Abstract
Background
Specific IgE antibodies against the low-molecular-weight carbohydrate antigen that does not bridge IgE molecules on mast cells are not associated with clinical symptoms. Cross reactivity can be determined in allergen-specific IgE detection assays when the carbohydrate structures between pollen allergens and plant derived food allergens are similar; in such cases, false positive results for grain or legume allergens can be reported for pollen allergic patients who are not sensitized to those allergens. This phenomenon arises owing to the presence of cross-reactive carbohydrate determinants (CCDs).
Objective
This study aimed to assess the impact of CCD interference on the results for pollen allergen-specific IgE antibodies in the general adult population and to perform CCD inhibition tests evaluating the involvement of CCD on samples positive to pollen allergens.
Methods
Serum samples from 322 subjects were tested for IgE antibodies to pollens and CCD. The research subjects were given questionnaires about pollen allergic symptoms to help assess the presence of allergies. Allergen IgE antibodies for Japanese cedar, Japanese cypress, orchard grass, ragweed, MUXF, bromelain, horseradish peroxidase (HRP), and ascorbate oxidase (ASOD) were analyzed.
Results
It was observed that among individuals who tested positive to any of the pollen allergens, the positive ratio of CCD-specific IgE antibody was the highest for HRP (13.5%–50.0%). The results from the inhibition tests revealed that CCD was marginally present. Although IgE antibodies for cedar pollen did not react with CCD, IgE antibodies for Japanese cypress, orchard grass, and ragweed might be detected by the presence of CCD.
Identification of causative antigens is generally performed using methods of allergen-specific IgE antibody tests, skin allergy tests (e.g., intracutaneous and scratch tests), and allergen-induced tests. Serum specific IgE tests based on the fluorescence-enzyme immunoassay, chemiluminescent enzyme immunoassay, and enzyme immunoassay are often favorably chosen in clinical settings owing to the capability of testing different allergen-specific IgE antibodies with relatively high specificity [1]. However, there are often cases in which patients show no symptoms despite detection of allergen-specific IgE antibodies. As with sensitization just below the threshold, it has been recently suggested that one of the possible causes of these false positives may be a cross-reaction of allergen-specific IgE antibodies with cross-reactive carbohydrate determinants (CCDs) specific antigens [23].
The carbohydrate structures of glycoprotein allergens in pollen and food are partially identical to each other; it is reported that patients who are sensitized to pollen allergens may not have any symptoms when allergy is induced by oral food challenge despite the presence of specific IgE [45]. In fact, it has been reported that glycoproteins of Cry j1 and Jun a1 (Japanese cedar pollen allergens) and Cha o1 (Japanese cypress pollen allergen) share these similar structures [678]. The carbohydrate structure of CCDs was initially identified as a N-linked oligomannose-type carbohydrate chain with β1,2-xylose and α1-3 fucose branches linked to bromelain, a thiol protease present in pineapple [9]. Glycoproteins from bromelain, horseradish peroxidase (HRP), and ascorbate oxidase (ASOD) are also known to share similar specific IgE binding structures in plant CCDs against which specific IgE antibodies can be produced [310]. However, unlike allergens, these glycoproteins show less type I hypersensitivity reaction-inducing capacity and less association with the presence of clinical symptoms. This may be attributed to the monovalent structure of most CCD-glycoproteins, where cross-linkages between the CCD and the anti-CCD-specific IgE antibodies on the mast cell membrane are not formed, thus prohibiting degranulation and the release of chemical transmitters (e.g., histamine) [111213]. In patients who show no clinical symptoms despite the detection of specific IgE antibodies to allergens (e.g., pollen), these false positive results may be attributed to cross-reactivity, in which the CCD-glycoprotein specific IgE in serum may be nonspecifically bound to pollen allergens due to the absence of allergen-specific IgE antibodies.
In this study, we evaluated the potential interference of 4 common types of CCDs on the diagnosis of pollen allergies. We report our findings as well as a review of previously published reports on CCD.
To assess the impact of CCD interference, we first evaluated the presence of CCD-specific IgE antibodies in serum samples from patients with complaints of the common nasal symptoms of pollen allergy (e.g., nasal discharge, stuffiness, and sneezing). In order not to occur difference of time of taking blood samples, and to obtain and examine as many data of average adults as possible, after conducting a survey on the subjective symptoms of pollen allergy, testing was performed for pollen- and CCD-related allergen-specific IgE antibodies in a general adult population who participated in a medical examination. An inhibition test was used to evaluate in vitro cross-reactivity between CCD- and pollen-specific IgE antibodies. Additionally, we analyzed possible associations with food allergy and evaluated the test results based on the presence of asthma symptoms, smoking and drinking habits, serum cholesterol and triglyceride levels, obesity, prevalence of pollen allergy, and the detection frequency of CCD.
We evaluated 129 outpatients (male, 63; female, 66; mean age, 44.7 years; range, 11–86 years) who visited the Department of Otorhinolaryngology, Juntendo University from October 2010 through March 2011, with complaints of seasonal symptoms such as nasal discharge, stuffiness, sneezing and/or ocular itching, and gave informed consent.
We evaluated 322 employees of SHiDAX (male, 255; female, 67; mean age, 40.7 years; range, 20–67 years) who participated in a health screening during October 1–23, 2012.
Serum samples were collected from the venous blood of subjects and were preserved at −20℃. IMMULITE 2000 Systems 3 g Allergy (Siemens Healthcare GmbH, Erlangen, Germany), a chemiluminescent enzyme immunoassay, was used for measuring the specific IgE antibody titers to the following allergens: pollen of Japanese cedar, Japanese cypress, orchard grass, and ragweed; CCD allergens of MUXF, bromelain, HRP, and ASOD; and food allergens of wheat and soybean. The titer levels were defined as negative when <0.1 IUA/mL, slightly positive between 0.1–0.34 IUA/mL, and positive when ≥0.35 IUA/mL.
CCD extracts were diluted in phosphate buffer solution to prepare the inhibitor solution. Ten-fold serial dilutions (undiluted, 1/10, 1/100) of the inhibitor solution were prepared. The dilutions were individually dispensed into patient samples and into IgE negative serum used as the negative control. These mixtures with the inhibitor and sample were mixed well and incubated at room temperature for 1 hour prior to testing for pollen-specific IgE antibody titers.
The study protocol was approved by the Institutional Review Board of the Juntendo Urayasu Hospital (No. 22-41) and Kyorin University (No. 427). This study was conducted in accordance with the principles of the Declaration of Helsinki.
One hundred twenty-nine patients with complaints for the common symptoms of pollen allergy, including nasal discharge, stuffiness, and sneezing were enrolled to be tested for pollen allergen-specific IgE antibodies. In this population, specific IgE antibodies to Japanese cedar, orchard grass, and ragweed were evaluated as the common pollen allergens in Japan. The numbers of positive samples were: 79 for Japanese cedar (61.2%), 30 for orchard grass 30 (23.3%), and 11 for ragweed (8.5%) (Table 1). In addition, CCD-related antigen-specific IgE antibodies were evaluated using MUXF, bromelain, HRP, and ASOD as the known CCDs. The number of cases with detectable specific IgE to each CCD was as follows: 3 for MUXF (2.3%), 13 for HRP (10.1%), 7 for bromelain (5.4%), and 7 for ASOD (5.4%). CCD-specific IgE antibodies of all types were detected for each type of pollen. Positive detection rates for anti-CCD antibodies were relatively more prevalent in ragweed (bromelain 6, 54.5%) than orchard grass (HRP 7, 23.3%) and Japanese cedar (HRP 10, 12.7%). MUXF was less frequently detected in comparison to the other pollens tested (Table 1).
Serum samples from employees who participated in a health screening were measured to determine the prevalence of CCD-related antigen-specific IgE antibodies in a general adult population. These subjects were also tested for pollen allergen-specific IgE antibodies and were given a questionnaire about pollen allergens to investigate a possible association with pollen allergies. Additionally, these test results were evaluated based on the presence of asthma symptoms, smoking and drinking habits, serum cholesterol and neutral fat levels, obesity, prevalence of pollen allergies, and the detection frequency of CCD. In this study, reviews of previously published reports on CCD are also included.
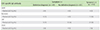
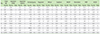
Three hundred twenty-two subjects were classified into 3 different groups: group 1, with subjective symptoms and a definitive diagnosis of pollen allergy, i.e., diagnosis by a doctor (n = 57); group 2, with subjective symptoms and without definitive diagnosis (n = 100); and group 3, without subjective symptoms (n = 165). The prevalence of pollen-specific IgE antibodies in groups 1, 2, and 3, respectively, were as follows: 82%, 79%, and 68% for Japanese cedar; 61%, 68%, and 55% for Japanese cypress; 23%, 34%, and 19% for orchard grass; and 5%, 11%, and 6% for ragweed (Table 2). The numbers of positive cases for one or more types of pollen-specific IgE antibodies was 47 of 57 in group 1, 81 of 100 in group 2, and 115 of 165 in group 3.
There was no significant difference in the presence of asthma symptoms, smoking and drinking habits, serum cholesterol and neutral fat levels, obesity, prevalence of pollen allergy, and the detection frequency of CCD (data not shown).
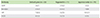
The prevalence of CCD-related allergen-specific IgE antibodies in pollen-specific IgE positive subjects was determined. The prevalence of CCD-specific IgE antibodies in group 1 (n = 47), group 2 (n = 81), and in group 3 (n = 115), respectively, was as follows: 4%, 5%, and 3% for MUXF; 11%, 5%, and 10% for bromelain; 11%, 16%, and 18% for HRP; and 6%, 5%, and 6% for ASOD (Table 3).
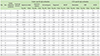
CCD inhibition tests were conducted to investigate the presence of cross-reactivity between pollen-specific IgE antibodies and CCD-related antigens. Twenty samples that were positive for specific IgE to Japanese cedar, Japanese cypress, orchard grass or ragweed, and having a CCD-related antigen-specific IgE antibody titer ≥0.35 IUA/mL were evaluated. All 20 samples tested positive for the specific IgE to Japanese cedar and there was no inhibition by any of the CCD-related allergens (Table 4). Of 19 samples that were positive for specific IgE to Japanese cypress, 2 samples were inhibited by HRP (10.5%) (Table 4). Of 10 samples that were positive for specific IgE to orchard grass, 1 sample was inhibited by HRP (10%) (Table 4). Of 7 samples that were positive for specific IgE to ragweed, 1 sample (28.6%) was inhibited by HRP and ASOD each. No inhibition was induced by MUXF or bromelain (Table 4). These results demonstrate that Japanese cedar specific IgE antibodies do not cross-react with the CCD-related antigens used in this study. However, Japanese cypress and orchard grass specific IgE antibodies may have limited cross-reactivity with HRP, and ragweed specific IgE antibodies may have limited cross-reactivity with HRP and ASOD.
Wheat and soybean are important allergens in food allergies. It has been reported that soybean-specific IgE antibodies may also bind to CCD. As with pollen-specific IgE testing, it is known that there can be false positives for soybean, where patients may have no allergic symptoms despite the detection of specific IgE to soybean. In this study, we also investigated the relationship between food allergens (wheat and soybean) and CCD-specific IgE antibodies in 322 subjects. A small number of specific IgE positive results were observed for wheat in 5 (2%) and for soybean in 12 individuals (4%). Additionally, at least 1 type of CCD-related specific IgE antibody was detected for all samples (100%) (Table 5). However, none of these positive subjects had any subjective symptoms for soybean or wheat allergies.
In this study, first, we evaluated our patients who showed subjective symptoms of pollen allergy. The prevalence of pollen-specific IgE antibodies was 61.2% for Japanese cedar, 23.3% for orchard grass, and 8.5% for ragweed. Both pollen and CCD-related antigen specific IgE antibodies were detected in some patients. The detection rate for CCD-related antigen-specific IgE antibodies, where bromelain was more frequently detected than other CCDs, was higher in patients with ragweed pollen allergy than in those with orchard grass and Japanese cedar pollen allergies (Table 1). MUXF-specific IgE antibodies were detected more frequently in allergies to ragweed pollen than any other (Table 1). These results, from the viewpoint of antigenicity, suggest that epitopes are shared between ragweed pollen- and CCD-related allergen-specific IgE antibodies. These results also indicate that specific IgE antibodies to ragweed pollen and CCD related allergens antibodies are more likely to cross-react.
We also evaluated the detection rates for pollen- and CDD-specific IgE from the serum of company employees who attended their company's health screening. The prevalence of specific IgE antibodies to Japanese cedar, Japanese cypress, orchard grass, and ragweed pollen were almost the same, regardless of the presence of subjective symptoms (Table 2). In this study, the prevalence of specific IgE antibodies was high in patients without subjective symptoms. Interestingly, the prevalence of CCD-related antigen-specific IgE antibodies was equivalent to or slightly higher in the group without subjective symptoms than in the group with subjective symptoms (Table 3). It was unclear whether each of the pollen-specific IgE antibodies binds directly to the CCD-related antigens. However, these results suggest that cross-reactivity between pollen- and CCD-related allergen-specific IgE antibodies can be one of the causes of false positive results in specific IgE antibody testing.
We performed an in vitro experiment to evaluate the cross-reactivity between pollen-specific IgE antibodies and CCD-related antigens. As shown in Table 4, in this study, Japanese cedar pollen-specific IgE antibodies did not cross-react with any CCD-related antigens, suggesting that the reactivity of Japanese cedar-specific IgE antibodies to these allergens may significantly depend on the peptide structure (amino-acid sequences and conformation). Cross-reactivity was observed for Japanese cypress- and orchard grass-specific IgE antibodies with HRP, and for the ragweed-specific IgE antibody with HRP and ASOD in some cases (Table 4). This suggests that while the reactivity of these pollen-specific IgE antibodies most likely depended on the peptide structure of allergens, pollen-specific IgE antibodies for which reactivity depended on CCD may also have been produced in some patients. Thus, CCD can be clinically applied for developing therapeutic agents for treating patients with pollen-specific IgE antibodies that cross-react with CCD-related antigens. Specifically, administration of CCD-related antigens to patients with pollen allergy during the pollen seasons, may contribute to inhibiting the induction of type I hypersensitivity through the binding of IgE antibodies in those patients with the CCD-related antigens instead of the pollen allergens. To this end, it is inevitable to identify CCD-related antigens that are harmless to the human body and can bind efficiently to pollen-specific IgE antibodies.
To investigate a possible association with food allergy, we evaluated 12 patients who were positive for soybean-specific IgE antibodies and 5 patients who were positive for wheat-specific IgE antibodies, for the titers of CCD-specific IgE antibodies; it was found that all these patients were positive for CCD-specific IgE antibodies as well. However, these patients showed no subjective symptoms from soybean or wheat allergies; therefore, these results may be false positives due to the cross-reactivity of CCD-related antigen-specific IgE antibodies to soybean and/or wheat allergens. Hence, it is suggested that an epitope of a CCD-related antigen-specific IgE antibody is more similar to those of soybean- and wheat-specific IgE antibodies than to pollen-specific IgE antibodies. We also evaluated the expression of CCD-related antigen-specific IgE antibodies in a general population of Japanese adults in addition to patients with pollen allergy. It was demonstrated that the detection rate for CCD-related antigen-specific IgE antibodies in the general population was higher than those for soybean and wheat, even though it was not comparable to the pollen-specific IgE antibodies. The limitations of our work were that data from average adults was obtained by questionnaires. Ideally, all 322 employees can receive a medical check by a doctor, and also we can perform skin test as additional examination. These are next task.
Conventionally, while the cross-reactivity of CCD-related-specific IgE antibodies to pollen allergens was considered as one of the possible causes of false positives in pollen-specific IgE antibody testing, cross-reactivity was not actually observed with Japanese cedar pollen. However, it has been demonstrated that cross-reactivity can be slightly observed for ragweed, Japanese cypress, and orchard grass with HRP and ASOD. In conclusion, careful evaluation of patient IgE results should be performed for Japanese cypress, orchard grass, and ragweed.
Figures and Tables
Table 2
Positive rate of pollen-specific IgE antibodies based on subjective symptoms at the time of medical examination
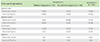
Table 3
Positive rate of CCD-specific IgE antibodies based on subjective symptoms at the time of medical examination
References
1. Costongs GM, Bas BM. The first fully automated allergy analyser UniCAP: comparison with IMMULITE for allergy panel testing. Eur J Clin Chem Clin Biochem. 1997; 35:885–888.
2. Aalberse RC, Akkerdaas J, van Ree R. Cross-reactivity of IgE antibodies to allergens. Allergy. 2001; 56:478–490.

3. Foetisch K, Westphal S, Lauer I, Retzek M, Altmann F, Kolarich D, Scheurer S, Vieths S. Biological activity of IgE specific for cross-reactive carbohydrate determinants. J Allergy Clin Immunol. 2003; 111:889–896.

4. van der Veen MJ, van Ree R, Aalberse RC, Akkerdaas J, Koppelman SJ, Jansen HM, van der Zee JS. Poor biologic activity of cross-reactive IgE directed to carbohydrate determinants of glycoproteins. J Allergy Clin Immunol. 1997; 100:327–334.

5. Mari A, Iacovacci P, Afferni C, Barletta B, Tinghino R, Di Felice G, Pini C. Specific IgE to cross-reactive carbohydrate determinants strongly affect the in vitro diagnosis of allergic diseases. J Allergy Clin Immunol. 1999; 103:1005–1011.

6. Maeda M, Kamamoto M, Hino K, Yamamoto S, Kimura M, Okano M, Kimura Y. Glycoform analysis of Japanese cedar pollen allergen, Cry j 1. Biosci Biotechnol Biochem. 2005; 69:1700–1705.

7. Kimura Y, Kamamoto M, Maeda M, Okano M, Yokoyama M, Kino K. Occurrence of Lewis a epitope in N-glycans of a glycoallergen, Jun a 1, from mountain cedar (Juniperus ashei) pollen. Biosci Biotechnol Biochem. 2005; 69:137–144.
8. Kimura Y, Kuroki M, Maeda M, Okano M, Yokoyama M, Kino K. Glycoform analysis of Japanese cypress pollen allergen, Cha o 1: a comparison of the glycoforms of cedar and cypress pollen allergens. Biosci Biotechnol Biochem. 2008; 72:485–491.

9. Ishihara H, Takahashi N, Oguri S, Tejima S. Complete structure of the carbohydrate moiety of stem bromelain. An application of the almond glycopeptidase for structural studies of glycopeptides. J Biol Chem. 1979; 254:10715–10719.

10. Mari A. IgE to cross-reactive carbohydrate determinants: analysis of the distribution and appraisal of the in vivo and in vitro reactivity. Int Arch Allergy Immunol. 2002; 129:286–295.

11. Ortolani C, Ispano M, Ansaloni R, Rotondo F, Incorvaia C, Pastorello EA. Diagnostic problems due to cross-reactions in food allergy. Allergy. 1998; 53:46 Suppl. 58–61.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download