Abstract
Background
Oral food challenge (OFC) tests are conducted in both specialized institutions and general hospitals. We aimed to compare the severity of the conditions of the patients between these 2 types of institutions in order to consider the role of such institutions in society.
Objective
We evaluated the results of OFC tests for hen's egg, cow's milk, and wheat that were conducted in a specialized institution (Aichi Children's Health and Medical Center [ACHMC], n = 835) and in 4 general hospitals (n = 327) in Aichi prefecture, Japan.
Methods
The symptoms provoked were scored using the total score (TS) of the Anaphylaxis Scoring Aichi scoring system in combination with the total ingested protein dose (Pro) before the appearance of allergic symptoms.
Results
The total ingested dose of the challenge-positive patients in ACHMC was significantly less than that in the general hospitals (p < 0.01). The median TS of the provoked symptoms in ACHMC and the general hospitals did not differ to a statistically significant extent in the hen's egg or cow's milk challenges; however, the median TS in ACHMC was significantly lower than that in the general hospitals for the wheat challenge (p = 0.02). The median TS/Pro values in ACHMC were almost identical to the upper 25% of the TS/Pro values in the general hospitals, suggesting that the specialized institution usually managed more severe patients.
The complete avoidance of allergenic foods is the standard strategy for managing food allergies throughout the world [12]. However, the Japanese Guidelines for Food Allergy 2017 (JGFA2017) recommend “minimal avoidance based on a precise diagnosis” as the principle for the management of food allergies [3]. It means that patients are encouraged to eat a tolerated amount of the allergenic food or processed foods with reduced allergenic activity. This principle is supported by the spread of oral food challenge (OFC) tests in Japan, not only to diagnose food allergies, but also to evaluate the threshold dose of the allergenic food, even in patients who have already diagnosed with food allergies [4].
Different types of institutions provide medical services for patients with allergies [5]. Primary care physicians will initially diagnose the food allergy, give simple guidance, and sometimes introduce selected patients to a local specialist. Local allergy specialists in a general hospital perform OFC tests and provide standard instructions based on the guidelines. Specialized institutions have a professional team to deal with more complicated and intractable cases, and also perform oral immunotherapies (OIT) [6].
It is desirable to follow patients with food allergies in the regional medical service because food allergies are a common, highly prevalent disease, and are closely related to a patient's daily life. Furthermore, most patients naturally gain tolerance before school age [789]. However, some patients exhibit anaphylaxis after the ingestion of a small amount of an allergen and do not easily gain tolerance. These patients should be treated in a specialized institution, because they require more precise dietary guidance or OIT.
A nationwide database showed that OFC tests were performed in 22 hospitals in Aichi prefecture (population: 7.5 million) in 2015; 13 of the hospitals performed more than 100 OFC tests per year. Among these hospitals, Aichi Children's Health and Medical Center (ACHMC) and Fujita Health University are considered to be specialized institutions; they perform more than 1,000 OFC tests per year and conduct clinical studies of OIT. Thus, this area has the potential to provide a stratified medical service system for patients with food allergies.
In this study, we aimed to compare the role of general hospitals and a specialized institution by evaluating the results of OFC tests that they performed. In the analysis, we employed our original scoring system, “Anaphylaxis Scoring Aichi (ASCA),” which enables the quantitative evaluation of multiorgan symptoms [10].
This study analyzed the results of OFC tests performed in one specialized institution (ACHMC) and four general hospitals in which an allergy specialist was in charge. ACHMC employs 9 doctors in the Department of Allergy and performs up to 8 OFC tests per day, 4 days a week. In contrast, an allergist in each general hospital performs 1 to 3 OFC tests per day, 1 to 3 times a week.
We collected the results of OFC tests performed for children under 16 years of age for hen's egg, cow's milk, and wheat between April 2014 and March 2015. We reviewed the OFC test results from ACHMC (n = 835) and 4 general hospitals (n = 327); Okazaki City Hospital (n = 114), Kasugai Municipal Hospital (n = 73), Tosei General Hospital (n = 89), and Toyota Kosei Hospital (n = 51).
Open OFC tests for hen's egg, cow's milk, and wheat were performed according to the JGFA 2014 [11] in each institution. Representative foods that were used in the challenges included boiled egg white, cow's milk, and udon noodles (for wheat); however, other cooking methods or processed foods containing a known amount of allergen were also used in some cases. The total dose of the target food was decided based on the patient's history and divided into 4 to 6 incremental doses every 20 to 40 minutes.
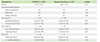
The severity of the provoked symptoms was scored using the total score (TS) of ASCA (Table 1). ASCA lists allergy symptoms in the 5 organ systems (respiratory, skin-mucosal, gastrointestinal, psycho-neurological, and cardio-vascular). Each organ score of 0–60 points was given in accordance with the Sampson's anaphylaxis grading system [1012]. An organ score of 10 points mostly corresponds to grade 2, suggesting the need of medication (oral antihistamines or inhalation of β-2 agonist). An organ score of 40 points suggests the need for the intramuscular injection of adrenaline. An organ score of 60 points corresponds to grade 4. TS is the sum of the highest 5 organ scores observed throughout the course of an OFC test (maximum, 240 points).
We have already evaluated the ASCA system in comparison with the Sampson's grading system [13]. TS significantly correlated to the Sampson's grading with some overlap between grades 2 and 3, because TS is a sum of multiorgan symptoms. On the other hand, clear discrimination of TS between grades 3 and 4 was obtained, because we employed the points in a gradient manner to distinguish a severe symptom in one organ from a sum of mild organ symptoms.
In the analysis, positive OFC test was defined as objective organ score ≥ 1. We defined “low dose” as a dose of <4 g (cumulative ingested dose), and “high TS” as a TS of ≥30 points. When the OFC test resulted in a negative result, the cumulative dose of the ingested allergen was evaluated.
We further employed a new indicator, “TS/Pro”, to allow the simultaneous expression of the severity of symptoms and the total ingested dose of theantigen [13]. “Pro” represents the cumulative protein dose (g) of the allergen that provoked symptoms, and the TS/Pro (point/g) was obtained by simply dividing the TS by the Pro value. The protein content was calculated based on the standard tables of food composition in Japan (seventh edition) [14]. According to this table, boiled egg white contains 11.3%, cow's milk contains 3.3% and udon noodle contains 2.6% protein. When whole egg was used for the egg challenge, we calculated the volume of egg white as two-thirds of the amount of whole egg, and the protein dose of egg white was applied to determine the TS/Pro value.
Specific IgE (sIgE) was examined using ImmunoCAP (Thermo Fisher Scientific, Uppsala, Sweden); a value of ≥0.35 kUA/L was considered to be positive. In the statistical analysis, ≥100 kUA/L was calculated as 100 kUA/L and <0.35 kUA/L was calculated as 0.34 kUA/L.
All of the statistical analyses were performed using Statcel 3 for Macintosh (OMS publication, Saitama, Japan). A univariate analysis was performed, with a Mann-Whitney U-test used for the sequential data and a chi-square test used for binary variables; p-values of <0.05 were considered to indicate statistical significance.
This study was performed in accordance with the Declaration of Helsinki, and was approved by the Ethical Committee of ACHMC (December 18, 2012), as well as the corresponding committees in the 4 general hospitals. Informed consent for the OFC test and enrollment in the study was obtained from the children's parents.
The median age of the subjects treated in ACHMC (4.2 years; range, 0.9–15.6 years) was older than that of the subjects in the general hospitals (2.6 years; range, 0.7–15.0 years; p < 0.05). The median levels of sIgE to the allergen foods in the subjects in ACHMC were higher in comparison to those in the general hospitals, with the exception of that in ω-5 gliadin. The prevalence of subjects with concomitant allergic diseases in ACHMC and the general hospitals did not differ to a statistically significant extent (Table 2).
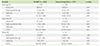
The rate of positive OFC test results in ACHMC was higher than that in the general hospitals for hen's egg (61.1% vs. 47.5%) and cow's milk (72.5% vs. 52.5%, p < 0.01) but not for the wheat challenge (Table 3). The total ingested dose of the challenge-positive patients in ACHMC was significantly less than that in the general hospitals (hen's egg, 3.5 g vs. 8.5 g; cow's milk, 3.7 mL vs. 18.5 mL; wheat, 3.7 g vs. 11.8 g, p < 0.01). The median TS of the provoked symptoms in ACHMC and the general hospitals did not differ to a statistically significant extent for the hen's egg (15 points vs. 15 points) or cow's milk (11 points vs. 10 points) challenges. However, in ACHMC, the TS provoked in the wheat challenge (10 points) was even lower than that in the general hospitals (15 points, p = 0.02) (Table 3).
The total ingested dose and TS were further evaluated (Figs. 1, 2, 3). The proportion of low-dose (<4 g) OFC-positive patients in ACHMC was higher than that in the general hospitals (hen's egg, 69% vs. 36%; cow's milk, 57% vs. 19%; wheat, 53% vs. 21%; p < 0.01). The proportion of high-TS (≥30 points) values in ACHMC and the general hospitals did not differ to a statistically significant extent (hen's egg, 21% vs. 23%; cow's milk, 12% vs. 24%; wheat, 8% vs. 15%).
To evaluate the TS and the total ingested dose simultaneously, the TS/Pro was compared between ACHMC and the general hospitals. In all of the hen's egg, cow's milk, and wheat challenges, the median levels of TS/Pro in ACHMC (53, 86, 103 points/g, respectively) were significantly higher than those in the general hospitals (6, 12, 20 points/g, respectively, p < 0.01) (Fig. 4). Furthermore, the median TS/Pro value in ACHMC tended to be higher than the 75th percentiles of the general hospitals (54, 50, 51 points/g, respectively). Conversely, the 25th percentiles of TS/Pro in ACHMC (13, 19, 38 points/g, respectively) tended to be higher than the median values in the general hospitals.
We evaluated the total ingested dose in the challenge-negative patients (Fig. 5). In the general hospitals, no patients showed a negative result in the low-dose challenge (<4 g). On the other hand, in the high-dose challenge (≥20 g of egg white and cow's milk), negative results were more frequently observed in the general hospitals (47% and 73%, respectively) than in ACHMC (17% and 37%, respectively).
We compared the results of OFC tests performed at a specialized institution (ACHMC) and 4 general hospitals. The age and allergen-specific IgE levels of the patients were significantly higher in ACHMC (Table 2), suggesting that ACHMC manages more severe and refractory patients in the area.
In the analysis, we employed our original scoring systems (ASCA and TS/Pro), which are advantageous for the statistical analysis of OFC test results [10]. Sampson's grading system [12] is widely used, but it is a semiquantitative index. Furthermore, many articles have reported the results of OFC tests based only on the severity of symptoms [15], regardless of the threshold dose. It may be effective to argue the safety of OFC tests; however, both the threshold dose and the severity of provoked symptoms are necessary to express the severity of a patient.
As a result, the total ingested dose in the challenge-positive patients, but not the TS, differed between ACHMC and the general hospitals (Table 3). This result was considered to be reasonable because an OFC test is always stopped when the initial mild (but definite) symptom is observed, and an appropriate treatment is given immediately [16].
There were no patients with negative results in the low-dose (<4 g) challenge in the general hospitals (Fig. 5), suggesting that low-dose challenges were rarely performed there. On the other hand, low-dose challenges were frequently performed in ACHMC, and some of them resulted in negative findings [17].
The PRACTALL consensus report proposes a standard OFC test protocol that is applicable worldwide [18]. It recommends a general challenge schedule consisting of 3, 10, 30, 100, 300, 1,000, and 3,000 mg of milk protein at intervals of at least 20 minutes. The cumulative dose is equivalent to 130 mL of cow's milk, which may be enough to rule out the diagnosis of milk allergy in challenge-negative patients. On the other hand, JGFA2017 recommends to apply a low-dose OFC test [3] to patients with a history of severe food allergy. JGFA2017 also suggests intervals of 20–60 minutes in order to avoid the over-dose beyond the threshold level [19]. This policy reflects the need to perform OFC tests even in the patients with severe food allergies in order to find the minimal ingestable dose.
ACHMC adopted this policy and the typical protocol of the low-dose challenge was 0.2-0.5-1-2 g every 40 minutes. The protocol for each patient was adjusted based on the precise history and laboratory data to ensure the safety of the patient [3]. If the low-dose OFC test resulted in a negative or mildly positive result, we propose the patient to start a low-dose intake, based on the approved OIT protocol [42021]. A registered dietitian, licensed as a pediatric allergy educator [22], was always in charge to help the patient consume the allergenic food at home.
On the other hand, the majority of OFC tests were performed for the initial diagnosis of food allergies or to confirm the acquisition of natural tolerance in the general hospitals. In those cases, a high-dose challenge was often performed, which might sometimes cause severe symptoms [23].
The analysis of the OFC test results reveals the role of each institution and helps to review the medical service system in the local area. The median TS/Pro values in ACHMC were almost identical to the upper 25% of the TS/Pro values in the general hospitals; suggesting that ACHMC managed more severe patients (Fig. 4).
This study is associated with some limitations. First, the OFC test protocols in the institutions were not identical; thus, the data was not completely compatible. However, as discussed above, each institution has its own reason for selecting a protocol. Second, we did not evaluate the indications for an OFC test in each hospital. In the general hospitals, a greater number of patients might not undergo an OFC test due to a history of severe allergic reactions. Third, the differences between the general hospitals were not evaluated because of the limited number of OFC tests in each hospital. Finally, this study was not a complete cross-sectional analysis of the area.
The Basic Law on Measures against Allergic Diseases in Japan (enforced in 2014) proclaimed that the medical treatment of allergic diseases should be given equally to individuals, regardless of the region in which they live. Although nationwide efforts have been conducted to provide countermeasures for food allergies [24], regional differences still exists in Japan because of the uneven distribution of allergy specialists [25]. To establish an appropriate medical supply for food allergy treatment, it is essential to construct a local OFC test network [25].
The methods applied in the present study could be a useful tool for comparing the activity of individual hospitals and for optimizing the distribution of patient to appropriate medical services.
Figures and Tables
 | Fig. 1The individual results of the hen's egg oral food challenges. The scatterplot shows the distribution of the total ingested dose (calculated as egg white) and the total score of Anaphylaxis Scoring Aichi. The vertical line indicates 4 g of total ingested dose and the horizontal line indicates a total score of 30 points. ACHMC, Aichi Children's Health and Medical Center. |
 | Fig. 2The individual results of the cow's milk oral food challenges. The scatterplot shows the distribution of the total ingested dose (calculated as milk) and the total score of Anaphylaxis Scoring Aichi. The vertical line indicates 4 mL of total ingested dose and the horizontal line indicates a total score of 30 points. ACHMC, Aichi Children's Health and Medical Center. |
 | Fig. 3The individual results of wheat oral food challenges. The scatterplot shows the distribution of the total ingested dose (calculated as udon noodle) and the total score of Anaphylaxis Scoring Aichi. The vertical line indicates 4 g of total ingested dose and the horizontal line indicates a total score of 30 points. ACHMC, Aichi Children's Health and Medical Center. |
 | Fig. 4The comparison of the TS/Pro values at Aichi Children's Health and Medical Center (ACHMC) and the general hospitals. The box plots indicate the median and interquartile range of the total score/protein dose (TS/Pro). The statistical significance of differences between the groups was determined using the Mann-Whitney U-test. |
 | Fig. 5The distribution of total ingested doses in the oral food challenge (OFC)-negative patients. The total ingested dose in the OFC-negative patients was compared between Aichi Children's Health and Medical Center (ACHMC) and the general hospitals. The horizontal bars indicate the prevalence of patients who showed a negative result after ingesting the designated total amount of allergenic food. |
ACKNOWLEDGEMENTS
This study was partially supported by the Practical Research Project for Allergic Disease and Immunology from the Japan Agency for Medical Research and Development, AMED (15ek0410019h0101).
References
1. Muraro A, Werfel T, Hoffmann-Sommergruber K, Roberts G, Beyer K, Bindslev-Jensen C, Cardona V, Dubois A, duToit G, Eigenmann P, Fernandez Rivas M, Halken S, Hickstein L, Høst A, Knol E, Lack G, Marchisotto MJ, Niggemann B, Nwaru BI, Papadopoulos NG, Poulsen LK, Santos AF, Skypala I, Schoepfer A, Van Ree R, Venter C, Worm M, Vlieg-Boerstra B, Panesar S, de Silva D, Soares-Weiser K, Sheikh A, Ballmer-Weber BK, Nilsson C, de Jong NW, Akdis CA. EAACI Food Allergy and Anaphylaxis Guidelines Group. EAACI food allergy and anaphylaxis guidelines: diagnosis and management of food allergy. Allergy. 2014; 69:1008–1025.

2. Boyce JA, Assa'ad A, Burks AW, Jones SM, Sampson HA, Wood RA, Plaut M, Cooper SF, Fenton MJ, Arshad SH, Bahna SL, Beck LA, Byrd-Bredbenner C, Camargo CA Jr, Eichenfield L, Furuta GT, Hanifin JM, Jones C, Kraft M, Levy BD, Lieberman P, Luccioli S, McCall KM, Schneider LC, Simon RA, Simons FE, Teach SJ, Yawn BP, Schwaninger JM. NIAID-Sponsored Expert Panel. Guidelines for the diagnosis and management of food allergy in the United States: summary of the NIAID-sponsored expert panel report. J Allergy Clin Immunol. 2010; 126:1105–1118.

3. Ebisawa M, Ito K, Fujisawa T. Committee for Japanese Pediatric Guideline for Food Allergy, The Japanese Society of Pediatric Allergy and Clinical Immunology, The Japanese Society of Allergology. Japanese guidelines for food allergy 2017. Allergol Int. 2017; 66:248–264.

4. Yanagida N, Okada Y, Sato S, Ebisawa M. New approach for food allergy management using low-dose oral food challenges and low-dose oral immunotherapies. Allergol Int. 2016; 65:135–140.

5. Ebisawa M, Nishima S, Ohnishi H, Kondo N. Pediatric allergy and immunology in Japan. Pediatr Allergy Immunol. 2013; 24:704–714.

6. Nurmatov U, Dhami S, Arasi S, Pajno GB, Fernandez-Rivas M, Muraro A, Roberts G, Akdis C, Alvaro-Lozano M, Beyer K, Bindslev-Jensen C, Burks W, du Toit G, Ebisawa M, Eigenmann P, Knol E, Makela M, Nadeau KC, O'Mahony L, Papadopoulos N, Poulsen LK, Sackesen C, Sampson H, Santos AF, van Ree R, Timmermans F, Sheikh A. Allergen immunotherapy for IgE-mediated food allergy: a systematic review and meta-analysis. Allergy. 2017; 72:1133–1147.

7. Savage JH, Matsui EC, Skripak JM, Wood RA. The natural history of egg allergy. J Allergy Clin Immunol. 2007; 120:1413–1417.

8. Skripak JM, Matsui EC, Mudd K, Wood RA. The natural history of IgE-mediated cow's milk allergy. J Allergy Clin Immunol. 2007; 120:1172–1177.

9. Keet CA, Matsui EC, Dhillon G, Lenehan P, Paterakis M, Wood RA. The natural history of wheat allergy. Ann Allergy Asthma Immunol. 2009; 102:410–415.

10. Hino A, Maeda T, Haneda Y, Kobayashi T, Yasui M, Kando N, Ito K. Establishment of “Anaphylaxis Scoring Aichi (ASCA),” a new symptom scoring system to be used in an oral food challenge (OFC). Arerugi. 2013; 62:968–979.
11. Urisu A, Ebisawa M, Ito K, Aihara Y, Ito S, Mayumi M, Kohno Y, Kondo N. Committee for Japanese Pediatric Guideline for Food Allergy, Japanese Society of Pediatric Allergy and Clinical Immunology. Japanese Society of Allergology. Japanese Guideline for Food Allergy 2014. Allergol Int. 2014; 63:399–419.

13. Sugiura S, Matsui T, Nakagawa T, Sasaki K, Nakata J, Kando N, Ito K. Development of a prediction model of severe reaction in boiled egg challenges. Allergol Int. 2016; 65:293–299.

14. Ministry of Education, Culture, Sports, Science and Technology. The standard tables of food composition. 7th ed. Tokyo: Ministry of Education, Culture, Sports, Science and Technology;2015.
15. Kamioka N, Nomura T, Kato T, Yoneyama M, Sobajima T, Tanida H, Morishita T, Sugiura S, Suda Y, Hirabayashi Y, Misawa C, Tanaka H, Mizuno M, Terada A, Kanda Y, Saitoh S. Probability curves for predicting symptom severity during an oral food challenge with wheat. Allergol Int. 2017; 66:627–628.

16. Perry TT, Matsui EC, Conover-Walker MK, Wood RA. Risk of oral food challenges. J Allergy Clin Immunol. 2004; 114:1164–1168.

17. Ito K. Diagnosis of food allergies: the impact of oral food challenge testing. Asia Pac Allergy. 2013; 3:59–69.

18. Sampson HA, Gerth van Wijk R, Bindslev-Jensen C, Sicherer S, Teuber SS, Burks AW, Dubois AE, Beyer K, Eigenmann PA, Spergel JM, Werfel T, Chinchilli VM. Standardizing double-blind, placebo-controlled oral food challenges: American Academy of Allergy, Asthma & Immunology-European Academy of Allergy and Clinical Immunology PRACTALL consensus report. J Allergy Clin Immunol. 2012; 130:1260–1274.
19. Yanagida N, Imai T, Sato S, Ebisawa M. Do longer intervals between challenges reduce the risk of adverse reactions in oral wheat challenges? PLoS One. 2015; 10:e0143717.

20. Okada Y, Yanagida N, Sato S, Ebisawa M. Better management of cow's milk allergy using a very low dose food challenge test: a retrospective study. Allergol Int. 2015; 64:272–276.

21. Okada Y, Yanagida N, Sato S, Ebisawa M. Better management of wheat allergy using a very low-dose food challenge: a retrospective study. Allergol Int. 2016; 65:82–87.

22. Masuko I. The role of allergy educator. Arerugi. 2012; 61:1054–1059.
23. Turner PJ, Mehr S, Joshi P, Tan J, Wong M, Kakakios A, Campbell DE. Safety of food challenges to extensively heated egg in egg-allergic children: a prospective cohort study. Pediatr Allergy Immunol. 2013; 24:450–455.

24. Ebisawa M. Management of food allergy in Japan “food allergy management guideline 2008 (revision from 2005)” and “guidelines for the treatment of allergic diseases in schools”. Allergol Int. 2009; 58:475–483.

25. Ito K. Establishment of the oral food challenge network. Arerugi. 2012; 61:1047–1053.
SUPPLEMENTARY MATERIAL
Supplementary Fig. 1
Abdominal pain face scale (FS). The degree of abdominal pain is expressed by this face scale in the Anaphylaxis Scoring Aichi sheet (Table 1).




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download