-related myelodysplastic syndrome and acute myelogenous leukemia following high-dose chemotherapy with autologous stem cell transplantation for non-Hodgkin's lymphoma. J Korean Med Sci. 2002. 17:555–559.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download