Abstract
Background
On 21st November 2016, Melbourne experienced an epidemic of ‘thunderstorm asthma.’ Although previously described in the literature, risk factors and natural history remain incompletely understood.
Objective
Our aim was to follow up those presenting to the 3 Emergency Departments (EDs) in our health service during the epidemic, and assess their history for previous asthma, rhinitis, and allergies.
Methods
ED notes of all respiratory presentations within 48 hours of the thunderstorm event were reviewed and patients with acute asthma included. A standardised questionnaire was devised encompassing asthma diagnosis, undiagnosed asthma symptoms and rhinitis severity. Patients were contacted by phone within 30 days of the event.
Results
Three hundred forty-four patients were identified overall; 263 patients were contactable and completed a phone or mail questionnaire. The mean age was 32.7 ± 19.2 years (range, 6 months–87 years; 25% < 18 years) with 58% male sex. A previous diagnosis of asthma was present in 42% (n = 111), and there was no previous asthma diagnosis in 58% (n = 152). Of those who had no asthma diagnosis 53% had probable undiagnosed asthma. Overall, rhinitis prevalence was 88%, of which 72% were moderate or severe (Allergic Rhinitis and its Impact on Asthma guidelines) and 51% (n = 133) reported a history of grass pollen allergy.
Epidemic thunderstorm asthma is the observed increase in acute bronchospasm cases following thunderstorms in the local vicinity [1]. First described in 1983 [2] with 26 asthma cases treated in Emergency Department (ED) in Birmingham (UK), thunderstorm asthma events have since been reported in Australia, Europe, North America, and the Middle East [1]. On 21st November 2016, Melbourne experienced the largest, most devastating epidemic of thunderstorm asthma with 2,332 ambulance calls, 3,365 excess respiratory related ED presentations and 9 possible related deaths to this thunderstorm event [3].
The literature suggests epidemic thunderstorm asthma occurs due to a complex interaction of patient and environmental factors. Patient factors include previous aeroallergen sensitization [4] and a previous history of allergic rhinitis [5]. Environmental factors include high concentrations of respirable aeroallergens in the atmosphere [6] and thunderstorm outflow tracts that produce downdrafts containing these aeroallergens [7].
Our study aimed to characterise the cohort of epidemic thunderstorm asthma patients who presented to the 3 EDs of Eastern Health, Melbourne's second largest metropolitan public health network servicing the eastern suburbs. In particular, we assessed for the prevalence of, prior and current asthma diagnosis, undiagnosed asthma symptoms, rhinitis and a history of previous allergy and eczema.
ED notes of all respiratory presentations to Eastern Health's 3 EDs over a 48-hour period from 1700 on the 21st November 2016 were reviewed. Documentation of acute asthma symptoms with exclusion of alternative diagnoses/triggers were included as epidemic thunderstorm asthma patients.
A questionnaire was developed to assess demographic data, previous history of asthma, rhinitis, allergies and eczema, smoking history, and the persistence/severity of symptoms 1 month after the thunderstorm event.
“Asthma ever” was defined as any previous diagnosis of asthma, with “current asthma” defined as those with symptoms within the last 12 months, and “past asthma” defined as most recent symptoms longer than 12 months ago. “Probable undiagnosed asthma” was defined as no previous diagnosis of asthma but reporting symptoms suggestive of asthma. Severity of rhinitis was classified according to Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines [8]. A history of allergies to food, grass, house dust mite, and animal was assessed.
Medical student volunteers trained with administering the telephone questionnaire contacted patients 1 month after the event under supervision by doctors from our Respiratory Department. All identified patients were contacted over a 2-week period with at least 3 attempts to contact patients via phone and those unable to be contacted were mailed a paper questionnaire. Those who declined consent, were uncontactable or did not respond to the mail questionnaire were excluded.
Data for all contacted patients was collated and analysed with descriptive statistical analysis performed on the whole cohort. Further subgroup analysis with Student t-test and chi-square test was performed to ascertain differences between those with asthma and those without. Approval was obtained from the Eastern Health Ethics and Research Committee for analysis of the results.
Three hundred forty-four patients met the inclusion criteria for epidemic thunderstorm asthma with a mean age of 31.60 ± 18.6 years and 58% (n = 199) were male sex. There were 263 (76%) completed questionnaires with 81 (24%) nonresponders. Of the nonresponders, 70 (87%) were uncontactable despite 3 phone calls and a mailout questionnaire, 7 (9%) declined participation and 4 (5%) presented other issues such as the need for an interpreter. There were no incomplete questionnaires that were excluded (Fig. 1).
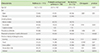
Of the 263 completed questionnaires the mean age was 32.7 ± 19.2 with 58% male sex (n = 153) (Table 1) which was comparable to the nonresponder group with a mean age of 28.1 ± 16.1 years and 57% male sex (n = 46).
Of the entire cohort, 42% (n = 111) had been diagnosed with asthma (“asthma ever”), comprising 29% (n = 75) with current asthma and 14% (n = 36) past asthma, but 58% (n = 152) did not have a previous diagnosis of asthma. However, 53% of these (n = 80) had probable undiagnosed asthma, reporting at least one symptom suggestive of asthma including wheeze (36%), chest tightness (29%) or shortness of breath (35%) with colds/hay fever/exercise or had been woken up from sleep by them (Fig. 2).
When comparing those with and without previous asthma diagnosis, the rates of rhinitis and grass pollen allergy were similar (Table 2). However, those with previously diagnosed asthma were older (36.7 ± 19.0 years vs. 29.7 ± 18.9 years, p = 0.004), more likely to have smoked (50% never smokers vs. 75% never smokers, p = 0.0001), have eczema (45% vs. 25%, p = 0.001) and a history of animal allergy (26% vs. 10%, p = 0.001) compared to those without asthma diagnosis (Table 2).
When comparing those with probable undiagnosed asthma to those with previous asthma, they were younger, less likely to smoke and have allergies (Table 3). Interestingly, patients with previous asthma diagnosis and probable undiagnosed asthma showed more persistent symptoms 4 weeks after the event.
The prevalence of rhinitis was 88% (n = 231) and of these, 78% (n = 177) experienced seasonal (Spring or Summer) symptoms, 13% (n = 30) perennial symptoms, and 9% (n = 24) reporting both. According to the ARIA classification, 18% (n = 41) had severe rhinitis, 54% (n = 125) moderate and 28% (n = 65) mild rhinitis.
Of patients assessed, 76% (n = 200) reported a history of at least one allergy (food/pollen/dust mites/animals) or eczema. The distribution of reported allergy history included grass pollens (51%) (n = 133), 20% (n = 53) food allergy, 30% (n = 78) house dust mite allergy, 17% (n = 44) animal allergy, and 33% (n = 87) with a history of eczema.
In this study of 263 respondents out of 344 patients presenting to ED with thunderstorm asthma, 58% had no asthma diagnosis. However, 53% of these had a history suggestive of probable undiagnosed asthma. Improved identification and treatment of these undiagnosed patients may further reduce the burden of thunderstorm asthma. Given that poor preventer adherence amongst those with diagnosed asthma is also a known risk factor for epidemic thunderstorm asthma [5], prescribing and improving adherence to inhaled steroids may help to reduce its impact. This is further illustrated by the observation that those with previous asthma and probable undiagnosed asthma had higher rates of persistent symptoms one month after the event than those with no asthma.
Overall, rhinitis prevalence was 88%, which is in keeping with the literature [59]. The majority had at least moderate rhinitis as per ARIA guidelines, and most had seasonal rhinitis affecting them in Spring or Summer. This suggests that having at least moderate rhinitis is a significant risk factor for epidemic thunderstorm asthma. A number of retrospective studies have found that treating allergic rhinitis is associated with reduction in healthcare utilisation for comorbid asthma. These include a risk reduction by half of an asthma-related event (hospitalisation and ED visit) for the treated group compared to the untreated group [10], and reduced risk for ED visits in patients with rhinitis who received intranasal corticosteroids [11]. As such, screening and educating rhinitis sufferers with regards to preventer intranasal corticosteroids in Spring months may reduce the impact of epidemic thunderstorm asthma.
In our cohort, allergy to grass pollen was the most commonly (51%) reported allergy. Grass pollen [45] and fungal spores [12] have been implicated as important aeroallergens in the pathogenesis of thunderstorm asthma [13]. Our data supports the key role of grass pollen allergy, but further assessment with either specific IgE testing or skin prick testing is required to confirm this.
In summary, our data highlights the importance of atopy and rhinitis as risk factors for epidemic thunderstorm asthma. A history of rhinitis should prompt clinicians to assess and treat rhinitis to reduce risk of epidemic thunderstorm asthma. Better identification of undiagnosed asthma and implementing treatment may also be important in reducing the burden of epidemic thunderstorm asthma.
Figures and Tables
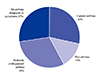 | Fig. 2Prevalence of asthma and probable undiagnosed asthma. Current asthma: previous diagnosis of asthma with symptoms in the last 12 months; Past asthma: previous diagnosis of asthma with no symptoms in the last 12 months; Probable undiagnosed asthma: no diagnosis of asthma, but symptoms to suggest asthma; No asthma: no diagnosis of asthma and no symptoms to suggest asthma. |
ACKNOWLEDGEMENTS
We acknowledge the following Medical students who assisted in data collection: Rowena Cao, Philip Chan, Robbie Chan, Kathryn Demase, Kai-Xing Goh, Nathan Hanegbi, Afnan Khaleque, Laura McDonald-Wedding, Julien Nithianandan, Natalie Saerian, Jenny Wang, Chloe Wong, Catherine Yu. All medical students affiliated with Eastern Health Clinical School, Monash University.
References
1. D’Amato G, Vitale C, D’Amato M, Cecchi L, Liccardi G, Molino A, Vatrella A, Sanduzzi A, Maesano C, Annesi-Maesano I. Thunderstorm-related asthma: what happens and why. Clin Exp Allergy. 2016; 46:390–396.

3. Review of response to the thunderstorm asthma event of 21–22 November 2016 Final Report [Internet]. Melbourne (Australia): State of Victoria, Inspector-General for Emergency Management, Department of Justice and Regulation;c2017. cited 2017 Jul 1. Available from: http://www.igem.vic.gov.au/home/reports+and+publications/reports/review+of+response+to+the+thunderstorm+asthma+event+of+november+2016+final+report.
4. Bellomo R, Gigliotti P, Treloar A, Holmes P, Suphioglu C, Singh MB, Knox B. Two consecutive thunderstorm associated epidemics of asthma in the city of Melbourne. The possible role of rye grass pollen. Med J Aust. 1992; 156:834–837.

5. Girgis ST, Marks GB, Downs SH, Kolbe A, Car GN, Paton R. Thunderstorm-associated asthma in an inland town in south-eastern Australia. Who is at risk. Eur Respir J. 2000; 16:3–8.

6. Suphioglu C, Singh MB, Taylor P, Bellomo R, Holmes P, Puy R, Knox RB. Mechanism of grass-pollen-induced asthma. Lancet. 1992; 339:569–572.

7. Marks GB, Colquhoun JR, Girgis ST, Koski MH, Treloar AB, Hansen P, Downs SH, Car NG. Thunderstorm outflows preceding epidemics of asthma during spring and summer. Thorax. 2001; 56:468–471.

8. Bousquet J, Khaltaev N, Cruz AA, Denburg J, Fokkens WJ, Togias A, Zuberbier T, Baena-Cagnani CE, Canonica GW, van Weel C, Agache I, Aït-Khaled N, Bachert C, Blaiss MS, Bonini S, Boulet LP, Bousquet PJ, Camargos P, Carlsen KH, Chen Y, Custovic A, Dahl R, Demoly P, Douagui H, Durham SR, van Wijk RG, Kalayci O, Kaliner MA, Kim YY, Kowalski ML, Kuna P, Le LT, Lemiere C, Li J, Lockey RF, Mavale-Manuel S, Meltzer EO, Mohammad Y, Mullol J, Naclerio R, O’Hehir RE, Ohta K, Ouedraogo S, Palkonen S, Papadopoulos N, Passalacqua G, Pawankar R, Popov TA, Rabe KF, Rosado-Pinto J, Scadding GK, Simons FE, Toskala E, Valovirta E, van Cauwenberge P, Wang DY, Wickman M, Yawn BP, Yorgancioglu A, Yusuf OM, Zar H, Annesi-Maesano I, Bateman ED, Ben Kheder A, Boakye DA, Bouchard J, Burney P, Busse WW, Chan-Yeung M, Chavannes NH, Chuchalin A, Dolen WK, Emuzyte R, Grouse L, Humbert M, Jackson C, Johnston SL, Keith PK, Kemp JP, Klossek JM, Larenas-Linnemann D, Lipworth B, Malo JL, Marshall GD, Naspitz C, Nekam K, Niggemann B, Nizankowska-Mogilnicka E, Okamoto Y, Orru MP, Potter P, Price D, Stoloff SW, Vandenplas O, Viegi G, Williams D;. LEN; AllerGen. Allergic Rhinitis and its Impact on Asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen). Allergy. 2008; 63:Suppl 86. 8–160.
9. Venables KM, Allitt U, Collier CG, Emberlin J, Greig JB, Hardaker PJ, Highham JH, Laing-Morton T, Maynard RL, Murray V, Strachan D, Tee RD. Thunderstorm-related asthma--the epidemic of 24/25 June 1994. Clin Exp Allergy. 1997; 27:725–736.
10. Crystal-Peters J, Neslusan C, Crown WH, Torres A. Treating allergic rhinitis in patients with comorbid asthma: the risk of asthma-related hospitalizations and emergency department visits. J Allergy Clin Immunol. 2002; 109:57–62.

11. Adams RJ, Fuhlbrigge AL, Finkelstein JA, Weiss ST. Intranasal steroids and the risk of emergency department visits for asthma. J Allergy Clin Immunol. 2002; 109:636–642.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download