Abstract
Objective
The relationship between vitamin D and allergic rhinitis (AR) remains unclear. The present study investigated their association by examining serum 25-hydroxyvitamin D (25(OH)D) levels, blood eosinophils, and the expression of vitamin D receptors (VDR) on nasal mucosa in patients with AR.
Methods
A total of 32 patients with persistent AR and 25 controls were enrolled in this study. Serum 25(OH)D levels were detected by enzyme-linked immunosorbent assay, and eosinophils in the peripheral blood were examined by an automated hematology system, while VDR expression on inferior turbinate mucosa was assessed by immunohistochemistry. Furthermore, the correlation of serum 25(OH)D levels with blood eosinophils in persistent AR was analyzed.
Results
No significant difference in serum 25(OH)D levels was detected between the AR and control groups (p = 0.371). Interestingly, the serum 25(OH)D levels of the AR group were negatively correlated with blood eosinophil count and its proportion (p = 0.019 and p = 0.010, respectively) even when adjusting confounding factors including age, sex, body mass index, and the season of blood sampling. On the other hand, no significant difference in the expression levels of VDR on nasal mucosa was found between the AR group and the control group (p = 0.231).
Vitamin D receptors (VDR) are expressed in the skeletal system and in various extraskeletal tissues and cells. Furthermore, certain tissues and cells express the enzyme that converts the primary inactive form of vitamin D and 25-hydroxyvitamin D (25(OH)D) to the active form, 1,25-hydroxyvitamin D (1,25(OH)2D). A number of studies have investigated on the effect of vitamin D on metabolism in cancer, cardiovascular diseases, infectious diseases and immune disorders [12345].
Vitamin D exerts pleiotropic effects through VDRs that form vitamin D-responsive elements in the nucleus to produce traditional genomic effects. VDRs are also present at the cell membrane and exert rapid nongenomic responses through second messengers. VDRs at the cell membrane mediate effects on the pancreas, vascular smooth muscle, monocytes, and immune cells. To the best of our knowledge, the expression of VDR on nasal mucosa is has not been extensively investigated.
Serum 25(OH)D is the most abundant and stable form of vitamin D in human systemic circulation, and is typically considered to directly represent the serum vitamin D level. The serum 25(OH)D concentration is affected by age, season, diet, and latitude.
The associations between low levels of 25(OH)D and an increased risk of asthma, atopic dermatitis, and allergic rhinitis (AR) are controversial [67], and the effect of vitamin D on allergic diseases remains unclear. The current study aimed to examine the association between serum vitamin D levels and persistent AR.
The present study included 32 patients with persistent AR (AR group) and 25 nonallergic subjects (control group). All the participants underwent septoplasty surgery at the Affiliated Jiangyin Hospital, Medical College of Southeast University (Jiangsu, China) between February 2014 and January 2015. The patients with persistent AR were diagnosed clinically according to the Allergic Rhinitis and its Impact on Asthma guidelines [8]. The subjects had symptoms and signs of AR with positive skin-prick tests and/or were positive for serum specific IgE against common aeroallergens, without other nasal disorders, and allergic diseases (such as chronic rhinosinusitis, asthma, and eczema/atopic dermatitis). The subjects had not received any vitamin D supplementation within the 3 months prior to blood testing. This study was approved by the Institutional Review Board of the Affiliated Jiangyin Hospital, Medical School of Southeast University (approval number: 2013-118). Informed consent was obtained from all participants or their guardian.
Skin-prick tests were performed with a standard panel of common aeroallergens, including house dust mites, animal dander, cockroaches, fungi, and pollens. Positive (histamine) and negative (normal saline) controls were also used. A mean wheal diameter of 3 mm or more 20 minutes after application was considered a positive skin reaction. Serum total and specific IgE levels were detected using an Allergen Screen Test kit (MEDIWISS Analytic GmbH, Moers, Germany). Specific IgE levels equal to or greater than 0.7 kU/L were considered positive. Blood eosinophil count and its proportion were performed using Sysmex XE-2100 Automated Hematology system (TOA Medical Electronics, Kobe, Japan). The normal range for eosinophil count in peripheral blood was 0.02–0.5×109/L, and the normal proportion in white blood cell was 0.5%–5%.
Serum 25(OH)D was assayed by an enz yme-linked immunosorbent assay (ELISA; Cloud-Clone Corp., Katy, TX, USA) according to the manufacturer's instructions. The insufficient value was defined as 21–30 ng/mL, the deficient value was <21 ng/mL, and the normal value was>30 ng/mL [9]. For seasonal blood analysis, the seasons were defined as follows: spring (March, April, and May); summer (June, July, and August); autumn (September, October, and November) and winter (December, January, and February).
VDR expression on nasal mucosa was measured by immunohistochemical staining. Inferior turbinate mucosa tissues were collected from septoplasty surgical samples, fixed in 10% formaldehyde solution, embedded in paraffin blocks and cut into 3-µm-thick sections. Standard immunohistochemical stains for VDR (rabbit polyclonal antibody; Bioss Antibodies Inc., Woburn, MA, USA) were performed [10]. Accordingly, paraffin sections were deparaffinized in xylene and rehydrated through a graded ethanol series. Antigen retrieval was performed by heated citrate buffer in a pressure cooker. Endogenous peroxidases were blocked by treating the sections with 0.3% hydrogen peroxide for 30 minutes, followed by washing 3 times with phosphate buffered saline (PBS). Nonspecific binding was blocked by incubating sections with 10% goat serum for 20 minutes at room temperature. The rabbit anti-VDR primary polyclonal antibody was applied in a moist chamber overnight at 4℃. Following rewarming to room temperature for 15 minutes, the slides were washed 3 times for 5 minutes in PBS. Then, the sections were incubated with secondary antibody, (DAKO; Agilent Technologies Inc., Santa Clara, CA, USA) for 25 minutes at room temperature. Af ter 3 additional rinsing steps with PBS for 5 minutes, diaminobenzidine was applied to the sections. This was followed by rinsing of the slides in deionized water. Counter staining with hematoxylin was performed prior to dehydration and clearing. Cover slips were then added to the sections. Control staining with no primary antibody incubation was also performed.
The expression of VDR was assessed by a pathologist according to a semiquantitative reference scale, accounting for the intensity and proportion of immunoreactive cells in individual slides of nasal mucosa. The staining was scored as follows: No staining; weak (<50% cells stained light brown in color); moderate (between weak and strong), and strong (>70% cells obviously stained deep brown in color). A cell was considered ‘stained’ if there was a discrete brown color associated with the cell, and the color was different from the cells stained only with hematoxylin or above any background color.
Data were evaluated using SPSS ver. 16.0 (SPSS Inc., Chicago, IL, USA). Differences in the distribution of characteristics, including age, sex, body mass index (BMI), the season of blood sampling, serum 25(OH)D levels, and the VDR expression between the patients with AR and the control subjects were analyzed using independent-samples t test or contingency table chi-square tests. The value of serum 25(OH)D were converted into binary variable, and multiple regression models were used to estimate the effect of mean serum 25(OH)D level and demographic characteristics on blood eosinophil count and its proportion. p < 0.05 was considered to indicate a statistically significant difference.
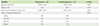
A total of 57 participants were included in the study: 32 in the AR group and 25 in the control group. The general characteristics of the subjects of the study are presented in Table 1. The majority of the participants were male (92%). There were no significant differences in age, sex, BMI, and the season of blood sampling between the 2 groups (all p > 0.05).
The difference in serum 25(OH)D levels between the AR group and the control group was not significant (t = -0.903, p = 0.371) (Table 2). There was also no significant difference in the proportion of participants with insufficient and deficient 25(OH) D levels (χ2 = 0.101, p = 0.751) (Table 2). Additionally, when female participants were excluded from the analysis, the difference in 25(OH)D levels between the 2 groups remained nonsignificant (t = -0.355, p = 0.724). Furthermore, there was no significant association between serum 25(OH)D levels and AR (odds ratio, 1.01; 95% confidence interval, 0.994–1.027; p = 0.235) when adjusting for age, sex, BMI, and the season of blood sampling as potential confounders.
The eosinophil count and its proportion in white blood cell samples from patients with AR were significantly higher than those of the control group (t = 3.081, p = 0.003, and t = 3.729, p < 0.0001, respectively) (Table 2). Interestingly, in AR group, the serum 25(OH)D levels were negatively correlated with blood eosinophil count and its proportion (p = 0.019 and p = 0.010, respectively) even when adjusting confounding factors including age, sex, BMI, and the season of blood sampling. However, the correlation was not significant in the control group (both p > 0.05).
In the majority of nasal mucosa samples, VDR expression was observed as moderate-to-strong staining. There was no significant difference in the expression level of VDR between the AR group and the control group (χ2 = 1.436, p = 0.231). Meanwhile, VDR expression was predominantly detected on the plasma membrane of epithelial cells in most samples, rather than in the cell nucleus and matrix (Fig. 1).
Vitamin D was proposed to play a protective role on immune system and respiratory infections [11121314]. A number of studies have previously investigated the immunoregulatory mechanisms of vitamin D [514]. Vitamin D functions in immune responses via VDR in the majority of immune cell types, including B cells, T cells, macrophages, dendritic cells, neutrophils, and eosinophils [1215]. However, vitamin D insufficiency and deficiency appear to be very common in general population without signs of nutritional rickets [16]. The present study identified that patients with persistent AR exhibited a lower serum level of 25(OH)D compared with the level in nonallergic subjects. The blood eosinophil count of the AR group was significantly higher than the control group. Meanwhile, the serum 25(OH)D levels of AR patients were inversely associated with the blood eosinophil count and its proportion in the regression models when adjusting for confounding factors (age, sex, BMI, and the season of blood sampling). However, the differences of serum 25(OH)D level between the 2 groups did not arrive statistical significance. This result might be due to a relatively higher mean serum 25(OH)D level and high standard deviation in control group. In addition, the expression of VDR on nasal mucosa in the 2 groups was similar.
Vitamin D impacts both innate and adaptive immune according to recent data. For the innate immune system, it stimulates the production of cathelicidin, which is an antimicrobial peptide [11]. As to adaptive immune, vitamin D reduces the production of T-helper type 1 (Th1) cells through suppressing IL-12 [12]. Meanwhile, different studies found vitamin D upregulates or deregulates expressions of interleukin (IL)-4 in different immune time. In vitro studies have demonstrated that vitamin D directly reduces IgE produced by peripheral human B cells [17]. However, certain studies failed to detect an inverse association between vitamin D and IgE levels [7]. Additionally, in vitro studies demonstrated that vitamin D may be involved in eosinophil recruitment to noninflammatory sites via regulation of C-X-C chemokine receptor type 4 expression in eosinophils [15]. These findings suggest that vitamin D may not be a direct factor in the pathogenesis of AR. In the current study, serum 25(OH) D levels were observed to be inversely associated with blood eosinophil count and its proportion in patients with persistent AR. A previous in vitro study reported results consistent with the findings of the present study. The previous study reported that vitamin D deficiency in neonatal mice contributed to the severity of airway hyper-responsiveness with increased eosinophilic inflammation; however, supplementation of vitamin D reduced pulmonary eosinophilia [18].
It is well established that 1,25(OH)2D, the activated form of 25(OH)D, causes genomic responses through interaction with the nuclear VDR; however, 1,25(OH)2D is also involved in rapid responses in a variety of cell types, including keratinocytes, chondrocytes and muscle cells [19]. The rapid responses take place within seconds to minutes inside the cells, resulting in the activation of various signaling pathways. To date, 2 receptors for 1,25(OH)2D have been identified to mediate these rapid responses: the VDR present on the plasma membrane, and membrane-associated protein disulfide isomerase family A member 3 [20]. These 2 receptors, when activated by 1,25(OH)2D, signal via different signaling pathways and initiate downstream cellular effects. Additionally, 1,25(OH)2D has been demonstrated to be capable of generating differently shaped ligands for the VDR, which allows it to select for different response arms: genomic or rapid responses [21]. Recent studies observed the pro- and anti-inflammatory properties of vitamin D in epithelial cells. Paplińska-Goryca et al. [22] found 1,25(OH)2D decreased the levels of IL-33 and IL-25 in cultured nasal epithelial cells. In inflammatory bowel disease, vitamin D also aids in sustaining the structural integrity of intestine epithelial cells while enhancing innate immune responses in the mucosa [23]. In the current study, VDR expression was predominantly detected on the plasma membrane in nasal epithelial cells. This might indicate that vitamin D plays a part role in intracellular signaling on nasal mucosa. Nevertheless, it is still unclear whether this nongenomic action of vitamin D regulated the immune responses of nasal mucosa [24].
The findings regarding the association between vitamin D levels and AR are inconclusive [14]. A study in Korean adults demonstrated that the serum 25(OH)D level in patients with AR was lower than the non-AR group, and the prevalence of AR steadily decreased in the patients with higher 25(OH)D [25]. Another study in Qatari children below the age of 16 identified that there was a higher prevalence of vitamin D deficiency (25(OH)D level < 10 ng/mL) in children with AR (18.5%) and asthma (17%) compared with in normal children (10.5%). Vitamin D deficiency was strongly associated with the allergic diseases [26]. However, a similar investigation in Korean adults reported that individuals with vitamin D insufficiency have an increased likelihood of having atopic dermatitis, but not allergic airway diseases, including AR and asthma [27]. A German study did not detect a decreased risk of AR and asthma with higher 25(OH) D levels in 10-year-old children; however, eczema and allergen-specific IgE levels were significantly correlated with those of vitamin D [28]. The results of the present study demonstrated that the serum 25(OH)D levels in the AR group were lower, but not significantly different to the control group. In addition, certain reports demonstrated that serum 25(OH)D were associated with AR in men and not in women [29], whereas others reported that male and female patients with AR had lower vitamin D levels [30]. The majority of subjects involved in the current study were male (92.0% and 84.4% in AR and control groups, respectively). If excluding female participants, the results remained statistically insignificant. Furthermore, our previous study investigating the polymorphisms of VDR observed that age and gender may have an impact on the genetic association of VDR polymorphisms with the risk of mite-sensitized persistent AR [31]. Wegienka et al. [32] reported that the association between vitamin D levels and allergy-associated outcomes, including eczema, skin-prick tests, and specific IgE levels, varied between different races: the results differed between Caucasian and black children. Therefore, the factors that influence vitamin D levels in patients with AR require further analysis in larger randomized studies, including identifying differences in sex, age, and race.
As for the effect of vitamin D supplementation on AR, studies are less and also inconclusive. A Danish cohort study involving midpregnancy (25 weeks) vitamin D intake from food and supplementation suggested no association with children AR at 18 months and 7 years but there was an inverse relationship between high total vitamin D intake and asthma at 7 years [33]. Another Finland birth cohort study found maternal vitamin D intake self-reported 5.1 ± 2.6 mg/day from food might be negatively associated with risk of asthma and AR at children by 5 years, but no association was found between vitamin D supplements alone and AR [34]. Bunyavanich et al. [35] also found food containing vitamin D in maternal diets rather than vitamin D supplements was associated with reduced odds of AR at school age. Regardless of the vitamin D supplementation, a recent study found vitamin D binding protein polymorphisms might lead to a racial difference of 25(OH)D level. Mean 25(OH)D levels of African American participants (77% with 25(OH)D < 20 ng/mL) were significantly lower than that of White Americans. However, African American have consistently higher bone mineral density and serum calcium than White Americans [36]. So whether or how 25(OH)D supplementation affecting the immunological disease are needed to be answered.
There are some limitations in our study. In the procedures of immunohistochemistry, we did not operate the intracellular staining, thus the staining might have been main observed in the cell membrane. In addition, the number of subjects in this study was small. These limitations need to be made up in further studies.
In conclusion, the present study suggests that serum 25(OH)D might be inversely associated with blood eosinophils in patients with persistent AR. However, the relationship between vitamin D and AR still requires further clarification.
Figures and Tables
 | Fig. 1Expression of vitamin D receptors on nasal mucosa (magnification, ×400). (A) The majority of epithelial cells of the nasal mucosa were moderately to strongly stained a distinct brown color. (B) Negative control staining. The expression scale was determined based on the intensity and proportion of immunoreactive cells in individual slides of the nasal mucosa, and was classified as no staining, weak, moderate, and strong. |
ACKNOWLEDGEMENTS
This work was supported by grants from the National Natural Science Foundation (81300834), the Priority Academic Program Development of Jiangsu Higher Education Institutions (JX10231801), and the Health Promotion Project of Jiangsu Province (RC2011071), the People's Republic of China. We thank Assistant Professor Yong-Ke Cao at the School of Foreign Languages of Nanjing Medical University for kind advice in the manuscript preparation.
References
1. Feldman D, Krishnan AV, Swami S, Giovannucci E, Feldman BJ. The role of vitamin D in reducing cancer risk and progression. Nat Rev Cancer. 2014; 14:342–357.

2. Lee TW, Lee TI, Chang CJ, Lien GS, Kao YH, Chao TF, Chen YJ. Potential of vitamin D in treating diabetic cardiomyopathy. Nutr Res. 2015; 35:269–279.

3. Mozos I, Marginean O. Links between Vitamin D deficiency and cardiovascular diseases. Biomed Res Int. 2015; 2015:109275.

4. Kearns MD, Alvarez JA, Seidel N, Tangpricha V. Impact of vitamin D on infectious disease. Am J Med Sci. 2015; 349:245–262.

5. Benson AA, Toh JA, Vernon N, Jariwala SP. The role of vitamin D in the immunopathogenesis of allergic skin diseases. Allergy. 2012; 67:296–301.

6. Bonanno A, Gangemi S, La Grutta S, Malizia V, Riccobono L, Colombo P, Cibella F, Profita M. 25-Hydroxyvitamin D, IL-31, and IL-33 in children with allergic disease of the airways. Mediators Inflamm. 2014; 2014:520241.

7. Yao TC, Tu YL, Chang SW, Tsai HJ, Gu PW, Ning HC, Hua MC, Liao SL, Tsai MH, Chiu CY, Lai SH, Yeh KW, Huang JL, Huang JL. PATCH study group. Suboptimal vitamin D status in a population-based study of Asian children: prevalence and relation to allergic diseases and atopy. PLoS One. 2014; 9:e99105.

8. Bousquet J, Khaltaev N, Cruz AA, Denburg J, Fokkens WJ, Togias A, Zuberbier T, Baena-Cagnani CE, Canonica GW, van Weel C, Agache I, Aït-Khaled N, Bachert C, Blaiss MS, Bonini S, Boulet LP, Bousquet PJ, Camargos P, Carlsen KH, Chen Y, Custovic A, Dahl R, Demoly P, Douagui H, Durham SR, van Wijk RG, Kalayci O, Kaliner MA, Kim YY, Kowalski ML, Kuna P, Le LT, Lemiere C, Li J, Lockey RF, Mavale-Manuel S, Meltzer EO, Mohammad Y, Mullol J, Naclerio R, O'Hehir RE, Ohta K, Ouedraogo S, Palkonen S, Papadopoulos N, Passalacqua G, Pawankar R, Popov TA, Rabe KF, Rosado-Pinto J, Scadding GK, Simons FE, Toskala E, Valovirta E, van Cauwenberge P, Wang DY, Wickman M, Yawn BP, Yorgancioglu A, Yusuf OM, Zar H, Annesi-Maesano I, Bateman ED, Ben Kheder A, Boakye DA, Bouchard J, Burney P, Busse WW, Chan-Yeung M, Chavannes NH, Chuchalin A, Dolen WK, Emuzyte R, Grouse L, Humbert M, Jackson C, Johnston SL, Keith PK, Kemp JP, Klossek JM, Larenas-Linnemann D, Lipworth B, Malo JL, Marshall GD, Naspitz C, Nekam K, Niggemann B, Nizankowska-Mogilnicka E, Okamoto Y, Orru MP, Potter P, Price D, Stoloff SW, Vandenplas O, Viegi G, Williams D. World Health Organization. GA(2)LEN. AllerGen. Allergic Rhinitis and its Impact on Asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2) LEN and AllerGen). Allergy. 2008; 63:Suppl 86. 8–160.
9. Bischoff-Ferrari HA, Giovannucci E, Willett WC, Dietrich T, Dawson-Hughes B. Estimation of optimal serum concentrations of 25-hydroxyvitamin D for multiple health outcomes. Am J Clin Nutr. 2006; 84:18–28.

10. Tian Y, Lv G, Yang Y, Zhang Y, Yu R, Zhu J, Xiao L, Zhu J. Effects of vitamin D on renal fibrosis in diabetic nephropathy model rats. Int J Clin Exp Pathol. 2014; 7:3028–3037.
11. Liu PT, Stenger S, Tang DH, Modlin RL. Cutting edge: vitamin D-mediated human antimicrobial activity against Mycobacterium tuberculosis is dependent on the induction of cathelicidin. J Immunol. 2007; 179:2060–2063.
12. Cassim R, Russell MA, Lodge CJ, Lowe AJ, Koplin JJ, Dharmage SC. The role of circulating 25 hydroxyvitamin D in asthma: a systematic review. Allergy. 2015; 70:339–354.

13. Baeke F, Takiishi T, Korf H, Gysemans C, Mathieu C. Vitamin D: modulator of the immune system. Curr Opin Pharmacol. 2010; 10:482–496.

15. Hiraguchi Y, Tanida H, Sugimoto M, Hosoki K, Nagao M, Tokuda R, Fujisawa T. 1,25-Dihydroxyvitamin D3 upregulates functional C-x-C chemokine receptor type 4 expression in human eosinophils. Int Arch Allergy Immunol. 2012; 158:Suppl 1. 51–57.
16. Rosen CJ. Clinical practice. Vitamin D insufficiency. N Engl J Med. 2011; 364:248–254.
17. Hartmann B, Heine G, Babina M, Steinmeyer A, Zügel U, Radbruch A, Worm M. Targeting the vitamin D receptor inhibits the B cell-dependent allergic immune response. Allergy. 2011; 66:540–548.

18. Vasiliou JE, Lui S, Walker SA, Chohan V, Xystrakis E, Bush A, Hawrylowicz CM, Saglani S, Lloyd CM. Vitamin D deficiency induces Th2 skewing and eosinophilia in neonatal allergic airways disease. Allergy. 2014; 69:1380–1389.
19. Chen J, Olivares-Navarrete R, Wang Y, Herman TR, Boyan BD, Schwartz Z. Protein-disulfide isomerase-associated 3 (Pdia3) mediates the membrane response to 1,25-dihydroxyvitamin D3 in osteoblasts. J Biol Chem. 2010; 285:37041–37050.

20. Nemere I, Farach-Carson MC, Rohe B, Sterling TM, Norman AW, Boyan BD, Safford SE. Ribozyme knockdown functionally links a 1,25(OH)2D3 membrane binding protein (1,25D3-MARRS) and phosphate uptake in intestinal cells. Proc Natl Acad Sci U S A. 2004; 101:7392–7397.

21. Norman AW. Minireview: vitamin D receptor: new assignments for an already busy receptor. Endocrinology. 2006; 147:5542–5548.
22. Paplińska-Goryca M, Nejman-Gryz P, Proboszcz M, Krenke R. The effect of 1,25-dihydroxyvitamin D3 on TSLP, IL-33 and IL-25 expression in respiratory epithelium. Eur Cytokine Netw. 2016; 27:54–62.
23. Abdo J, Rai V, Agrawal DK. Interplay of immunity and vitamin D: interactions and implications with current IBD therapy. Curr Med Chem. 2017; 24:852–867.

25. Jung JW, Kim JY, Cho SH, Choi BW, Min KU, Kang HR. Allergic rhinitis and serum 25-hydroxyvitamin D level in Korean adults. Ann Allergy Asthma Immunol. 2013; 111:352–357.

26. Bener A, Ehlayel MS, Bener HZ, Hamid Q. The impact of vitamin D deficiency on asthma, allergic rhinitis and wheezing in children: an emerging public health problem. J Family Community Med. 2014; 21:154–161.

27. Cheng HM, Kim S, Park GH, Chang SE, Bang S, Won CH, Lee MW, Choi JH, Moon KC. Low vitamin D levels are associated with atopic dermatitis, but not allergic rhinitis, asthma, or IgE sensitization, in the adult Korean population. J Allergy Clin Immunol. 2014; 133:1048–1055.

28. Wawro N, Heinrich J, Thiering E, Kratzsch J, Schaaf B, Hoffmann B, Lehmann I, Bauer CP, Koletzko S, von Berg A, Berdel D, Linseisen J. Serum 25(OH)D concentrations and atopic diseases at age 10: results from the GINIplus and LISAplus birth cohort studies. BMC Pediatr. 2014; 14:286.

29. Mai XM, Langhammer A, Camargo CA Jr, Chen Y. Serum 25-hydroxyvitamin D levels and incident asthma in adults: the HUNT Study. Am J Epidemiol. 2012; 176:1169–1176.

30. Arshi S, Ghalehbaghi B, Kamrava SK, Aminlou M. Vitamin D serum levels in allergic rhinitis: any difference from normal population? Asia Pac Allergy. 2012; 2:45–48.

31. Tian HQ, Chen XY, Lu Y, Lu WM, Wang ML, Zhao HL, Lu MP, Zhou H, Chen RX, Zhang ZD, Shen C, Cheng L. Association of VDR and CYP2R1 polymorphisms with mite-sensitized persistent allergic rhinitis in a Chinese population. PLoS One. 2015; 10:e0133162.

32. Wegienka G, Havstad S, Zoratti EM, Kim H, Ownby DR, Johnson CC. Association between vitamin D levels and allergy-related outcomes vary by race and other factors. J Allergy Clin Immunol. 2015; 136:1309–1314. 1314.e1–1314.e4.

33. Maslova E, Hansen S, Jensen CB, Thorne-Lyman AL, Strøm M, Olsen SF. Vitamin D intake in mid-pregnancy and child allergic disease: a prospective study in 44,825 Danish mother-child pairs. BMC Pregnancy Childbirth. 2013; 13:199.

34. Erkkola M, Kaila M, Nwaru BI, Kronberg-Kippilä C, Ahonen S, Nevalainen J, Veijola R, Pekkanen J, Ilonen J, Simell O, Knip M, Virtanen SM. Maternal vitamin D intake during pregnancy is inversely associated with asthma and allergic rhinitis in 5-year-old children. Clin Exp Allergy. 2009; 39:875–882.

35. Bunyavanich S, Rifas-Shiman SL, Platts-Mills TA, Workman L, Sordillo JE, Camargo CA Jr, Gillman MW, Gold DR, Litonjua AA. Prenatal, perinatal, and childhood vitamin D exposure and their association with childhood allergic rhinitis and allergic sensitization. J Allergy Clin Immunol. 2016; 137:1063–1070.e2.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download