Abstract
Background
Pollen allergy may be frequently associated with fruit-vegetables: the so-called pollen food syndrome. Pru p 3 is the most relevant peach allergen. Previously, it has been reported that serum specific IgE level to Pru p 3 depends on age in a limited geographic area.
Objective
This study aimed to to test the hypothesis about the differences of Pru p 3 sensitization across Italy, mainly concerning the impact of age.
Methods
The current study was retrospective and multicentre, involving 2 labs in Northern Italy (709 subjects), 1 in Genoa (1,040 subjects), and 1 in Southern Italy (2,188 subjects). All of them referred to labs for IgE testing because of suspected food allergy. Serum IgE to Pru p 3 was assessed in all subjects.
Lipid transfer protein (LTP) is commonly considered a panallergen as it is shared by several foods [1]. LTP is the most frequent cause of both primary food allergy and food-dependent anaphylaxis in Italy [2]. It is well known that peach may be considered the primary sensitizer to LTP in the Mediterranean area. As this protein has a cross-reactive capability, LTP-allergic patients frequently present allergy to some plant-derived foods, including Rosaceae fruits, nuts (such as hazelnut, walnut, peanut, pine nut: noteworthy these nuts belong to different botanic species), rice, maize, and vegetables, mainly tomato and lettuce [3]. In this regard, it has been reported that high levels of serum allergen-specific to the peach LTP, i.e., Pru p 3, were associated with increased probability to have systemic allergy to peach [4]. A further study partially confirmed these outcomes [5]. In fact, even though the occurrence of food allergy to foods different from Rosaceae fruits was associated with the highest serum allergen-specific IgE levels, the predictive value was rather limited.
Pollen food syndrome (PFS) is defined by symptom occurrence after eating fruits or vegetables in pollenosic patients. Usually, symptoms are confined to oral cavity: the so-called oral allergy syndrome (OAS). OAS prevalence may depend on several factors, including age, type of allergy, and residence area. Murad et al. [6] recently described the case of a child who developed 2 separate episodes of anaphylaxis after consuming apple seed and grape, with evidence that nonspecific LTPs may have been responsible for these reactions.
As this matter is particular intriguing, we would like to test the hypothesis about the differences of Pru p 3 sensitization across Italy, mainly concerning the impact of age.
The current study was retrospective and multicentre, involving 2 labs in Northern Italy (709 subjects), such as a continental area, 1 in Genoa, a Bet v 1-predominant area (1,040 subjects), and 1 in Southern Italy (2,188 subjects) typically Mediterranean area. The aim was to evaluate the impact of age on both the frequency of sensitization and the serum IgE levels to Pru p 3 in a large population.
Globally, 3,937 subjects (1,244 males; mean age, 38.2 years) were evaluated. All of them referred to labs for IgE testing because of suspected food allergy. Inclusion criterion was the measurement of serum IgE specific to Pru p 3.
The study conformed to the local ethic criteria concerning the management of clinical data and written informed consent was obtained from each subject according to the Helsinki declaration.
Serum levels of specific IgE for Bet v 1 were detected by the IFMA procedure (ImmunoCAP Thermo Fisher Scientific, Uppsala, Sweden) in peripheral blood samples from patients. Serum was collected into gel-separator tubes, centrifuged and stored at −20℃ until analysis.
Measurement of circulating specific IgE antibodies was performed according to manufacturer's instructions [7]. Specific IgE levels were expressed in kUA/L according to the traceable calibration to the 2nd Implementation Research Platform-World Health Organization for Human IgE and 0.35 kUA/L has been considered as a cutoff [8].
Patients were arbitrarily subdivided in 9 age classes: 0–5.9, 6–12.9, 13–17.9, 18–20.9, 21–30.9, 31–40.9, 41–50.9, 51–60.9, and >61 years.
Statistical analysis was performed using the statistical software package Medcalc 9 (MedCalc Software bvba, Ostend, Belgium). Medians and interquartile ranges were calculated; analysis of variance was performed.
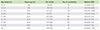
Table 1 reports the distribution of serum IgE to Pru p 3 positivities and levels according to age classes. Globally, 659 subjects were sensitized to Pru p 3, such as 16.7% of the recruited population.
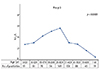
Fig. 1 shows the impact of age on percentages of Pru p 3-sensitized patients stratified for age classes. There were significant differences among the age-subgroups (p < 0.0001). In particular, sensitization percentages significantly diminished from childhood to aging.
Fig. 2 shows the impact of age on IgE serum levels on the basis of age classes. There were significant differences among the age-subgroups (p < 0.0001). Serum IgE levels progressively increased from childhood to young adulthood (peak in the 21- to 30.9-year subgroup) and then decreased until aging.
Actually, there were no significant different outcomes among centres.
This study was stimulated by the challenge offered by the intriguing relevance of PFS. PFS is the new denomination of an old clinical feature formerly known as OAS [9]. The first report was described by Tuft and Blumstein in 1942 [10]. The main characteristic is the association between pollen allergy and food allergy. Recently, the molecular allergen diagnostics allowed to understand the pathogenic association between respiratory and digestive symptoms. Interestingly, up to 60% of food allergies in older children, adolescents, and adults are linked with respiratory allergy. So, the term of PFS has been coined [1112]. Usually, the primary sensitization is pollen-related and cross-reactions with food allergens, fruits or vegetables, successively occurs. The typical example is offered by Bet v 1 (the main birch allergen) that is a sensitizer for allergy to apple. Cross-reaction is based on binding between IgE and homologous allergen structures. In other words, pollens and fruits/vegetables share common linear proteic sequences. Several studies were very recently conducted aiming to demonstrate the correlations between pollen and food molecules [1314]. In this regard, LTP family has a relevant role in the Mediterranean area and in bordering ones; so, the term LTP syndrome has been proposed [1516]. The main sensitizer of LTP syndrome is the peach.
Peach is the fruit of a small deciduous tree growing to 10 m tall, belonging to the subfamily Prunoideae of the family Rosaceae. It is classified with the Almond in the subgenus Amygdalus within the genus Prunus, distinguished from the other subgenera by the corrugated seed shell. Peach is a well documented and common cause of allergy in both children and adults, resulting in mild reactions, such as oral allergy, and systemic ones, such as urticaria, asthma, and anaphylactic shock following the ingestion of fresh or processed fruit. This is particularly relevant in the Mediterranean basin, where Peach is considered as a major allergen [17181920]. Some peach allergens of major importance have been identified, including LTP, profilin, and many larger proteins.
At present, 3 main peach allergen molecules have been detected and are available for molecualr diagnostics: Pru p 1, Pru p 3, and Pru p 4.
Pru p 1 is a 17-kDa peach protein belonging to the PR-10 protein family. The major birch pollen allergen Bet v 1 is the most prominent member of this family, with which Pru p 1 shares 59% amino acid sequence identity [21]. Pru p 1 is heat labile and most subjects suffering from birch-pollen-induced peach allergy may tolerate cooked peaches [22]. Pru p 1 cross-reacts extensively with Bet v 1 homologous from Prunus pecies (e.g., cherry, apricot, plum) and other Roseaceae fruits such as apple and also, although to a lower degree, with PR-10 proteins from foods like carrot, celery, soy, and peanut. Sensitization to Pru p 1 is not necessarily manifested as clinical reactions to peach but is a good marker for the birch-fruit syndrome. Ingestion of peach and other related foods may elicit oral symptoms but also, in rare cases, more severe systemic reactions [2324].
Pru p 3 is a nonspecific LTP. LTPs are panallergens characterized by ubiquitous distribution in tissues of many plant species, resulting in variable degrees of cross-reactivity, and in particularly relevant cross-reactivity in fruits and vegetables [25]. LTPs are small molecules of approximately 9–10 kDa that demonstrate great stability and are very resistant to pepsin and heat treatment [26]. LTPs are highly conserved and widely distributed throughout the plant kingdom. They have been identified as allergens in the Rosaceae subfamilies of the Prunoideae (peach, apricot, plum) and of the Pomoideae (apple). They belong to a family of structurally highly conserved proteins that are also present in non-Rosaceae vegetable foods. They have been linked to severe and systemic symptoms and induce sensitisation by the oral route in fruit-allergic patients who do not have associated pollen allergy. This is probably due to extreme pepsin stability; the allergens probably reach the intestinal tract in an almost unmodified form.
LTP is found in Peach peel in amounts approximately 7 times greater than in pulp [27]. It may be absent from chemically peeled fruit, and levels of LTP vary in different cultivars and at different stages of the ripening process, showing a progressive increment during ripening [28]. Pru p 3 may be involved in allergenic relationships with other fruits from the family Rosaceae, particularly apricot, cherry, and plum. A high level of cross-reactivity occurs among fruits and vegetables containing LTPs, which include sweet chestnut, cabbage, walnut, lettuce, and hazelnut [2930]. Grape and wine may contain LTP homologous to and cross-reactive with peach LTP [31]. LTP cross-reactivity is often accompanied by clinical food allergy, frequently including systemic reactions [32]. Finally, peach has been identified the primer sensitizer to Pru p 3 [33].
Pru p 4 is a peach profilin and an actinbinding protein, it is a member of the profilin plant family. Profilins are panallergens recognised in about 20% of patients with birch allergy and plant foods allergy [34]. Profilins are heat- and digestion-labile and are therefore more often associated with less severe allergic reactions and OAS. Plant profilins may cause several allergies to pollens [35]. Pru p 4 has a sequence identity very similar to plant pollens, mainly concerning Bet v 2: the birch profilin.
Previously, it has been reported by a study conducted in Genoa that Pru p 3 sensitization is closely dependent on age [36]. So, the current study was designed to confirm that experience in a larger set of population across Italy.
The current showed some relevant outcomes: (1) Sixteen point seven percent (16.7%) of recruited subjects were sensitized to Pru p 3. (2) The percentage of sensitization significantly decreased over time. (3) Serum IgE levels trend to increase from infancy to young adulthood and then trend to reduce until aging. Thus, age may impact the production of IgE to Pru p 3. Of note, there was no difference among centers; this point is very relevant as underlines a scarce influence of climate on LTP sensitization and production across Italy. Therefore, the age plays a relevant impact on the sensitization pattern as well as on the serum levels. Unfortunately, this experience had the limitation of clinical data lacking and the sizes of the single age classes are inconsistent. However, a relative correlation between serum IgE level and allergy diagnosis as well as symptom severity was previously reported [45]. These findings underline the relevance of considering age when IgE are interpreted and the practical importance of adequately paying attention to this issue in real life, such as in allergy clinic.
In conclusion, our experience demonstrates that Pru p 3 sensitization and production are closely age-dependent phenomena.
Figures and Tables
ACKNOWLEDGEMENTS
We wish to thank Sabrina Nigrisoli for helpful assistance in the statistical analysis.
References
1. Pastorello EA, Robino AM. Clinical role of lipid transfer proteins in food allergy. Mol Nutr Food Res. 2004; 48:356–362.

2. Asero R, Antonicelli L, Arena A, Bommarito L, Caruso B, Crivellaro M, De Carli M, Della Torre E, Della Torre F, Heffler E, Lodi Rizzini F, Longo R, Manzotti G, Marcotulli M, Melchiorre A, Minale P, Morandi P, Moreni B, Moschella A, Murzilli F, Nebiolo F, Poppa M, Randazzo S, Rossi G, Senna GE. EpidemAAITO: features of food allergy in Italian adults attending allergy clinics: a multi-centre study. Clin Exp Allergy. 2009; 39:547–555.

3. Asero R, Mistrello G, Roncarolo D, Amato S, Caldironi G, Barocci F, van Ree R. Immunological cross-reactivity between lipid transfer proteins from botanically unrelated plant-derived foods: a clinical study. Allergy. 2002; 57:900–906.

4. Rossi RE, Monasterolo G, Canonica GW, Passalacqua G. Systemic reactions to peach are associated with high levels of specific IgE to Pru p 3. Allergy. 2009; 64:1795–1796.

5. Asero R, Arena A, Cecchi L, Conte ME, Crivellaro M, Emiliani F, Lodi Rizzini F, Longo R, Minale P, Murzilli F, Musarra A, Nebiolo F, Quercia O, Ridolo E, Savi E, Senna GE, Villalta D. Are IgE levels to foods other than rosaceae predictive of allergy in lipid transfer protein-hypersensitive patients? Int Arch Allergy Immunol. 2011; 155:149–154.

6. Murad A, Katelaris CH, Baumgart K. A case study of apple seed and grape allergy with sensitisation to nonspecific lipid transfer protein. Asia Pac Allergy. 2016; 6:129–132.

7. Leimgruber A, Mosimann B, Claeys M, Seppey M, Jaccard Y, Aubert V, Peitrequin R, Nisoli MP, Pécoud A. Clinical evaluation of a new in-vitro assay for specific IgE, the immuno CAP system. Clin Exp Allergy. 1991; 21:127–131.

8. Seagroatt V, Anderson SG. The second international reference preparation for human serum immunoglobulin E and the first British standard for human serum immunoglobulin E. J Biol Stand. 1981; 9:431–437.

9. Webber CM, England RW. Oral allergy syndrome: a clinical, diagnostic, and therapeutic challenge. Ann Allergy Asthma Immunol. 2010; 104:101–108.

10. Tuft L, Blumstein GI. Studies in food allergy: II. Sensitization to fresh fruits: clinical and experimental observations. J Allergy. 1942; 13:574–582.
11. Price A, Ramachandran S, Smith GP, Stevenson ML, Pomeranz MK, Cohen DE. Oral allergy syndrome (pollen-food allergy syndrome). Dermatitis. 2015; 26:78–88.

12. Werfel T, Asero R, Ballmer-Weber BK, Beyer K, Enrique E, Knulst AC, Mari A, Muraro A, Ollert M, Poulsen LK, Vieths S, Worm M, Hoffmann-Sommergruber K. Position paper of the EAACI: food allergy due to immunological cross-reactions with common inhalant allergens. Allergy. 2015; 70:1079–1090.

13. Ludman S, Jafari-Mamaghani M, Ebling R, Fox AT, Lack G, Du Toit G. Pollen food syndrome amongst children with seasonal allergic rhinitis attending allergy clinic. Pediatr Allergy Immunol. 2016; 27:134–140.

14. Mastrorilli C, Tripodi S, Caffarelli C, Perna S, Di Rienzo-Businco A, Sfika I, Asero R, Dondi A, Bianchi A, Povesi Dascola C, Ricci G, Cipriani F, Maiello N, Miraglia Del Giudice M, Frediani T, Frediani S, Macrì F, Pistoletti C, Dello Iacono I, Patria MF, Varin E, Peroni D, Comberiati P, Chini L, Moschese V, Lucarelli S, Bernardini R, Pingitore G, Pelosi U, Olcese R, Moretti M, Cirisano A, Faggian D, Travaglini A, Plebani M, Verga MC, Calvani M, Giordani P, Matricardi PM. Italian Pediatric Allergy Network (I-PAN). Endotypes of pollen-food syndrome in children with seasonal allergic rhinoconjunctivitis: a molecular classification. Allergy. 2016; 71:1181–1191.

15. Pascal M, Muñoz-Cano R, Reina Z, Palacín A, Vilella R, Picado C, Juan M, Sánchez-López J, Rueda M, Salcedo G, Valero A, Yagüe J, Bartra J. Lipid transfer protein syndrome: clinical pattern, cofactor effect and profile of molecular sensitization to plant-foods and pollens. Clin Exp Allergy. 2012; 42:1529–1539.

16. Azofra J, Berroa F, Gastaminza G, Saiz N, Gamboa PM, Vela C, García BE, Lizarza S, Echenagusia MA, Joral A, Aranzabal MA, Quiñones MD, Jauregui I, Madera JF, Navarro JA, Lizaso MT, Bernad A, Goikoetxea MJ. Lipid transfer protein syndrome in a non-Mediterranean area. Int Arch Allergy Immunol. 2016; 169:181–188.

17. Fernández-Rivas M, González-Mancebo E, Rodríguez-Pérez R, Benito C, Sánchez-Monge R, Salcedo G, Alonso MD, Rosado A, Tejedor MA, Vila C, Casas ML. Clinically relevant peach allergy is related to peach lipid transfer protein, Pru p 3, in the Spanish population. J Allergy Clin Immunol. 2003; 112:789–795.
18. Rodríguez-Perez R, Fernández-Rivas M, González-Mancebo E, Sánchez-Monge R, Díaz-Perales A, Salcedo G. Peach profilin: cloning, heterologous expression and cross-reactivity with Bet v 2. Allergy. 2003; 58:635–640.

19. Rodriguez J, Crespo JF, Lopez-Rubio A, De La Cruz-Bertolo J, Ferrando-Vivas P, Vives R, Daroca P. Clinical cross-reactivity among foods of the Rosaceae family. J Allergy Clin Immunol. 2000; 106(1 Pt 1):183–189.

20. García-Sellés FJ, Díaz-Perales A, Sánchez-Monge R, Alcántara M, Lombardero M, Barber D, Salcedo G, Fernández-Rivas M. Patterns of reactivity to lipid transfer proteins of plant foods and Artemisia pollen: an in vivo study. Int Arch Allergy Immunol. 2002; 128:115–122.
21. Marknell Dewitt Å, Andersson K, Lidholm J. Cloning and sequence of the major peach allergen Pru p 1. Sequence accession No. ABB78006, direct submission. https://www.ncbi.nlm.nih.gov/protein/82492265/.
22. Ahrazem O, Jimeno L, López-Torrejón G, Herrero M, Espada JL, Sánchez-Monge R, Duffort O, Barber D, Salcedo G. Assessing allergen levels in peach and nectarine cultivars. Ann Allergy Asthma Immunol. 2007; 99:42–47.

23. Fernández-Rivas M, Bolhaar S, González-Mancebo E, Asero R, van Leeuwen A, Bohle B, Ma Y, Ebner C, Rigby N, Sancho AI, Miles S, Zuidmeer L, Knulst A, Breiteneder H, Mills C, Hoffmann-Sommergruber K, van Ree R. Apple allergy across Europe: how allergen sensitization profiles determine the clinical expression of allergies to plant foods. J Allergy Clin Immunol. 2006; 118:481–488.

24. Asero R. Plant food allergies: a suggested approach to allergen-resolved diagnosis in the clinical practice by identifying easily available sensitization markers. Int Arch Allergy Immunol. 2005; 138:1–11.

25. Sánchez-Monge R, Lombardero M, García-Sellés FJ, Barber D, Salcedo G. Lipid-transfer proteins are relevant allergens in fruit allergy. J Allergy Clin Immunol. 1999; 103(3 Pt 1):514–519.

26. Asero R, Amato S, Alfieri B, Folloni S, Mistrello G. Rice: another potential cause of food allergy in patients sensitized to lipid transfer protein. Int Arch Allergy Immunol. 2007; 143:69–74.

27. Carnés J, Fernández-Caldas E, Gallego MT, Ferrer A, Cuesta-Herranz J. Pru p 3 (LTP) content in peach extracts. Allergy. 2002; 57:1071–1075.

28. Brenna OV, Pastorello EA, Farioli L, Pravettoni V, Pompei C. Presence of allergenic proteins in different peach (Prunus persica) cultivars and dependence of their content on fruit ripening. J Agric Food Chem. 2004; 52:7997–8000.

29. Sánchez-Monge R, Blanco C, López-Torrejón G, Cumplido J, Recas M, Figueroa J, Carrillo T, Salcedo G. Differential allergen sensitization patterns in chestnut allergy with or without associated latex-fruit syndrome. J Allergy Clin Immunol. 2006; 118:705–710.
30. Palacín A, Cumplido J, Figueroa J, Ahrazem O, Sánchez-Monge R, Carrillo T, Salcedo G, Blanco C. Cabbage lipid transfer protein Bra o 3 is a major allergen responsible for cross-reactivity between plant foods and pollens. J Allergy Clin Immunol. 2006; 117:1423–1429.
31. Pastorello EA, Farioli L, Pravettoni V, Ortolani C, Fortunato D, Giuffrida MG, Perono Garoffo L, Calamari AM, Brenna O, Conti A. Identification of grape and wine allergens as an endochitinase 4, a lipid-transfer protein, and a thaumatin. J Allergy Clin Immunol. 2003; 111:350–359.

32. Asero R, Mistrello G, Roncarolo D, de Vries SC, Gautier MF, Ciurana CL, Verbeek E, Mohammadi T, Knul-Brettlova V, Akkerdaas JH, Bulder I, Aalberse RC, van Ree R. Lipid transfer protein: a pan-allergen in plant-derived foods that is highly resistant to pepsin digestion. Int Arch Allergy Immunol. 2000; 122:20–32.

33. Asero R, Mistrello G, Amato S, Roncarolo D, Martinelli A, Zaccarini M. Peach fuzz contains large amounts of lipid transfer protein: is this the cause of the high prevalence of sensitization to LTP in Mediterranean countries? Eur Ann Allergy Clin Immunol. 2006; 38:118–121.
34. Willerroider M, Fuchs H, Ballmer-Weber BK, Focke M, Susani M, Thalhamer J, Ferreira F, Wüthrich B, Scheiner O, Breiteneder H, Hoffmann-Sommergruber K. Cloning and molecular and immunological characterisation of two new food allergens, Cap a 2 and Lyc e 1, profilins from bell pepper (Capsicum annuum) and Tomato (Lycopersicon esculentum). Int Arch Allergy Immunol. 2003; 131:245–255.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download