1. Kündig TM, Bachmann MF, DiPaolo C, Simard JJ, Battegay M, Lother H, Gessner A, Kühlcke K, Ohashi PS, Hengartner H, et al. Fibroblasts as efficient antigen-presenting cells in lymphoid organs. Science. 1995; 268:1343–1347. PMID:
7761853.

2. Zinkernagel RM, Ehl S, Aichele P, Oehen S, Kündig T, Hengartner H. Antigen localisation regulates immune responses in a dose- and time-dependent fashion: a geographical view of immune reactivity. Immunol Rev. 1997; 156:199–209. PMID:
9176709.

3. Zinkernagel RM. Localization dose and time of antigens determine immune reactivity. Semin Immunol. 2000; 12:163–171. PMID:
10910735.

4. Senti G, Johansen P, Kündig TM. Intralymphatic immunotherapy. Curr Opin Allergy Clin Immunol. 2009; 9:537–543. PMID:
19680119.

5. Senti G, Johansen P, Kündig TM. Intralymphatic immunotherapy: from the rationale to human applications. Curr Top Microbiol Immunol. 2011; 352:71–84. PMID:
21725898.

6. Senti G, Kündig TM. Intralymphatic immunotherapy. World Allergy Organ J. 2015; 8:9. PMID:
25780493.

7. Senti G, Kündig TM. Novel delivery routes for allergy immunotherapy: intralymphatic, epicutaneous, and intradermal. Immunol Allergy Clin North Am. 2016; 36:25–37. PMID:
26617225.
8. von Moos S, Kündig TM, Senti G. Novel administration routes for allergen-specific immunotherapy: a review of intralymphatic and epicutaneous allergen-specific immunotherapy. Immunol Allergy Clin North Am. 2011; 31:391–406. xiPMID:
21530827.

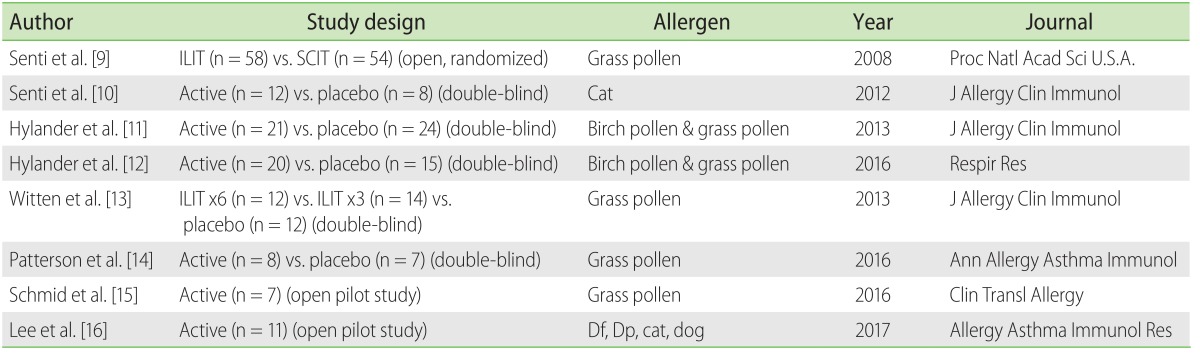
9. Senti G, Prinz Vavricka BM, Erdmann I, Diaz MI, Markus R, McCormack SJ, Simard JJ, Wüthrich B, Crameri R, Graf N, Johansen P, Kündig TM. Intralymphatic allergen administration renders specific immunotherapy faster and safer: a randomized controlled trial. Proc Natl Acad Sci U S A. 2008; 105:17908–17912. PMID:
19001265.

10. Senti G, Crameri R, Kuster D, Johansen P, Martinez-Gomez JM, Graf N, Steiner M, Hothorn LA, Grönlund H, Tivig C, Zaleska A, Soyer O, van Hage M, Akdis CA, Akdis M, Rose H, Kündig TM. Intralymphatic immunotherapy for cat allergy induces tolerance after only 3 injections. J Allergy Clin Immunol. 2012; 129:1290–1296. PMID:
22464647.

11. Hylander T, Latif L, Petersson-Westin U, Cardell LO. Intralymphatic allergen-specific immunotherapy: an effective and safe alternative treatment route for pollen-induced allergic rhinitis. J Allergy Clin Immunol. 2013; 131:412–420. PMID:
23374268.

12. Hylander T, Larsson O, Petersson-Westin U, Eriksson M, Kumlien Georén S, Winqvist O, Cardell LO. Intralymphatic immunotherapy of pollen-induced rhinoconjunctivitis: a double-blind placebo-controlled trial. Respir Res. 2016; 17:10. PMID:
26817454.

13. Witten M, Malling HJ, Blom L, Poulsen BC, Poulsen LK. Is intralymphatic immunotherapy ready for clinical use in patients with grass pollen allergy? J Allergy Clin Immunol. 2013; 132:1248–1252.e5. PMID:
24035151.

14. Patterson AM, Bonny AE, Shiels WE 2nd, Erwin EA. Three-injection intralymphatic immunotherapy in adolescents and young adults with grass pollen rhinoconjunctivitis. Ann Allergy Asthma Immunol. 2016; 116:168–170. PMID:
26706294.

15. Schmid JM, Nezam H, Madsen HH, Schmitz A, Hoffmann HJ. Intralymphatic immunotherapy induces allergen specific plasmablasts and increases tolerance to skin prick testing in a pilot study. Clin Transl Allergy. 2016; 6:19. PMID:
27231527.

16. Lee SP, Choi SJ, Joe E, Lee SM, Lee MW, Shim JW, Kim YJ, Kyung SY, Park JW, Jeong SH, Jung JH. A pilot study of intralymphatic immunotherapy for house dust mite, cat, and dog allergies. Allergy Asthma Immunol Res. 2017; 9:272–277. PMID:
28293934.

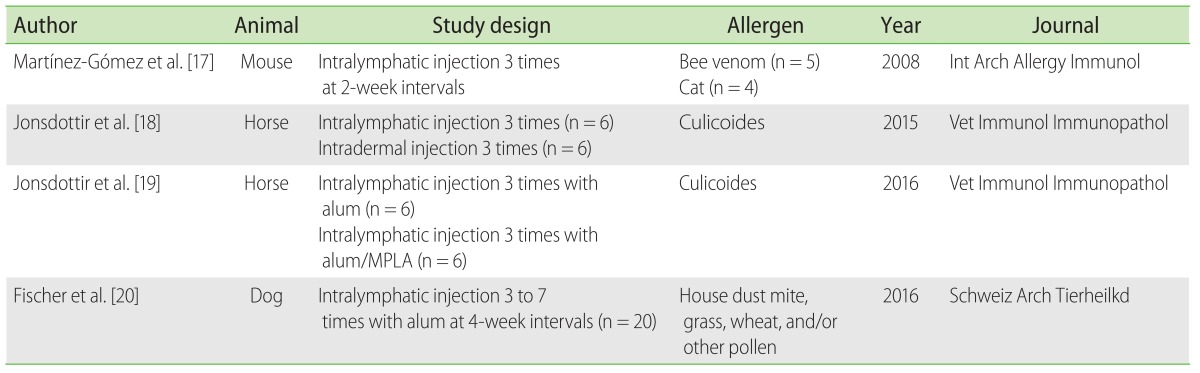
17. Martínez-Gómez JM, Johansen P, Erdmann I, Senti G, Crameri R, Kündig TM. Intralymphatic injections as a new administration route for allergen-specific immunotherapy. Int Arch Allergy Immunol. 2009; 150:59–65. PMID:
19339803.

18. Jonsdottir S, Hamza E, Janda J, Rhyner C, Meinke A, Marti E, Svansson V, Torsteinsdottir S. Developing a preventive immunization approach against insect bite hypersensitivity using recombinant allergens: a pilot study. Vet Immunol Immunopathol. 2015; 166:8–21. PMID:
26004943.

19. Jonsdottir S, Svansson V, Stefansdottir SB, Schüpbach G, Rhyner C, Marti E, Torsteinsdottir S. A preventive immunization approach against insect bite hypersensitivity: Intralymphatic injection with recombinant allergens in Alum or Alum and monophosphoryl lipid A. Vet Immunol Immunopathol. 2016; 172:14–20. PMID:
27032498.

20. Fischer N, Rostaher A, Favrot C. Intralymphatic immunotherapy: An effective and safe alternative route for canine atopic dermatitis. Schweiz Arch Tierheilkd. 2016; 158:646–652. PMID:
27655164.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download