Abstract
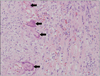
Giant cell arteritis (GCA) is a systemic vasculitis predominantly found in individuals of Northern European ancestry over 50 years of age. Typically it presents with new-onset persistent headache, claudication of jaws, and existence of an abnormal temporal artery. However, the diagnosis of GCA and the assessment of its activity remain challenging, especially in patients presenting with a variety of non-specific symptoms and laboratory tests. In those cases, 18F-fluorodeoxy-glucose positron emission tomography (18F-FDG-PET) is useful for the diagnosis of GCA. Recently, the number of foreign patients who visit domestic hospitals for medical care is increasing in Korea. Here-in, we report a Russian patient who was admitted to our hospital with fever of unknown origin (FUO). FUO study was performed to search for infection or malignancy and GCA was suspected by 18F-FDG-PET. The patient was eventually diagnosed with GCA by random temporal artery biopsy.
Figures and Tables
References
1. Chew SS, Kerr NM, Danesh-Meyer HV. Giant cell arteritis. J Clin Neurosci. 2009. 16:1263–1268.
2. Chang HK, Hur SH, Chung HR. A case of giant cell arteritis developed in polymyalgia rheumatica. J Korean Rheum Assoc. 2000. 7:72–76.
3. Seo JW, Hur J, Kim HO, Jeon DH, Baek JH, Kim JH, et al. A case of atypical giant cell arteritis presenting as Raynaud's phenomenon and diagnosed by random temporal artery biopsy. J Korean Rheum Assoc. 2010. 17:278–282.
4. Arnaud L, Haroche J, Malek Z, Archambaud F, Gambotti L, Grimon G, et al. Is (18)F-fluorodeoxyglucose positron emission tomography scanning a reliable way to assess disease activity in Takayasu arteritis? Arthritis Rheum. 2009. 60:1193–1200.
5. Breuer GS, Nesher G, Nesher R. Rate of discordant findings in bilateral temporal artery biopsy to diagnose giant cell arteritis. J Rheumatol. 2009. 36:794–796.
6. Czihal M, Tatò F, Förster S, Rademacher A, Schulze-Koops H, Hoffmann U. Fever of unknown origin as initial manifestation of large vessel giant cell arteritis: diagnosis by colour-coded sonography and 18-FDG-PET. Clin Exp Rheumatol. 2010. 28:549–552.
7. Direskeneli H, Aydin SZ, Merkel PA. Assessment of disease activity and progression in Takayasu's arteritis. Clin Exp Rheumatol. 2011. 29:1 Suppl 64. S86–S91.
8. Wang X, Hu ZP, Lu W, Tang XQ, Yang HP, Zeng LW, et al. Giant cell arteritis. Rheumatol Int. 2008. 29:1–7.
9. Cantini F, Niccoli L, Nannini C, Bertoni M, Salvarani C. Diagnosis and treatment of giant cell arteritis. Drugs Aging. 2008. 25:281–297.
10. Nesher G, Berkun Y, Mates M, Baras M, Rubinow A, Sonnenblick M. Low-dose aspirin and prevention of cranial ischemic complications in giant cell arteritis. Arthritis Rheum. 2004. 50:1332–1337.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download