Abstract
Background
The loss of bone mass is usually detected after bone marrow transplantation (BMT), particularly during the early post-transplant period. We recently reported that enhanced bone resorption following BMT was related to both the steroid dose and increase in IL-6. It was also suggested damage of the marrow microenvironment due to myeloablation and changes in bone growth factors contribute to post-BMT bone loss. Recently, the interactions of OPG and RANKL have been reported to be crucial in osteoclastogenesis and therefore in bone homeostasis. There are few data on the changes in RANKL/OPG status during the post-BMT period. This study investigated the changes in the levels of RANKL and OPG during the post-BMT period, and also assessed whether the changes in these cytokine levels actually influenced bone turnover and post-BMT bone loss.
Methods
We prospectively investigated 110 patients undergoing allogenic BMT and analyzed 36 (32.4±1.3 years, 17 men and 19 women) where DEXA was performed before and 1 year after the BMT. The serum bone turnover marker levels were measured before and 1, 2, 3, 4 and 12 wks, 6 Ms, and 1 yr after the BMT. The serum sRANKL and OPG levels were measured in all patients before and 1, 3 and 12 wks after the BMT.
Results
The mean bone losses in the lumbar spine and total proximal femur, which were calculated as the percent change from the baseline to 1 yr, were 5.2 (P<0.01) and 11.6% (P<0.01), respectively. The mean serum ICTP, a bone resorption marker, increased progressively until 3 and 6 months after the BMT, but decreased gradually thereafter, reaching the basal values after 1 year. The serum osteocalcin levels decreased progressively until 3 wks after the BMT, then increased transiently at 3 and 6 Ms, but returned to the basal level by 1 yr. The serum sRANKL and OPG levels had increased significantly by weeks 1 and 3 compared with the baseline (P<0.01), but decreased at 3 months. The sRANKL/OPG ratio increased progressively until 3 weeks, but then decreased to the basal values. During the observation period, the percent changes from the baseline in the serum RANKL levels and RANKL/OPG ratio showed positive correlations with the percent changes from the baseline serum ICTP levels. Patients with higher RANKL levels and RANKL/OPG ratio during the early post-BMT period lost more bone mass at the lumbar spine.
Conclusion
In conclusion, dynamic changes in the sRANKL and OPG levels were observed during the immediate post-BMT period, which were related to a decrease in bone formation and loss of L-spine BMD during the year following the BMT. Taken together, these results suggest that increased sRANKL levels and sRANKL/OPG ratios could be involved in a negative balance in bone metabolism following BMT.
Figures and Tables
 | Fig. 1The changes in BMD before and after BMT. The mean bone loss in the lumbar spine and proximal femur calculated as the percent change from the basline to the level at 12 months after BMT was 5.2% (P<0.05) and 11.6% (P<0.01) respectively. |
 | Fig. 2The changes of serum bone turnover markers, before and after BMT. Data are given as mean value±SEM. Immediately after BMT, ICTP was progressively increased, reaching its peak at 6 months. Thereafter it declined to the baseline at 12 months. Osteocalcin was progressively decreased, reaching its nadir at 3 weeks. Thereafter, it recovered back to the baseline level by 12 months. Serum creatinine levels were within the normal range throughout the entire observation period.
*, P<0.05; †, P<0.01 against the basal value.
|
 | Fig. 3The changes in the OPG, sRANKL levels and sRANKL/OPG ratio in the peripheral blood before and after BMT. The data are reported as a mean value±SEM. A&B, After BMT, the serum OPG and sRANKL levels was progressively increased, reaching a peak at 3 week, which declined thereafter. C, The serum sRANKL/OPG ratio was highest at post-BMT 3 weeks. †, p<0.01 against the basal value. |
Table 1
The Correlations Between the Percentage Changes from the Baseline to 1 year in the BMD at the Lumbar Spine and Proximal Femur and the Percentage Changes in OPG
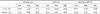
L2-4 (%): the percentage changes from the baseline to 1 yr in the BMD at the lumbar spine (lumbar vertebrae L2-L4)
femur (%): the percentage changes from the baseline to 1 yr in the BMD at the proximal femur.
sRANKL (%): the percentage changes from baseline in the sRANKL
OPG (%): the percentage changes from baseline in the OPG
sRANKL/OPG (%): the percentage changes from baseline in the sRANKL/OPG *, P<0.05
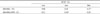
Table 2
The Correlations Between Serum OPG and Bone Turnover Markers Following BMT. Serum Levels of OPG and sRANKL were Determined Before BMT, and at 1 and 3 wk and 3 Months after BMT. Correlation Coefficients were Calculated from Matched time point. n=36. OC, Serum Osteocalcin; ICTP, Serum Collagen I Carboxy-Terminal Telopeptide

References
1. Yasuda H, Shima N, Nakagawa N, Yamaguchi K, Kinosaki M, Mochizuki S, Tomoyasu A, Yano K, Goto M, Murakami A, Tsuda E, Morinaga T, Higashio K, Udagawa N, Takahashi N, Suda T. Osteoclast differentiation factor is a ligand for osteoproteogerin/osteoclastogenesis-inhibitory factor and is identical to TRANCE/RANKL. Proc Natl Acad Sci U S A. 1998. 95:3597–3602.
2. Tsukii K, Shima N, Mochizuki S, Yamaguchi K, Kinosaki M, Yano K, Shibata O, Udagawa N, Yasuda H, suda T, Higashio K. Osteoclast differentiation factor mediates an essential signal for bone resorption induced by 1 alpha, 25-dihydroxyvitamin D3, prostaglandin E2, or parathyroid hormone in the microenvironment of bone. Biochem Biophys Res Commun. 1998. 246:337–341.
3. Takai H, Kanematsu M, Yano K, Tsuda E, Higashio K, Ikeda K, Watanabe K, Yamada Y. Transforming growth factor-beta stimulate the production of osteoprotegerin/osteoclastogenesis inhibitory factor by bone marrow stromal cells. J Biol Chem. 1998. 273:27091–27096.
4. Lories RJ, Luyten FP. Osteoprotegerin and osteoprotegerin-ligand balance: a new paradigm in bone metabolism providing new therapeutic targents. Clin Rheumatol. 2001. 20:3–9.
5. Aubin JE, Bonnelye E. Osteoprotegerin and its ligand: a new paradigm for regulation of osteoclastogenesis and bone resorption. Osteoporos Int. 2000. 11:905–913.
6. Lazner F, Gowen M, Pavasovic D, Kola I. Osteopetrosis and osteoporosis: two sides of the same coin. Hum Mol Genet. 1999. 8:1839–1846.
7. Ebeling PR, Thomas DM, Erbas B, Hopper JL, Szer J, Grigg AP. Mechanisms of bone loss following allogenic and autologous hematopoietic stem cell transplantation. J Bone Miner Res. 1999. 14:342–350.
8. Weibaecher KN. Mechanisms of osteoporosis after hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2000. 6:165–174.
9. Banfi A, Podest M, Fazzuoli L, Sertoli MR, Venturini M, Santini G, Cancedda R, Quatro R. High-dose chemotherapy shows a dose-dependent toxicity to bone marrow osteoprogenitors. Cancer. 2001. 92:2419–2428.
10. Lee WY, Cho SW, Oh ES, Oh KW, Lee JM, Yoon KH, Kang MI, Cha BY, Lee KW, Son HY, Kang SK, Kim CC. The effect of bone marrow transplantation on the osteoclastic differentiation of human bone marrow stromal cells. J Clin Endocrinol Metab. 2002. 87:329–335.
11. Lee WY, Kang MI, Oh ES, Oh KW, Han JH, Cha BY, Lee KW, Son HY, Kang SK, Kim CC. The role of cytokines in the changes in bone turnover following bone marrow transplantation. Osteoporos Int. 2002. 13:62–68.
12. Kang MI, Lee WY, Oh KW, Han JH, Song KH, Cha BY, Lee KW, Son HY, Kang SK, Kim CC. The short-term changes of bone mineral metabolism after bone marrow transplantation. Bone. 1999. 26:275–279.
13. Castaneda S, Carmona L, Carvajal I, Arranz R, Diaz A, Garcia-Vadillo A. Reduction of bone mass in women after bone marrow transplantation. Calcif Tissue Int. 1997. 60:343–347.
14. Heaf J, Tvedegaard E, Kanstrup IL, Fogh-Andersen N. Bone loss after renal transplantation: role of hyperparathyroidism, acidosis, cyclosporine and systemic disease. Clin Transplant. 2000. 14:457–463.
15. Shane E, Rivas M, McMahon DJ, Staron RB, Silverberg SJ, Seibel MJ, Mancini D, Michler RE, Aaronson K, Addesso V, Lo SH. Bone loss and turnover after cardiac transplantation. J Clin Endocrinol Metab. 1997. 82:1497–1506.
16. Yano K, Tsuda E, Washida N, Kobayashi F, Goto M, Harada A, Ikeda K, Higashio K, Yamada Y. Immunological characterization of circulating osteoprotegerin/osteoclastogenesis inhibitory factor: increased serum concentrations in postmenopausal women with osteoporosis. J Bone Miner Res. 1999. 14:518–527.
17. Yasuda H, Shima N, Nakagawa N, Mochizuki SI, Yano K, Fujise N, Sato Y, Goto M, Yamaguchi K, Kuriyama M, Kanno T, Murakami A, Tsuda E, Morinaga T, Higashio K. Identity of osteoclastogenesis inhibitory factor (OCIF) and osteoprotegerin (OPG): a mechanism by which OPG/OCIF inhibits osteoclastogenesis in vitro. Endocrinology. 1998. 139:1329–1337.
18. Lacey DL, Timms E, Tan HL, Kelley MJ, Dunstan CR, Burgess T, Elliott R, Colombero A, Elliott G, Scully S, Hsu H, Sullivan J, Hawkins N, Davy E, Capparelli C, Eli A, Qian YX, Kaufman S, Sarosi I, Shalhoub V, Senaldi G, Guo J, Delaney J, Boyle WJ. Osteoprotegerin ligand is a cytokine that regulates osteoclast differentiation and activation. Cell. 1998. 93:165–176.
19. Lee SK, Lorenzo JA. Parathyroid hormone stimulates TRANCE and inhibits osteoprotegerin messenger ribonucleic acid expression in murine bone marrow cultures: correlation with osteoclast-like cell formation. Endocrinology. 1999. 140:3552–3561.
20. Hofbauer LC, Khosla S, Dunstan CR, Lacey DL, Boyle WJ, Riggs BL. The roles of osteoprotegerin and osteoprotegerin ligand in the paracrine regulation of bone resorption. J Bone Miner Res. 2000. 15:2–12.
21. Suda T, Takahashi N, Udagawa N, Jimi E, Gillespie MT, Martin TJ. Modulation of osteoclast differentiation and function by the new members of the tumor necrosis factor receptor and ligand families. Endocrine Rev. 1999. 20:345–357.
22. Mizuno A, Amizuka N, Irie K, Murakami A, Fujise N, Kanno T, Sato Y, Nakagawa N, Yasuda H, Mochizuki S, Gomibuchi T, Yano K, Shima N, Washida N, Tsuda E, Morinaga T, Higashio K, Ozawa H. Severe osteoporosis in mice lacking osteoclastogenesis inhibitory factor/osteoprotegerin. Biochem Biophys Res Commun. 1998. 247:610–615.
23. Bucay N, Sarosi I, Dunstan CR, Morony S, Tarpley J, Capparelli C, Scully S, Tan HL, Xu W, Lacey DL, Boyle WJ, Simonet WS. osteoprotegerin-deficient mice develop early onset osteoporosis and arterial calcification. Genes Dev. 1998. 12:1260–1268.
24. Simonet WS, Lacey DL, Dunstan CR, Kelley M, Chang MS, Luthy R, Nguyen HQ, Wooden S, Bennett L, Boone T, Shimamoto G, DeRose M, Elliott R, Colombero A, Tan HL, Trail G, Sullivan J, Davy E, Bucay N, Renshaw-Gegg L, Hughes TM, Hill D, Pattison W, Campbell P, Boyle WJ, et al. Osteoprotegerin: a novel secreted protein involved in the regulation of bone density. Cell. 1997. 89:309–319.
25. Khosla S, Arrighi HM, Melton LJ 3rd, Atkinson EJ, O'Fallon WM, Dunstan C, Riggs BL. Correlates of osteoprotegerin levels in women and men. Osteoporos Int. 2002. 13:394–399.
26. Khosla S, Atkinson EJ, Dunstan CR, O'Fallon WM. Effect of estrogen versus testosterone on circulating osteoprotegerin and other cytokine levels in normal elderly men. J Clin Endocrinol Metab. 2002. 87:1550–1554.
27. Fahrleitner A, Prenner G, Leb G, Tscheliessnigg KH, Piswanger-Solkner C, Obermayer-Pietsch B, Portugaller HR, Berghold A, Dobnig H. Serum osteoprotegerin is a major determinant of bone density development and prevalent vertebral fracture status following cardiac transplantation. Bone. 2003. 32:96–106.
28. Sato T, Tominaga Y, Iwasaki Y, Kazama JJ, Shigematsu T, Inagaki H, Watanabe I, Katayama A, Haba T, Uchida K, Fukagawa M. Osteoprotegerin levels before and after renal transplantation. Am J Kidney Dis. 2001. 38:4 Suppl. 1. S175–S177.
29. Vidal NO, Brandstrom H, Jonsson KB, Ohlsson C. Osteoprotegerin mRNA is expressed in primary human osteoblast-like cells: down-regulation by glucocorticoids. J Endocrinol. 1998. 159:191–195.
30. Hofbauer LC, Riggs BL, Dunstan CR, OBrien T, Khosla S. Cyclosporine A and glucocorticoids inhibit osteoprotegerin production in human osteoblastic and coronary artery smooth muscle cells: potential mechanism of post-transplant osteoporosis and vascular disease. J Bone Miner Res. 1999. 14:Supple. 1. S176.
31. Hofbauer LC, Gori F, Riggs BL, Lacey DL, Dunstan CR, Spelsberg TC, Khosla S. Stimulation of osteoprotegerin ligand and inhibition of osteoprotegerin production by glucocorticoids in human osteoblastic lineage cells: potential paracrine mechanisms of glucocorticoid-induced osteoporosis. Endocrinology. 1999. 140:4382–4389.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download