Abstract
Background
Chronic obstructive pulmonary disease (COPD) is now recognized as a systemic disorder with many comorbidities. Atopy in patients with COPD and upper airways symptoms has not been characterized.
Objective
We investigated the occurrence and impact of aeroallergen sensitisation in patients with COPD and upper airways symptoms.
Methods
All 41 subjects with COPD diagnosed as per Global Initiative for Chronic Obstructive Lung Disease guidelines, underwent spirometry with reversibility, computed tomography of the paranasal sinuses (CT-PNS), skin prick test (SPT) against common aeroallergens and responded to St. George's Respiratory Questionnaire (SGRQ) and Sino Nasal Outcome Test - 22 (SNOT-22) questionnaires. Upper airways symptoms were assessed as per the Allergic Rhinitis and its Impact on Asthma guidelines.
Results
As documented earlier, 27 of the 41 patients (65.9%) with COPD had upper airways symptoms. Of these 27 patients, 11 had SPT positivity against at least one aeroallergen (group 1). One patient had monosensitisation to pollens of grass Imperata while polysensitisation was seen in 10/11 patients commonly to weeds, trees, and insects. Fungal sensitisation to Aspergillus fumigatus was seen in 3 of 11 patients (27.2%). In group 1, all 11 patients (100%) had radiological sinusitis as compared to 8 of 16 (50%) in group 2. The mean CT-PNS scores were significantly higher in group 1 as compared to group 2. Similarly, the SNOT-22 scores were significantly higher in group 1 as compared to group 2. However, there was no difference in SGRQ scores between the 2 groups. In group 1, there was a significant correlation between CT-PNS and SNOT-22 scores.
Conclusion
Patients with COPD, associated upper airways symptoms and a positive SPT had a significantly higher frequency of radiological sinusitis on CT-PNS. They even had worse quality of life as compared to those with a negative SPT. The study suggested that atopic patients with COPD and upper airways involvement were more symptomatic. It is therefore possible that upper airways symptoms, if left untreated, would result in less than desirable control of the disease.
“Bronchodilation and emphysema” were the terms used by Laennec [1] in 1819 to describe the anatomical changes that we now recognize as chronic obstructive pulmonary disease (COPD). It is well known that COPD affects many systems and is now considered as a systemic disorder [2]. A mounting body of evidence has highlighted the occurrence of upper airways symptoms in patients with COPD, a feature that would undoubtedly add to the morbidity of the disease [3]. The prevalence of upper airways symptoms in patients with COPD is estimated to vary from 40%–88% [4567].
Atopy refers to a heightened predisposition to develop an allergic response on exposure to allergens. Orie and Sluiter [8] from The Netherlands first highlighted the concept of atopy in patients with COPD in 1961. He envisaged that both COPD and asthma were different expressions of the same disease entity. This concept suggests that atopy and bronchial hyperresponsiveness were involved in the pathogenesis of COPD and this surmise was popularized by Fletcher and Pride [9] as the “Dutch hypothesis.” Patients with atopy have a greater degree of reversibility on spirometry, better response to inhaled steroids but a higher exacerbation rate [10]. The frequency of atopy in COPD has been reported in 18%–42% [111213] of patients. In this same group of 41 patients with COPD, we had earlier reported that upper airways symptoms occurred in 27 (65%) and that these patients had a poorer QoL [14]. We now present data in these patients on the frequency and effect of sensitization to common aeroallergens in terms of computed tomography of the paranasal sinuses (CT-PNS) scores and its impact on QoL. To our knowledge, these aspects are yet to be documented.
This study recruited newly referred smokers, 35 years and above diagnosed with COPD as per the Global Initiative for Chronic Obstructive Lung Disease [2] guidelines (postbronchodilator forced expiratory volume in one second [FEV1]/forced vital capacity [FVC] < 70%). Patients were stable and ambulatory but those with significant reversibility on spirometry or with complications like respiratory failure, cor pulmonale, or significant comorbidities were excluded. In addition, patients with respiratory symptoms since childhood and persisting up to 35 years of age were also excluded. Allergic Rhinitis and its Impact on Asthma [15] workshop report was used to assess and document the presence of upper airways symptoms in these patients.
Cardinal symptoms of respiratory diseases and upper airways symptoms were recorded in all patients. They were also subjected to spirometry with reversibility testing [16], SPT against common aeroallergens [17] and noncontrast CT-PNS. CT-PNS was scored as per the staging system enunciated by Lund and Kennedy [18]. Each sinus group was graded as 0 (no abnormality), 1 (partial opacification), and 2 (total opacification). The ostiomeatal complex scored only as 0 (not occluded) or 2 (occluded).
QoL in these patients were assessed through St. George's Respiratory Questionnaire (SGRQ) [19] and Sino Nasal Outcome Test - 22 (SNOT-22) [20] questionnaires. Subjects who had received oral corticosteroids and/or antihistaminic drugs within a month prior to enrollment were excluded. None had ever used inhaled medications and/or intranasal corticosteroid sprays prior to inclusion
Patients with COPD and upper airways symptoms were divided into 2 groups: group 1, those with positive SPT against at least one aero-allergen; group 2, those with negative SPT. In both groups, radiological sinusitis was defined as per the European Position Paper on Rhinosinusitis and Nasal Polyps 2012 [21] criteria along with relevant clinical and CT-PNS findings.
Patients were recruited after obtaining voluntary, informed and written consent. The study was approved by the institutional human ethics committee.
SPT was performed against 67 aero-allergens commonly encountered in our surroundings. The various groups of allergens included pollens (grasses, trees, weeds), dust (including house dust mite), fungi, and insects. Histamine dihydrochloride (10 mg/mL) was used as a positive control and while buffered saline was used as negative control. These allergens including positive and negative controls were applied on the volar aspect of the forearm and read 15–20 minutes post application. A wheal diameter ≥ 3 mm greater than the negative control was considered to be positive [17].
A datasheet detailing all the cardinal respiratory as well as upper airways symptoms and the information regarding presence and duration of the above symptoms along with smoking habits was filled in for all patients by the same investigator. QoL assessment was done through SGRQ [19] and SNOT-22 [20] questionnaires. Investigations for all patients were recorded along with the questionnaires.
SGRQ [19] comprises 50 items with 76 weighted responses with three subclasses: symptoms (8 items), activity (16 items), and impacts (26 items). Symptoms deal with the frequency and the severity of respiratory manifestations, activity relates to activities that cause or are limited by breathlessness and impacts covers aspects of social functions and psychosocial disturbances. Scores for all these subclasses as well as overall score was calculated. For each subscale and for overall questionnaire, scores range from 0 to 100 (nil to maximum impairment).
SNOT-22 [20] questionnaire comprising 22 items, graded on a 5-point scale from “no problem” to “problem as bad as it can be,” assessed rhinosinusitis and its impact. The resultant sum was divided by 22 to yield SNOT-22 scores between 0 and 5.
Data was analyzed with SPSS ver. 11.5 (SPSS Inc., Chicago, IL, USA). Differences in symptoms, CT-PNS scoring, SNOT-22 and SGRQ scores between patients in both the groups were analyzed using the chi-square test. Student t test was used for continuous data. Pearson correlation test determined the correlation between CT-PNS and SNOT-22 scores. A significance level of p < 0.05 was accepted for all analysis.
Of the total of 41 consecutive patients with COPD including two females, 27 (65.9% [26 male and 1 female patient]; mean age, 55.7 years) had upper airways symptoms. Of these 27 patients with upper airways symptoms, 11 (40.7%) had a positive SPT (group 1). The demographic characteristics are detailed in Table 1.
The clinical symptomatology including the upper airways symptoms and the cardinal respiratory symptoms have been documented in Table 2. There was no significant difference in the mean duration of symptoms in both groups (group 1 vs. group 2, 5.7 ± 4.6 vs. 9.8 ± 9.1; p = 0.18).
The baseline characteristics of patients are depicted in Table 1. There was no significant difference in age of onset, disease duration, smoking characteristics, postbronchodilator FVC and FEV1/FVC ratio between the 2 groups. Absolute eosinophil counts were significantly higher in group 1 patients as compared to those in group 2 (p = 0.001).
Radiological sinusitis on CT-PNS was observed in 19 of 27 patients (70.4%) with upper airways symptoms while mucosal thickening was detected in 3 of 14 patients (21.4%) in those without upper airways symptoms (p = 0.003). Radiological sinusitis was seen in all 11 patients (100%) in group 1 as compared to 8 of 16 patients (50%) in group 2 (p = 0.005). Mean CT-PNS scores in group 1 was significantly higher (4.18 ± 3.54 vs. 0.81 ± 1.05, p = 0.001).
SPT was positive in 11 of 27 patients (40.7%) with upper airways symptoms (group 1) while it was positive in only 1 patient (1 of 14, 7.1%) in those without upper airways symptoms (p = 0.02). In group 1, mono sensitisation was seen in 1 of 11 patients (against Imperata) while 10 of 11 patients had poly sensitisation. Sensitisation to only 1 group of allergen was seen in 1 of 11 patients, 5 aeroallergen groups in 3 of 11 patients, 6 groups in 5 of 11 patents and 7 groups in 2 of 11 patients. Sensitisation to pollens of weeds and trees was seen in 10 of 11 patients (90.9%) each and those of grasses in 8 of 11 (72.7%). This was followed by sensitisation to insects in 10 of 11 (90.9%), dust in 9 of 11 (81.8%), fungal allergens in 8 of 11 (72.7%), and house dust mite in 6 of 11 patients (54.6%). The most common allergen among grasses was Sorghum in 5 of 11 (45.5%), among weeds Adhatoda in 5 of 11(45.5%), and in trees Holoptelia in 4 of 11 patients (36.4%). The most common allergen in dust group included house dust and wheat dust in 5 of 11 patients (45.5%) each. Among the fungal allergens, sensitisation to Fusarium was most common in 4 of 11 patients (36.4%) followed by Aspergillus fumigatus in 3 of 11 patients (27.2%). House fly and mosquito were the most common insect allergen to which sensitisation was seen in 6 of 11 patients (54.6%) each.
There was no significant difference in the total SGRQ as well as symptoms, activity and impact scores between the 2 groups.
The SNOT-22 scores were significantly higher in group 1 than group 2 (1.15 ± 0.23 vs. 0.67 ± 0.30, p = 0.0002). In those with a positive SPT (group 1) and radiological sinusitis (11 of 11), there was a strong positive correlation between CT-PNS and SNOT-22 scores (r = 0.70, p = 0.01).
There was no significant difference in the SGRQ total (group 1 vs. group 2, 55.6 ± 18.2 vs. 57.5 ± 23; p = 0.84), symptom (group 1 vs. group 2, 61.2 ± 22.62 vs. 71.4 ± 17.1; p = 0.27), activity (group 1 vs. group 2, 72.7 ± 17.9 vs. 80.1 ± 23.5; p = 0.44), and impact score (group 1 vs. group 2, 40.9 ± 22.9 vs. 43.5 ± 24.7; p = 0.81) between patients with radiological sinusitis in groups 1 and 2. However, the SNOT-22 scores were significantly higher in patients with radiological sinusitis in group 1 as compared to group 2 patients (group 1 vs. group 2, 1.15 ± 0.23 vs. 0.56 ± 0.30; p = 0.0001).
The occurrence of upper airways symptoms in patients with COPD is yet to receive the attention it deserves. As documented earlier, upper airways symptoms were observed in two-thirds of the 41 patients with COPD (27 of 41, 65.9%) [14]. The presence of these symptoms had significantly impacted the QoL as evidenced by SGRQ [19] and SNOT-22 [20] scores. A postal questionnaire survey in 392 patients with self-reported chronic bronchitis or emphysema documented recurrent or permanent nasal complaints in 40% subjects [4]. In more specific studies, the frequency of upper airways symptoms ranged from 42%–88% [567]. In the East London COPD rolling cohort study, 88% of the 65 patients had one or the other upper airways symptoms [6].
Cigarette smoke, the major offending agent for COPD, causes upper airways inflammation and results in increased goblet cell hypertrophy and submucosal gland hyperplasia resulting in excessive mucus production from nasal mucosal lining [22]. It also reduces muco-ciliary clearance [23]. Increased nasal inflammation has been documented in COPD patients with greater nasal neutrophil activity after histamine challenge in those with nasal symptoms than those without [24]. Nasal inflammation is known to persist even after smoking cessation [25].
In our patients with upper airways symptoms, SPT was positive in 11 of 27 (40.7%) as compared to 1 of 14 patients (p = 0.02) in those without indicating an element of an atopic background. Based only on clinical evaluation, a study from France [7] too reported similar observation. The authors had suggested that “atopy is indeed involved in chronic nasal symptoms among COPD patients” and they further stated that “atopy was defined on a purely clinical basis with no confirmation by skin prick tests or radioallergosorbent test (specific immunoglobulin E dosage)” [7]. Atopy in patients with COPD has been documented previously. In a study from Brazil [13], 62 of 149 patients (41.6%) with COPD had an evidence of atopy based on positive SPT/symptoms of allergic rhinitis along with eosinophilia on nasal lavage. In a recent longitudinal population based study from Sweden [26], smoking and atopy based on a positive Phadiatop test (odds ratio, 1.6) were considered as risk factors for development of noninfectious rhinitis in patients with COPD. Earlier, we too had documented a patient with COPD and concomitant allergic bronchopulmonary aspergillosis with positive intradermal tests against Aspergillus flavus and A. fumigatus suggesting type I hypersensitivity [27]. On further analysis, in the 11 patients with radiological sinusitis on CT-PNS and positive SPT, a greater degree of sinusitis was documented as evidenced by significantly higher CT-PNS scores as compared to those with a radiological sinusitis and negative SPT.
Asthma-COPD overlap syndrome (ACOS) is a recently recognised clinical entity which has overlapping features of both asthma as well as COPD. The diagnostic criteria for ACOS [28] formulated at a global expert roundtable discussion during the 2015 American Thoracic Society Congress included a set of six criterias. This comprised 3 major criteria: (1) persistent airflow limitation (postbronchodilator FEV1/FVC < 0.7) in individuals ≥ 40 years of age, (2) tobacco smoking (10 pack-years or more) or equivalent indoor/outdoor air pollution exposure, (3) documented history of asthma before 40 years of age or bronchodilator reversibility (BDR) > 400 mL in FEV1; and 3 minor criteria as (1) documented history of atopy/allergic rhinitis, (2) BDR >200 mL and 12% from baseline in FEV1 on 2 or more visits, and (3) peripheral blood eosinophil count of 300 cells/mm3. A diagnosis of ACOS can be established based on presence of all three major criteria and one of the minor criterion. ACOS was ruled out in our patients with COPD as (1) no enrolled patient had symptoms suggestive of asthma in the childhood, (2) all patients had developed symptoms after attaining the age of 35 years, and (3) BDR was an exclusion criteria.
In our study, there was no significant difference in SGRQ scores in patients with upper airways symptoms with/without positive SPT. A study from Brazil too did not find any significant difference in QoL in those with / without atopy [13]. Mean SNOT-22 scores in our group 1 patients were significantly higher (p = 0.0002) highlighting the negative impact of atopy in COPD patients with upper airways symptoms. In addition, in these patients, CT-PNS scores showed a moderately strong positive correlation with SNOT-22 scores. Those with higher CT-PNS scores and positive SPT had worse QoL. Previous studies have reported lower mean SNOT-20/SNOT-22 scores in patients with COPD and upper airways symptoms signifying that nasal symptoms impaired QoL [2930]. However, these studies did not evaluate for atopy. The small sample size and absence of radioallergosorbent test were the limitations of this study.
In conclusion, our study highlights that patients with COPD and associated upper airways symptoms along with positive SPT had a higher frequency of radiological sinusitis on CT-PNS and worse QoL. A significant correlation was seen between scores of CT-PNS and SNOT-22 suggesting an impaired QoL due to upper airways symptoms seen in COPD patients. Atopy was prevalent in patients with COPD with upper airways symptoms and is a potentially relevant component affecting the QoL by influencing the upper airways. Since COPD and rhinosinusitis are two diseases often treated by two different specialties, the occurrence of upper airways symptoms in patients with COPD may easily be overlooked. It is possible that if upper airways symptoms are left untreated in these patients, therapy for COPD would possibly be less than effective.
Figures and Tables
Table 1
Demographic, baseline characteristics and quality of life scores in patients with COPD and upper airways symptoms
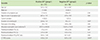
Values are presented as mean ± standard deviation or number (%).
COPD, chronic obstructive pulmonary disease; SPT, skin prick test; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; CT-PNS, computed tomography of the paranasal sinuses.
*p < 0.05, statistically significant difference.
References
1. Laennec RT. A treatise on the diseases of the chest. New York: Hafner Publishing;1962.
2. GOLD 2017 Global Strategy for the Diagnosis, Management and Prevention of COPD [Internet]. Washington, DC: Global Initiative for Chronic Obstructive Lung Disease;2016. cited 2017 Mar 6. Available from: http://goldcopd.org/gold-2017-global-strategy-diagnosismanagement-prevention-copd/.
3. Shah A. Nosing around in chronic obstructive pulmonary disease. Indian J Chest Dis Allied Sci. 2011; 53:5–7.
4. Montnémery P, Svensson C, Adelroth E, Löfdahl CG, Andersson M, Greiff L, Persson CG. Prevalence of nasal symptoms and their relation to self-reported asthma and chronic bronchitis/emphysema. Eur Respir J. 2001; 17:596–603.

5. Roberts NJ, Lloyd-Owen SJ, Rapado F, Patel IS, Wilkinson TM, Donaldson GC, Wedzicha JA. Relationship between chronic nasal and respiratory symptoms in patients with COPD. Respir Med. 2003; 97:909–914.

6. Hurst JR, Wilkinson TM, Donaldson GC, Wedzicha JA. Upper airway symptoms and quality of life in chronic obstructive pulmonary disease (COPD). Respir Med. 2004; 98:767–770.

7. Caillaud D, Chanez P, Escamilla R, Burgel PR, Court-Fortune I, Nesme-Meyer P, Deslee G, Perez T, Pinet C, Roche N. Initiatives BPCO Scientific Committee and Investigators. Association of chronic nasal symptoms with dyspnoea and quality-of-life impairment in chronic obstructive pulmonary disease. Respirology. 2014; 19:346–352.

8. Orie NG, Sluiter HJ, editors. Bronchitis I. Springfield (IL): Charles C Thomas;1961.
9. Fletcher CM, Pride NB. Definitions of emphysema, chronic bronchitis, asthma, and airflow obstruction: 25 years on from the Ciba symposium. Thorax. 1984; 39:81–85.

10. Postma DS, Weiss ST, van den Berge M, Kerstjens HA, Koppelman GH. Revisiting the Dutch hypothesis. J Allergy Clin Immunol. 2015; 136:521–529.

11. Pauwels RA, Löfdahl CG, Laitinen LA, Schouten JP, Postma DS, Pride NB, Ohlsson SV. Long-term treatment with inhaled budesonide in persons with mild chronic obstructive pulmonary disease who continue smoking. European Respiratory Society Study on Chronic Obstructive Pulmonary Disease. N Engl J Med. 1999; 340:1948–1953.
12. Watson L, Schouten JP, Löfdahl CG, Pride NB, Laitinen LA, Postma DS. European Respiratory Society Study on Chronic Obstructive Pulmonary Disease. Predictors of COPD symptoms: does the sex of the patient matter? Eur Respir J. 2006; 28:311–318.

13. Neves MC, Neves YC, Mendes CM, Bastos MN, Camelier AA, Queiroz CF, Mendoza BF, Lemos AC, D'Oliveira Junior A. Evaluation of atopy in patients with COPD. J Bras Pneumol. 2013; 39:296–305.

14. Kumar A, Kunal S, Shah A. Incidence and impact of upper airway symptoms in patients with chronic obstructive pulmonary disease. Arch Bronconeumol. 2017; 07. 01. DOI: 10.1016/j.arbres.2017.03.001.[Epub].

15. Brozek JL, Bousquet J, Baena-Cagnani CE, Bonini S, Canonica GW, Casale TB, van Wijk RG, Ohta K, Zuberbier T, Schünemann HJ. Global Allergy and Asthma European Network. Grading of Recommendations Assessment, Development and Evaluation Working Group. Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines: 2010 revision. J Allergy Clin Immunol. 2010; 126:466–476.
16. Global Initiative for Asthma. 2017 GINA report, global strategy for asthma management and prevention [Internet]. Global Initiative for Asthma;2016. cited 2017 Mar 6. Available from: http://ginasthma.org/2017-gina-report-global-strategy-for-asthma-managementand-prevention/.
17. Bousquet J, Heinzerling L, Bachert C, Papadopoulos NG, Bousquet PJ, Burney PG, Canonica GW, Carlsen KH, Cox L, Haahtela T, Lodrup Carlsen KC, Price D, Samolinski B, Simons FE, Wickman M, Annesi-Maesano I, Baena-Cagnani CE, Bergmann KC, Bindslev-Jensen C, Casale TB, Chiriac A, Cruz AA, Dubakiene R, Durham SR, Fokkens WJ, Gerth-van-Wijk R, Kalayci O, Kowalski ML, Mari A, Mullol J, Nazamova-Baranova L, O'Hehir RE, Ohta K, Panzner P, Passalacqua G, Ring J, Rogala B, Romano A, Ryan D, Schmid-Grendelmeier P, Todo-Bom A, Valenta R, Woehrl S, Yusuf OM, Zuberbier T, Demoly P. Global Allergy and Asthma European Network. Allergic Rhinitis and its Impact on Asthma. Practical guide to skin prick tests in allergy to aeroallergens. Allergy. 2012; 67:18–24.

18. Lund VJ, Kennedy DW. Quantification for staging sinusitis. The Staging and Therapy Group. Ann Otol Rhinol Laryngol Suppl. 1995; 167:17–21.
19. Jones PW. Quality of life measurement for patients with diseases of the airways. Thorax. 1991; 46:676–682.

20. Piccirillo JF, Merritt MG Jr, Richards ML. Psychometric and clinimetric validity of the 20-Item Sino-Nasal Outcome Test (SNOT-20). Otolaryngol Head Neck Surg. 2002; 126:41–47.

21. Fokkens WJ, Lund VJ, Mullol J, Bachert C, Alobid I, Baroody F, Cohen N, Cervin A, Douglas R, Gevaert P, Georgalas C, Goossens H, Harvey R, Hellings P, Hopkins C, Jones N, Joos G, Kalogjera L, Kern B, Kowalski M, Price D, Riechelmann H, Schlosser R, Senior B, Thomas M, Toskala E, Voegels R, Wang de Y, Wormald PJ. EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012. A summary for otorhinolaryngologists. Rhinology. 2012; 50:1–12.

22. Auerbach O, Stout AP, Hammond EC, Garfinkel L. Changes in bronchial epithelium in relation to cigarette smoking and in relation to lung cancer. N Engl J Med. 1961; 265:253–267.

23. Bascom R, Kesavanathan J, Fitzgerald TK, Cheng KH, Swift DL. Sidestream tobacco smoke exposure acutely alters human nasal mucociliary clearance. Environ Health Perspect. 1995; 103:1026–1030.

24. Nihlén U, Andersson M, Löfdahl CG, Persson CG, Montnémery P, Greiff L. Nasal neutrophil activity and mucinous secretory responsiveness in COPD. Clin Physiol Funct Imaging. 2003; 23:138–142.

25. Hurst JR, Wilkinson TM, Perera WR, Donaldson GC, Wedzicha JA. Relationships among bacteria, upper airway, lower airway, and systemic inflammation in COPD. Chest. 2005; 127:1219–1226.

26. Bergqvist J, Andersson A, Olin AC, Murgia N, Schiöler L, Bove M, Hellgren J. New evidence of increased risk of rhinitis in subjects with COPD: a longitudinal population study. Int J Chron Obstruct Pulmon Dis. 2016; 11:2617–2623.

27. Mir E, Shah A. Allergic bronchopulmonary aspergillosis in a patient with chronic obstructive pulmonary disease. Prim Care Respir J. 2012; 21:111–114.

28. Sin DD, Miravitlles M, Mannino DM, Soriano JB, Price D, Celli BR, Leung JM, Nakano Y, Park HY, Wark PA, Wechsler ME. What is asthma-COPD overlap syndrome? Towards a consensus definition from a round table discussion. Eur Respir J. 2016; 48:664–673.

29. Hens G, Vanaudenaerde BM, Bullens DM, Piessens M, Decramer M, Dupont LJ, Ceuppens JL, Hellings PW. Sinonasal pathology in nonallergic asthma and COPD: ‘united airway disease’ beyond the scope of allergy. Allergy. 2008; 63:261–267.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download