Abstract
Background
In view of the increasing prevalence of food allergies, there has been an associated increase in frequency of situations requiring an emergency response for anaphylaxis at the home, childcare facilities and educational institutions.
Objective
To clarify the situation of adrenaline auto-injector administration in nursery/kindergarten/school, we carried out a questionnaire survey on pediatric physicians in Western Japan.
Methods
In 2015, self-reported questionnaires were mailed to 421 physicians who are members of the West Japan Research Society Pediatric Clinical Allergy and Shikoku Research Society Pediatric Clinical Allergy.
Results
The response rate was 44% (185 physicians) where 160 physicians had a prescription registration for the adrenaline auto-injector. In the past year, 1,330 patients were prescribed the adrenaline auto-injector where 83 patients (6% of the prescribed patients) actually administered the adrenaline auto-injector, of which 14 patients (17% of the administered patients) self-administered the adrenaline auto-injector. “Guardians” at the nursery/kindergarten and elementary school were found to have administered the adrenaline auto-injector the most. Among 117 adrenaline auto-injector prescription-registered physicians, 79% had experienced nonadministration of adrenaline auto-injector at nursery/kindergarten/school when anaphylaxis has occurred. The most frequent reason cited for not administering the adrenaline auto-injector was “hesitation about the timing of administration.”
Conclusion
If the adrenaline auto-injector was administered after the guardian arrived at the nursery/kindergarten/school, it may lead to delayed treatment of anaphylaxis in which symptoms develop in minutes. Education and cooperation among physicians and nursery/kindergarten/school staff will reduce the number of children suffering unfortunate outcomes due to anaphylaxis.
In association with the increase in number of patients with food allergies and anaphylaxis [1], the frequency of occasions requiring emergency care at the home, nursery, kindergarten, and school has also increased [2]. In order to minimize accidental exposure to foods to which a child could be allergic, many schools in the United States have a “no sharing” policy for food [3]. There has been an increasing need to provide allergy countermeasures during school lunches [45].
In Japan, after a fatal case of food allergy-induced anaphylaxis occurred during a school lunch in 2012, “Basic Rules Regarding Measures Against Allergic Diseases” were established and the Ministry of Education, Culture, Sports, Science and Technology announced “Guidelines for Allergic Diseases in Schools” in 2008 and “Correspondence Guidelines for Food Allergies during School Lunches” in 2015, recommending food allergy countermeasures and the use of the adrenaline auto-injector (AAI) should anaphylaxis occur. “Japanese Guidelines for Food Allergy” were also published by the Japanese Society of Pediatric Allergy and Clinical Immunology [6]. However, it is unclear whether the AAI is appropriately administrated in patients with anaphylaxis at nursery/kindergarten/school.
In this study, to clarify the actual situation of AAI administration in nursery/kindergarten/school, we carried out a field survey on AAI with members of the West Japan Research Society Pediatric Clinical Allergy and Shikoku Research Society Pediatric Clinical Allergy. All members were clinicians who have been engaged in the Department of Pediatrics and/or Pediatric Allergy in Western Japan.
During the period from January to March 2015, self-reported questionnaires (Table 1) were mailed to 421 physicians who were members of the West Japan Research Society Pediatric Clinical Allergy and the Shikoku Research Society Pediatric Clinical Allergy. The physicians were requested to send one answer sheet per facility by Fax/E-mail. We obtained informed consent from all physicians for publication of this study.
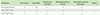
As shown in Fig. 1, responses (rate) were received from 185 physicians (44% of the number sent). One hundred sixty of the physicians were “registered as an insurance AAI prescribing physician,” while 25 were “nonregistered physicians.” The responses from registered AAI prescribing physicians are analyzed below.
Number of patients who were prescribed AAI, and patients who administrated the AAI.
One hundred sixty AAI prescription-registered physicians, the total number of patients with food allergy was 10,574. One thousand three hundred thirty patients were prescribed AAI during the past one year by 117 AAI prescription-registered physicians. Of the patients who were prescribed AAI, the AAI was actually administered in 83 patients (6% of the prescribed patients). Of the patients who administered AAI, the AAI was self-administered in 14 patients (17% of the administered patients).
Forty-five (45) physicians had patients who administered the AAI. Among these physicians, the most common location for AAI administration was “at home” (21 physicians), followed by “at nurseries/kindergartens/schools” (12 physicians), and “others” (5 physicians).
As shown in Table 2, the person who administered the AAI at nursery/kindergarten/school was answered by the physicians as follows, in descending order: “guardians” (10 physicians) and “emergency medical technician” (1 physician) at nursery/kindergarten; “guardians” (12 physicians), “nursing teachers/nurses” (3 physicians), “themselves” (1 physician), “homeroom teachers” (1 physician), and “others” (2 physicians) at elementary school; and “themselves” (5 physicians), “nursing teachers/nurses” (3 physicians), “guardians” (2 physicians), “principals/assistant principals” (1 physician), and “others” (1 physician) at junior-high school.
Among 117 AAI prescription-registered physicians, 92 (79%) had experienced nonadministration of AAI at nursery/kindergarten/school when anaphylaxis has occurred. As shown in Table 3, the most frequently cited reason for nonadministration of AAI at nursery/kindergarten/school was “hesitation about the timing of administration” (31 physicians); and others including “forgot to carry AAI” (5 physicians); “fears regarding the procedure” (4 physicians); “fear of adverse reactions” (2 physicians); “improved with other medicines” (2 physicians); “direction from emergency staff to wait until they contacted the personal doctor” (1 physician); and “determined that there was no need for administration” (1 physician).
As shown in Table 4, the criteria for the physicians to prescribe AAI were, in descending order, a “history of anaphylaxis” (160 physicians); “living distant from emergency department” (77 physicians); “the guardians' request” (72 physicians); and “possibility of repeated accidental ingestion” (70 physicians).
Cooperation between physicians and the nurser y/kindergarten/school was put into practice, in descending order, by “communication in writing” (132 physicians); “direct meeting” (82 physicians); “instruct at training workshops” (75 physicians); “provide certification” (76 physicians).
According to the Ministry of Education, Culture, Sports, Science and Technology in Japan, the proportion of patients with food allergies in Japan is 4.5% in elementary school children, 4.8% in junior-high school children, and 4.0% in high school children, with those having experienced anaphylaxis being 0.6%, 0.4%, and 0.3%, respectively. In Japan, the number of deaths due to food anaphylaxis has increased from 15 patients during the period from 1996 through 2001 to 27 patients from 2006 through 2011, and with the occurrence of a recent fatal case during a school lunch, there is clearly an urgent need for countermeasures. The use of AAI is central to these countermeasures and the Japan Society of Pediatric Allergy and Clinical Immunology is promoting clarification of the symptoms and timing of administration [67].
In the present investigation, the actual rate of AAI administration was 6% of the prescribed patients and the rate of self-administered AAI was 17% of the administered patients. Surprisingly, most AAI administrators at nurseries/kindergartens, and elementary schools were the guardians. If AAI was administered after the guardians arrived at nurseries/kindergartens/elementary schools, it sometimes led to delayed treatment for anaphylaxis in which symptoms develop in minutes.
Moreover, 79% physicians had experienced nonadministration of AAI at nursery/kindergarten/school when anaphylaxis has occurred. The most frequently cited reason for not administering the AAI at nursery/kindergarten/school was “hesitation about the timing of administration”. Fleming et al. [8] reported that administration at an early stage can reduce the risk of hospitalization and administration at the proper timing is required. Delayed administration of AAI has been reported in yet another large series of anaphylaxis-related fatalities [4]. Many guidelines recommend that all staff engaged in a nursery/kindergarten/school receive AAI training [49].
These problems of AAI at the nursery/kindergarten/school is not only an issue in Japan. Caffarelli et al. [10] reported that only 2.8% of school children with food allergy were prescribed AAI, and Fleischer et al. [11] reported that AAI was administered to only 30% of patients even when anaphylaxis had occurred. Moreover, Ben-Shoshan et al. [12] described that among 4- to 19-year-old patients prescribed with AAI, 48% do not bring the AAI to school. In the current study, unfortunately, the method of cooperation between physicians and nurseries/kindergartens/schools is limited to “communication in writing.”
There are some limitations associated with the present report. Firstly, because this questionnaire was retrospectively completed by physicians, there could be a recall bias. Secondly, the response rate was low at 44%. Thirdly, the pediatric population of these areas is approximately 3,000,000 patients with food allergies estimated at 120,000. Therefore, 10,574 patients with food allergies whom the physicians treat comprise only approximately 10% of these areas. Fourthly, we requested physicians to send back one answer sheet per facility. However, physicians who completed the questionnaire were not able to confirm if the response was representative of the entire facility. Additionally, some question results only reflected the number of physicians who answered instead of the number of patients, etc.
However, the actual situation of AAI prescription and administration has become apparent, leading to the identification of challenges involved. Education and cooperation among physicians and nursery/kindergarten/school staffs will reduce the number of children suffering unfortunate outcomes due to anaphylaxis.
Figures and Tables
 | Fig. 1Response rates and background of the physicians. Responses (rate) were received from 185 physicians (44% of the number sent). One hundred sixty of the physicians were “registered as an insurance adrenaline auto-injector (AAI) prescribing physician,” while 25 were “nonregistered physicians.” The responses from registered AAI prescribing physicians are analyzed below. |
References
1. Grabenhenrich LB, Dölle S, Moneret-Vautrin A, Köhli A, Lange L, Spindler T, Ruëff F, Nemat K, Maris I, Roumpedaki E, Scherer K, Ott H, Reese T, Mustakov T, Lang R, Fernandez-Rivas M, Kowalski ML, Bilò MB, Hourihane JO, Papadopoulos NG, Beyer K, Muraro A, Worm M. Anaphylaxis in children and adolescents: The European Anaphylaxis Registry. J Allergy Clin Immunol. 2016; 137:1128–1137.e1.

2. Ward CE, Greenhawt MJ. Treatment of allergic reactions and quality of life among caregivers of food-allergic children. Ann Allergy Asthma Immunol. 2015; 114:312–318.e2.

3. Rhim GS, McMorris MS. School readiness for children with food allergies. Ann Allergy Asthma Immunol. 2001; 86:172–176.

4. Simons FE, Ebisawa M, Sanchez-Borges M, Thong BY, Worm M, Tanno LK, Lockey RF, El-Gamal YM, Brown SG, Park HS, Sheikh A. 2015 update of the evidence base: World Allergy Organization anaphylaxis guidelines. World Allergy Organ J. 2015; 8:32.

5. Pistiner M, Devore CD, Schoessler S. School Food Allergy and Anaphylaxis Management for the Pediatrician--Extending the Medical Home with Critical Collaborations. Pediatr Clin North Am. 2015; 62:1425–1439.

6. Urisu A, Ebisawa M, Ito K, Aihara Y, Ito S, Mayumi M, Kohno Y, Kondo N. Committee for Japanese Pediatric Guideline for Food Allergy. Japanese Society of Pediatric Allergy and Clinical Immunology. Japanese Society of Allergology. Japanese guideline for food allergy 2014. Allergol Int. 2014; 63:399–419.

7. Inoue N, Yamamoto A. Clinical evaluation of pediatric anaphylaxis and the necessity for multiple doses of epinephrine. Asia Pac Allergy. 2013; 3:106–114.

8. Fleming JT, Clark S, Camargo CA Jr, Rudders SA. Early treatment of food-induced anaphylaxis with epinephrine is associated with a lower risk of hospitalization. J Allergy Clin Immunol Pract. 2015; 3:57–62.

9. Vale S, Smith J, Said M, Mullins RJ, Loh R. ASCIA guidelines for prevention of anaphylaxis in schools, pre-schools and childcare: 2015 update. J Paediatr Child Health. 2015; 51:949–954.

10. Caffarelli C, Coscia A, Ridolo E, Povesi Dascola C, Gelmett C, Raggi V, Volta E, Vanell M, Dall'Aglio PP. Parents' estimate of food allergy prevalence and management in Italian school-aged children. Pediatr Int. 2011; 53:505–510.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download