Abstract
Background
Drug hypersensitivity is defined as any unfavorable reaction that occurs after the administration of any drug. It may or may not be mediated by the involvement of the immune system. Epidemiological data related to drug hypersensitivity reactions in our country are scarce.
Objective
To determine the prevalence of drug hypersensitivity in a group of young adults, as well as to identify associated factors.
Methods
A structured questionnaire was applied to young people aged 18 to 25 years. The instrument was oriented to identify reactions of drug hypersensitivity, as well as the most prevalent drugs involved. In addition, a personal and family history of atopic diseases was included. Analysis for associations between variables was been done through logistic regression.
Results
The prevalence of drug hypersensitivity reactions was 12% (144 of 1,200). The antibiotics were the agents most related to hypersensitivity reactions (9.8%) followed by nonsteroidal anti-inflammatory drugs (1.6%). Factors associated with drug hypersensitivity were a personal history of asthma, odds ratio (OR) 3.15 (95% confidence interval [CI], 1.44–6.91), maternal and paternal history of drug hypersensitivity, OR 2.33 (95% CI, 1.21–4.48) and OR 3.11 (95% CI, 1.22–7.92), respectively.
Drug hypersensitivity is defined as those unfavorable reactions that occur after the administration of any drug. It may or may not be mediated by the involvement of the immune system [1]. Determining its prevalence in the population represents a real challenge, since the majority of the research related to this problem, have been carried out in the hospital environment. Results from previous studies, obtained through questionnaires, show that drug hypersensitivity range from 5% to 25% of the population studied [234567].
Health problems related to the use of drugs are considered as a dynamic process, they depend on the treatment protocols, new products, as well as new pharmacological indications [8]. However, there are 2 groups of drugs that over the years appear to have not changed their prevalence, β-lactam antibiotics and nonsteroidal anti-inflammatory drugs (NSAIDs) [2567891011].
Factors causing drug hypersensitivity reactions have been classified depending on drug physicochemical characteristics, the treatment protocol and the patient itself [12]. Among patient characteristics are sex, age, comorbidities and history of drug reactions [256111314].
Data related to drug hypersensitivity in our country is scarce, and especially in population studies. Thus, the objective of this study was to determine the prevalence of drug hypersensitivity in Mexican young adults. In addition, to associate personal and family history of atopic diseases with drug hypersensitivity.
This study is a secondary analysis of a previous research [15]. A cross-sectional study, carried out between February and May 2014, analyzed a sample of 1,200 students from a public university (State of Mexico), aged 18 to 25. A nonprobabilistic sampling was performed.
A structured questionnaire was applied to investigate the personal and family history of allergic diseases: asthma, allergic rhinitis, urticaria, atopic dermatitis, and drug hypersensitivity [15].
The prevalence of drug hypersensitivity was calculated by dividing the affirmative response frequency by the total number of respondents. The odds ratio (OR) assessed the magnitude of the association between personal or family history of allergic disease with drug hypersensitivity. In all cases, 95% confidence intervals (CIs) were estimated. Risks were adjusted through binary logistic regression analysis. Values of p ≤ 0.05 were considered statistically significant. The data collected were analyzed with SPSS Statistics version 22.0 (IBM Co., Armonk, NY, USA).
The frequency of drug hypersensitivity was 144 of 1,200 with a prevalence of 12%. The prevalence in women was 13.4% and in men 10.0%, however, there was not statistically different (p = 0.068). Students in the Faculty of Chemistry had the highest prevalence, 15.4% (46 of 298); then Faculty of Dentistry, 11.9% (16 of 135) and Medicine, 11.8% (61 of 517). The lowest frequency was found in the Faculty of Engineering, 8.4% (21 of 250); however, no significant difference was observed among groups (p = 0.093).
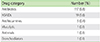
The mean age of subjects with drug hypersensitivity did not differ significantly from those without reactions (p = 0.240) (Table 1). Personal clinical history of asthma was more frequent in students with drug hypersensitivity (p = 0.001). In addition, maternal clinical history of atopic dermatitis (p = 0.018) and drug hypersensitivity (p = 0.001), as well as a paternal clinical history of drug hypersensitivity (p = 0.004), were significantly related to drug hypersensitivity in students.
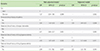
Antibiotics (9.8%), then NSAIDs (1.6%) and antihistamines (0.4%) were the most common category of drugs (Table 2). Penicillin was the most common antibiotic (6.3%), followed by sulfonamides (1.8%) and then cephalosporin (0.4%) (Table 3). Among the NSAIDs, acetylsalicylic acid (0.7%) was the most prevalent, followed by naproxen (0.5%) and metamizole (0.2%). Unexpectedly, among antihistamines, loratadine caused 0.4% of hypersensitivity reactions.
The multivariate analysis identified the personal clinical history of asthma (OR, 3.15; p = 0.004), and maternal or paternal clinical history of drug hypersensitivity (OR, 2.33; p = 0.011 and OR, 3.11; p = 0.018, respectively) as well as factors associated with drug hypersensitivity (Table 4).
Additionally univariate analyzes showed that personal clinical history of asthma was associated with hypersensitivity to antibiotics (OR, 2.69; 95% CI, 1.14–6.37; p = 0.024) and also did with NSAIDs (OR, 4.51; 95% CI, 0.99–20.41; p = 0.05). Among the antibiotics, the sulfonamides showed a significant association with the clinical history of asthma (OR, 9.13; 95% CI, 2.90–28.72; p = 0.0002). In contrast, among the NSAIDs
Ibuprofen was related to personal history of asthma (OR, 111.28; 95% CI, 4.44–2,785.75; p = 0.0004) but not acetylsalicylic acid (OR, 2.10; 95% CI, 0.12–37.17; p = 0.612).
In this study, the prevalence of drug hypersensitivity was 12% in university students. Thus, this is the first report of prevalence of drug hypersensitivity in our country in young adults. Mainly β-lactams and acetylsalicylic acid were the most prevalent drugs as the cause of hypersensitivity reactions. Factors associated with drug hypersensitivity were the personal clinical history of asthma and the paternal or maternal history of drug hypersensitivity.
At the global level, efforts to determine the prevalence of drug hypersensitivity in general population are scarce. Studies conducted in university students have shown that the problems associated with drug hypersensitivity are a common event. For example in Turkey, a group of medical students had a prevalence of drug hypersensitivity of 4.7% [2]. Recently in the United Arab Emirates, a group of students showed a drug hypersensitivity frequency of 7% [3]. Interestingly, our findings are quite similar to those reported for a population of university students in Brazil (12.1%) [4]. On the other hand, it was found that in an adult population of Portugal, the frequency was 7.8% [5], while in Turkey, the number of subjects who self-reported some type of drug reaction was 13.4% [6]. In Maputo, Africa 25% of a studied population reported drug hypersensitivity [7]. In hospitalized patients, the prevalence of drug hypersensitivity is higher than in the general population. For example, a survey study in patients who were to undergo surgery reported allergic drug reactions (up to more than 38%) [9]. In another study, performed in an Emergency Department, 13% of the patients declared to be allergic to some type of antibiotic [16].
Drugs that have been mostly related to hypersensitivity reactions are antibiotics or NSAIDs. In our study, students with drug hypersensitivity reported more than 80% reactions due to the use of antibiotics, mainly β-lactams and less than 15% were related to the use of NSAIDs. These findings are similar to previous reports [256791011]. However, there are also studies in which NSAIDs are most prevalently associated with hypersensitivity reactions [41718]. Perhaps for our country, the high prevalence of antibiotics compared with NSAIDs is a consequence of the lack of regulation in the sale of antibiotics that began until 2010 [19]. It allowed the general population to be overexposed to them (self-medication), thus in this way facilitated the process of sensitization.
In our study, the drugs that were most closely related to hypersensitivity reactions were penicillin, then sulfonamides and acetylsalicylic acid. This is consistent with the findings of previous studies [29]. Interestingly, there were 5 students who self-perceived as “allergic” to loratadine. Antihistamines are a group of medications widely used in the control of the symptoms of allergy and other diseases, however, few occasions produce hypersensitivity reactions. In Spain, a study reported five cases of urticaria associated with an antihistamine treatment [20]. It has also been reported a case of levocetirizine-induced fixed drug eruption [21], associated with piperazine derivatives and another one of urticaria by hydroxyzine and cetirizine [22]; also, anaphylactic reactions have also been documented [2324]. The questionnaire did not inquire about the symptoms caused by drugs, therefore it could be hard to tell drug allergy or hypersensitivity from other side effects, especially in cases of ambroxol, amantadine, or salbutamol which showed a low prevalence. In this study, no hypersensitivity events due to anesthetics, muscle relaxants or image contrast medium were reported.
Several factors associated with drug hypersensitivity have been described, some of which are related to drug itself, others with the treatment protocol and others with the participant [12]. In our study, we focused on factors related to the subjects and in their parental clinical history of drug hypersensitivity. This relationship has been documented previously; for example, Alergológica-2005, a multicenter study carried out in Spain, reported that patients with a family history of drug allergy were more likely to be allergic to some medication [11]. Similarly, Bavbek et al. [2] showed that the family history of drug hypersensitivity was associated with a higher probability of drug reactions in 2 self-reported studies, 1 with medical students and other studies in the open population [26]. Similar findings were observed in factory workers in Turkey [13] where the personal history of allergic disease was associated with drug hypersensitivity [261113]. In our study, we observed that family history of asthma showed this association.
It is suggested that genetic predisposition, sex, and age play an important role in the development of drug hypersensitivity [56111314]. In this study, the genetic predisposition was suspected through the parental clinical history of drug hypersensitivity. Our results show that sulfonamides were related to the personal clinical history of asthma, this type of association has rarely been reported, since the manifestations triggered by this group of drugs affect the skin [25]. A possible explanation would be that these students had a possible anaphylactic reaction as a manifestation of allergy to sulfonamides.
On the other hand, ibuprofen hypersensitivity was also associated with asthma. Traditionally acetylsalicylic acid, a COX-1 inhibitor, has been associated with this type of problem, producing aspirin-exacerbated respiratory disease. Ibuprofen inhibits COX-1 just like acetylsalicylic acid, thus producing bronchospasm [2627]. The association could be due to people uses ibuprofen more frequently than acetylsalicylic acid.
One of the main limitations of our study was that the diagnosis of drug hypersensitivity was through a self-reported questionnaire, which implies the possibility that the subject has misinterpreted some unrelated symptoms as part of drug allergy. Another limitation was the use of the term allergy instead of hypersensitivity to detect drug reactions. Finally, we did not specifically question the discomfort derived from drug hypersensitivity neither corroborated the diagnosis. Even so, this study provided an opportunity to estimate the size of reactions associated with drug use.
In conclusion, the perceived prevalence of drug hypersensitivity among university students is high. On the other hand, the personal clinical history of asthma and the parental clinical history of drug hypersensitivity are factors associated with drug hypersensitivity.
Figures and Tables
ACKNOWLEDGEMENTS
The authors gratefully acknowledge financial support from Universidad Autónoma del Estado de México (grant number: 3550/2013CTH).
References
1. Johansson SG, Bieber T, Dahl R, Friedmann PS, Lanier BQ, Lockey RF, Motala C, Ortega Martell JA, Platts-Mills TA, Ring J, Thien F, Van Cauwenberge P, Williams HC. Revised nomenclature for allergy for global use: Report of the Nomenclature Review Committee of the World Allergy Organization, October 2003. J Allergy Clin Immunol. 2004; 113:832–836.

2. Bavbek S, Erkekol FÖ, Celik GE, Gönüllü I, Misirligil Z. Self-reported prevalence of hypersensitivity reactions against drugs among medical students: does awareness cause any difference? Pharmacoepidemiol Drug Saf. 2011; 20:154–161.

3. John LJ, Ahmed S, Anjum F, Kebab M, Mohammed N, Darwich H, Ibraheem N, Arifulla M, Sreedharan J. Prevalence of allergies among university students: a study from Ajman, United Arab Emirates. ISRN Allergy. 2014; 2014:502052.

4. Ensina LF, Amigo MH, Koch T, Guzman E, Paoli R, Nunes IC. Drug hypersensitivity in students from São Paulo, Brazil. Clinics (Sao Paulo). 2010; 65:1009–1011.

5. Gomes E, Cardoso MF, Praça F, Gomes L, Mariño E, Demoly P. Self-reported drug allergy in a general adult Portuguese population. Clin Exp Allergy. 2004; 34:1597–1601.

6. Bavbek S, Çelik GE, Aydın Ö, Erkekol FÖ, Kurşun N, Mungan D, Mısırlıgil Z. Prevalence of hypersensitivity reactions against drugs among adult population in Turkey: a self-reported survey. J Public Health. 2012; 20:585–592.

7. Lunet N, Falcão H, Sousa M, Bay N, Barros H. Self-reported food and drug allergy in Maputo, Mozambique. Public Health. 2005; 119:587–589.

8. Doña I, Blanca-López N, Torres MJ, García-Campos J, García-Núñez I, Gómez F, Salas M, Rondón C, Canto MG, Blanca M. Drug hypersensitivity reactions: response patterns, drug involved, and temporal variations in a large series of patients. J Investig Allergol Clin Immunol. 2012; 22:363–371.
9. Velicković J, Palibrk I, Miljković B, Velicković D, Jovanović B, Bumbasirević V, Djukanović M, Sljukić V. Self-reported drug allergies in surgical population in Serbia. Acta Clin Croat. 2015; 54:492–499.
10. Makris MP, Sergentanis TN, Aggelides X, Tzanninis S, Polyzou E, Rigopoulos D, Psaltopoulou T. Cross sectional questionnaire-based internet study: Self-perception and clinical course of drug allergy in Greece. Allergol Int. 2017; 66:59–63.

11. Gamboa PM. The epidemiology of drug allergy-related consultations in Spanish Allergology services: Alergológica-2005. J Investig Allergol Clin Immunol. 2009; 19:Suppl 2. 45–50.
12. Thong BY, Tan TC. Epidemiology and risk factors for drug allergy. Br J Clin Pharmacol. 2011; 71:684–700.

13. Kurt E, Demir AU, Cadirci O. Immediate type drug hypersensitivity reactions and associated risk factors in an adult Turkish men population. Iran J Allergy Asthma Immunol. 2010; 9:245–250.
14. Demoly P, Bousquet J. Epidemiology of drug allergy. Curr Opin Allergy Clin Immunol. 2001; 1:305–310.

15. Puente-Fernández C, Maya-Hernández RL, Flores-Merino MV, Romero-Figueroa Mdel S, Bedolla-Barajas M, Domínguez García MV. Self-reported prevalence and risk factors associated with food hypersensitivity in Mexican young adults. Ann Allergy Asthma Immunol. 2016; 116:523–527.e3.

16. Wong J, Knott JC, Taylor DC, MacBean CE. Prevalence and validity of self-reported antibiotic allergy in Emergency Department patients. J Pharma Pract Res. 2008; 38:92–95.

17. Çelik GE, Karakaya G, Öztürk AB, Gelincik A, Abadoğlu O, Sin A, Damadoğlu E, Yılmaz İ, Demirtürk M, Dursun B, Özdemir SK, Çelikel S, Değirmenci P, Bozkurt B, Göksel Ö, Erkekol FÖ, Ayın Ö, Kavut AB, Kğrmaz C, Kalpaklğoğlu F, Büyüköztürk S, Kalyoncu F. Drug allergy in tertiary care in Turkey: results of a national survey. The ADAPT study: adult drug allergy perception in Turkey. Allergol Immunopathol (Madr). 2014; 42:573–579.

18. Jares EJ, Sánchez-Borges M, Cardona-Villa R, Ensina LF, Arias-Cruz A, Gómez M, Barayazarra S, Bernstein JA, Serrano CD, Cuello MN, Morfin-Maciel BM, De Falco A, Cherrez-Ojeda I. Latin America Drug Allergy Interest Group. Multinational experience with hypersensitivity drug reactions in Latin America. Ann Allergy Asthma Immunol. 2014; 113:282–289.

19. Diario Oficial de la Federación. Acuerdo por el que se determinan los lineamientos a los que estará sujeta la venta y dispensación de antibióticos (in Spanish) [Internet]. Ciudad de México (México): Diario Oficial de la Federación;2017. cited 2016 Dec 19. Available from: http://dof.gob.mx/nota_detalle.php?codigo=5144336&fecha=27/05/2010.
20. Rodríguez del Río P, González-Gutiérrez ML, Sánchez-López J, Nuñez-Acevedo B, Bartolomé Alvarez JM, Martínez-Cócera C. Urticaria caused by antihistamines: report of 5 cases. J Investig Allergol Clin Immunol. 2009; 19:317–320.
21. Kim MY, Jo EJ, Chang YS, Cho SH, Min KU, Kim SH. A case of levocetirizine-induced fixed drug eruption and cross-reaction with piperazine derivatives. Asia Pac Allergy. 2013; 3:281–284.

22. Chang YS, Kwon HS, Cho SH, Kim YY, Min KU. A case of urticaria induced by both hydroxyzine and cetirizine but not by levocetirizine. Allergy. 2007; 62:819–821.

23. Barranco P, López-Serrano MC, Moreno-Ancillo A. Anaphylactic reaction due to diphenhydramine. Allergy. 1998; 53:814.

24. Weidinger S, Mempel M, Ollert M, Elser I, Rakoski J, Köhn FM, Ring J. Anaphylaxis to mizolastine. J Allergy Clin Immunol. 2004; 114:979–981.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download