Introduction
Henoch-Schönlein purpura (HSP), a systemic vasculitis, usually manifests as a combination of purpuric rash, arthritis/arthralgia, renal disease, and gastrointestinal symptoms. Gastrointestinal symptoms occur in about half of children with HSP and range from mild (nausea, vomiting, abdominal pain, and transient paralytic ileus) to more significant (gastrointestinal hemorrhage, bowel ischemia and necrosis, intussusceptions, and bowel perforation) (1,2). Acute pancreatitis may be a rare complication of HSP. It tends to develop during the first week of the illness after characteristic palpable purpura (3-6), but may develop as an initial presenting feature before or at the same time as the typical rash (7-12). We describe here a patient with acute pancreatitis as a complication of adult HSP. To our knowledge, this is the first such case reported in Korea.
Case Report
A 52-year-old man was hospitalized in a tertiary medical center in December 2010 with a three day history of bilious vomiting and colicky abdominal pain. Ten days prior to admission, he had pain and swelling of both ankles and an erythematous purpuric rash over his upper and lower extremities. There was no history of trauma, medication, chronic illness, or current alcoholic intake, and his family history was unremarkable.
On physical examination the patient was acutely ill, with a body temperature of 36.4℃, a blood pressure of 130/80 mmHg, and a pulse rate of 70 beats/min. He had a purpuric rash, consisting of petechiae and macules, located over upper and lower extremities (Fig. 1), and mild tenderness and swelling of both ankles. Abdominal examination showed tenderness in all quadrants, particularly the epigastric area, but no rigidity or rebound tenderness. There was no hepatosplenomegaly, and bowel sounds were decreased. He had a pretibial pitting edema (+2).
Blood workup showed a hemoglobin concentration of 14.2 g/dL, a white cell count of 16,200/uL, and a platelet count of 493,000/uL. His C-reactive protein concentration was 5.74 mg/dL (normal range, 0~0.6 mg/dL). Serum testing showed glucose 136 mg/dL, urea 26 mg/dL, creatinine 1.4 mg/dL (normal range, 0.7~1.4 mg/dL), calcium 8.0 mg/dL, total cholesterol 160 mg/dL, and triglycerides 145 mg/dL. His serum albumin concentration was quite low, at 1.8 g/dL, and his serum amylase and lipase concentrations were high, at 3,093 U/L (normal range, 30~110 U/L) and 4,063 U/L (normal range, 22~51 U/L), respectively. His serum alanine aminotransferase (103 IU/L), aspartate aminotransferase (128 IU/L), total bilirubin (2.2 mg/dL), and direct bilirubin (1.2 mg/dL) concentrations were higher than normal. Urinary sediment examination showed microscopic hematuria and proteinuria. A 24 hour urine collection showed that his albuminuria had reached the levels of nephrotic syndrome (4.9 g/24 hr). His serum IgA concentration (331 mg/dL) was within the normal range (70~400 mg/dL). He was negative for rheumatoid factor, antinuclear antibodies, and antineutrophil cytoplasmic antibodies.
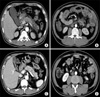
An abdominal computed tomography (CT) scan showed peripancreatic infiltration with fluid collection and multifocal bowel wall thickening with mesenteric infiltration of the small bowel (Fig. 2A, B). A kidney biopsy showed focal extra-capillary proliferative glomerulonephritis (GN), with immunofluorescence (IF) microscopic examination showing glomerular (mesangial) IgA deposits (Fig. 3). Skin biopsy showed non-specific mild perivascular lymphocyte infiltration. The patient was diagnosed with HSP complicated by acute pancreatitis and GN according to typical musculoskeletal, gastrointestinal, and renal manifestation, although skin lesion was not typical. The patient was placed on bowel rest and started on intravenous methylprednisolone (60 mg/day). Serum amylase and lipase concentrations became normal on the eighth day of treatment and the patient's clinical status improved. A follow-up abdominal CT scan on the ninth day was normal (Fig. 2C, D). Three months after discharge, however, the patient still had active urinary sediment.
Discussion
Our patient showed classical signs of HSP, including non-thrombocytopenic purpura over his upper and lower extremities, arthritis, GN, and gastrointestinal symptoms. He was diagnosed with HSP based on the presence of IgA deposits on kidney IF microscopic examination. Concomitant with abdominal pain and vomiting, the patient had elevated serum amylase and lipase concentrations, as well as peripancreatic infiltration with fluid collection on an abdominal CT scan, establishing a diagnosis of acute pancreatitis. Other known causes of pancreatitis, such as biliary tract disease, drugs, alcohol, familial hereditary pancreatitis, hypertriglyceridemia, trauma, viral infections, and hyperparathyroidism, were inconsistent with his clinical and laboratory presentations. We therefore regarded his pancreatitis as a complication of HSP.
Acute pancreatitis is a rare complication of HSP, with only a few cases reported to date. A report in 1965 described a 20-year-old man with hemorrhagic pancreatitis occurring 3 months before another episode of abdominal pain and associated with the appearance of petechiae on his extremities, suggesting that the pancreatitis was a result of HSP (13). Pediatric HSP complicated by acute pancreatitis was reported in a 7-year-old girl in 1977 (5). Pancreatitis tends to develop during the first week of the illness, but may develop after 50 days (14) or before the rash (7-12).
Appropriate medical and surgical treatment may prevent complications of pancreatitis. These include a cessation of oral nutrition. Steroids, which are not appropriate in patients with acute pancreatitis, may be used to treat patients with pancreatic involvement of HSP after excluding other causes of pancreatitis, because HSP-associated pancreatitis is likely caused by vasculitic involvement of the pancreas (3,9-12). Steroid therapy relieves the vasculitis and should be given until clinical findings disappear. Pancreatic involvement in HSP is self-limiting and benign, with prompt resolution achieved after treatment with steroids (3,9-12). HSP pancreatitis is rarely complicated by pseudocyst and it can be spontaneously resolves after 5 weeks (10).
In summary, we have described a patient with acute pancreatitis as a complication of adult HSP. To our knowledge, this is the first such case reported in Korea. HSP is a rare and benign cause of acute pancreatitis. Elevated serum amylase and lipase concentrations can be considered as early diagnostic markers of HSP pancreatitis. Patients with HSP and abdominal pain should be evaluated for pancreatitis by measurements of serum amylase and lipase concentrations, and by abdominal CT scan, to plan specific treatment and avoid unnecessary surgery.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download