Abstract
Background
Sericulture plays an eminent role in development of rural economy in India. Silk filature is a unit where silk is unwound from the cocoons and the strands are collected into skeins. During the process workers are exposed to the high molecular weight proteins like Sericin and Fibroin which are potent allergens leading to sensitization over a period of time and subsequently occupational related health disorders.
Objective
To identify and compare the magnitude of silk allergen sensitization in workers of silk filatures.
Methods
A community based comparative descriptive study was conducted for a period of 1 year at Ramanagara in south India. One hundred twenty subjects working in the silk filatures formed the study group. For comparison, 2 types of controls were selected viz.120 subjects who were not working in the silk filatures but resided in the same geographical area (control A) and 360 subjects who were not working in silk filatures as well not residing in the same geographical area (control B). Skin prick test was used to identify the silk allergen sensitization.
Results
Mean age was 34.14 ± 2.84 years in the study group. Mean age was 40.59 ± 14.40 years and 38.54 ± 12.20 years in control A and control B, respectively. There were 35 males (29.16%) and 85 females (70.84%) in the study group. There were 58 (48.34%) males and 62 (51.66%) females and 152 (42.2%) males and 208 females (57.8%) in control A and control B, respectively. Sensitization to silk allergen was 35.83% in the study group and 20.83% in the control group A and 11.11% in control group B. There was difference in the allergen sensitivity between the study group and control groups and it was statistically significant (chi-square = 38.08; p < 0.001).
Recent studies indicate that airborne insect allergens play an equally important role as pollens and fungi in the incidence and development of allergic diseases [1234]. The allergic respiratory reactions due to insects have been discussed for decades and among various insects, silkworm moth (Bombyx mori) has been identified as an important inhalant allergen in several studies worldwide [5678].
Silk filature is a unit where silk is unwound from the cocoons and the strands are collected into skeins. Various operations involved in the filatures include sorting of cocoons, boiling/cooking and reeling the filament. During the process workers are exposed to the high molecular weight proteins like Sericin and Fibroin which are potent allergens [9]. The workers can develop sensitization to silk allergen over a period of time leading to occupational related health disorders like Bronchial asthma, allergic rhinitis, conjunctivitis and dermatitis [1011].
Sericulture plays an eminent role in the development of rural economy in India. India happens to be the second largest producer of silk in the world producing an annual silk production of around 20,000 million tons. Karnataka contributes to 85% of total country's silk production [12]. Hence occupational related health hazards have significant impact on quality of life, productivity and economy. But they can be prevented by identifying at risk individuals and proper health education.
There are no studies on silk allergen sensitization in India after a study by Harindranath et al. [9] in 1985. In this regard, this study was undertaken to identify the silk allergen sensitization among workers of silk filature units in Ramanagara also known as Silk City of Karnataka, India.
A community based comparative descriptive study was conducted for a period of 1 year at Ramanagara in south India. Sample size was calculated based on prevalence of 16.9% [9] and with precision of 10% it was 56. With doubling effect, it was rounded off to 120. For the selection of study group, Silk filature units were randomly visited and owners were explained about the purpose of the study. All the workers willing to participate in the study and satisfying the inclusion and exclusion criteria were included in the study. Inclusion criteria were subjects working in silk filatures for period of minimum 6 months and individuals aged between 18–60 years of age. Exclusion criteria were those who were not willing to take part in the study; individuals with contraindications to skin prick test.
For comparison, 2 types of controls were selected. One hundred twenty subjects were selected among individuals who were not working in the silk filatures but resided in the same geographical area (control A). Another 360 subjects were selected among the individuals who were not working in silk filatures as well not residing in the same geographical area (control B). Control A was in the ratio of 1:1 and control B was in the ratio of 1:3. The study was conducted after the approval from the Institutional Ethics Committee. Informed consent was taken from all the subjects.
Skin prick test was used to identify the silk allergen sensitization. Commercial extracts of silk allergens were not readily available in India hence raw materials of pupae, cocoon, and sericin extract were obtained from Karnataka State Sericulture Research Development Institute and were sent to Creative Diagnostic Medicare Pvt Ltd, Navi Mumbai, India for preparation of allergen extracts for skin prick test. Three types of silk allergens viz. pupa, cocoon and sericin were used in the study. Skin prick test was performed on flexor aspect of the forearm after cleaning with the isopropyl alcohol.A single drop of allergen extract was placed along with positive control (histamine) and negative control (saline). Sterile lancet was used to prick by making ashallow lift (at an acute angle) for a second to allow adequate entry of antigen beneath the stratum corneum epidermis. Allergen was left in place for 20 minutes and then reading of wheal area diameter was taken with the help of a measuring scale. Results were interpreted according to Indian College of Allergy Asthma and Immunology guidelines. Grade 2+ and above were considered as positives [13].
Data was entered in the Microsoft Excel and analysed using SPSS ver. 16.0 (SPSS Inc., Chicago, IL, USA). Descriptive statistics like mean, standard deviation, proportions, and inferential statistics like chi-square test were used.
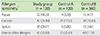
There were 35 males (29.16%) and 85 females (70.84%) in the study group. There were 58 males (48.34%) and 62 females (51.66%) and 152 males (42.2%) and 208 females (57.8%) in control A and control B, respectively. Mean age was 34.14 ± 2.84 years in the study group. Mean age was 40.59 ± 14.40 years and 38.54 ± 12.20 years in control A and control B, respectively. Majority of the subjects in both study and control groups A and B were the age group of 21–30 years (Table 1).
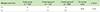
Sensitization to silk allergen was identified by skin prick test. It showed that 22 (18.33%) were sensitive to pupae, 42 (35%) were sensitive to cocoon and 35 (29.17%) were sensitive to sericin in the study group. It was observed that 4 (3.33%) were sensitive to pupae, 21 (17.50%) were sensitive to cocoon and 6 (5.00%) were sensitive to Sericin in the control group A and 15 (4.17%) were sensitive to pupae, 39 (10.83%) were sensitive to cocoon and 13 (3.61%) were sensitive to sericin in the control group B. Overall incidence of allergen sensitivity (sensitivity to one or other allergen) was 35.83% in the study group and 20.83 % in the control group A and 11.11% in control group B (Table 2). Comparison of allergen sensitivity between the study group and control groups were done. The difference was statistically significant (chi-square = 38.08; p < 0.001) (Table 3).
This present study revealed that sensitization to silk allergen among workers in silk filatures was 35.83%. Extensive review of literature showed that there was only one study conducted among silk workers in India by Harindranath et al. [9] in 1985. In their study, the skin prick test was performed using crude silkworm cocoon and pupa allergen extract. Results showed that 28.8% of the subjects were sensitive to silk allergen. Sericulture is also an important industry in China. In a community based cross sectional study conducted in China in 2001 by Celedon et al. [14] it was seen that 8.5% of asthmatics were sensitive to silk allergen. However the present study showed that sensitization to silk allergen was higher at 35.83%, which is more than that seen in both of the above studies.
It was observed that 20.83% of subjects living in the same geographical area but not working in the silk filatures were sensitive to silk allergen. The probable explanation for this is that the allergens released during the process become airborne and spread to the surrounding environment causing sensitization among people living in that environment. It is interesting to note that 11.11% of subjects living away from the geographical area of silk filatures also had sensitization.This skin test positivity may be due to cross reactivity with other insects like moth, butterfly [1516].
We thus conclude that there is high burden of silk allergen sensitivity among the workers of silk filature units in Ramanagara. It may lead to development of allergic disorders like asthma, urticaria, allergic rhinitis, allergic conjunctivitis, and others. Hence it is recommended that health education to be given regarding the signs and symptoms of allergic disorders to enable its early diagnosis and treatment and to prevent complications. Appropriate preventive measures to reduce/prevent exposure to silk allergen among silk industry workers are advised. Adoption of newer technology like Automated Reeling Machine which reduces the release of silk allergen into the environment and contact with human beings will greatly reduce the sensitization among the workers.
Figures and Tables
References
1. Bircher AJ. Systemic immediate allergic reactions to arthropod stings and bites. Dermatology. 2005; 210:119–127.

3. Sun BQ, Zheng PY, Zhang XW, Huang HM, Chen DH, Zeng GQ. Prevalence of allergen sensitization among patients with allergic diseases in Guangzhou, Southern China: a four-year observational study. Multidiscip Respir Med. 2014; 9:2.

4. Wu AY. Immunotherapy: vaccines for allergic diseases. J Thorac Dis. 2012; 4:198–202.
5. Perlman F. Insects as inhalant allergens; consideration of aerobiology, biochemistry, preparation of material, and clinical observations. J Allergy. 1958; 29:302–328.
6. Okuda M, Usami A, Itoh H, Ogino S. Nationwide investigation of insect allergy in patients with allergic rhinitis. Nihon Jibiinkoka Gakkai Kaiho. 2002; 105:1181–1188.

7. Larsson S, Backlund A. Regarding the putative identity of a moth (Thaumetopoea spp.) allergen. Allergy. 2009; 64:493.
8. Fedoskova TG, Petrova MA, Tsyvkina GI, Ivanov VD, Makovetskaia AK. Insect allergens in the human dwelling. Gig Sanit. 2005; (3):25–28.
9. Harindranath N, Prakash O, Subba Rao PV. Prevalence of occupational asthma in silk filatures. Ann Allergy. 1985; 55:511–515.
10. Zaoming W, Codina R, Fernandez-Caldas E, Lockey RF. Partial characterization of the silk allergens in mulberry silk extract. J Investig Allergol Clin Immunol. 1996; 6:237–241.
11. Fueki R, Kobayashi S. Some aspects of occupational asthma in Japan: peak flow diary and sericulture asthma. Allergy. 1988; 8:71–75.
12. Government of Karnataka Department of Sericulture [Internet]. Bangalore (IN): Government of Karnataka Department of Sericulture;cited 2014 Feb 23. Available from: http://www.karnataka.gov.in/sericulture.
13. Gaur SN, Singh BP, Singh AB, Vijayan VK, Agarwal MK. Guidelines for practice of allergen immunotherapy in India. Indian J Allergy Asthma Immunol. 2009; 23:1–21.
14. Celedon JC, Palmer LJ, Xu X, Wang B, Fang Z, Weiss ST. Sensitization to silk and childhood asthma in rural China. Pediatrics. 2001; 107:E80.
15. Johansson SG, Wuthrich B, Zortea-Caflisch C. Nightly asthma caused by allergens in silk-filled bed quilts: clinical and immunologic studies. J Allergy Clin Immunol. 1985; 75:452–459.

16. Wüthrich B, Dietschi R, Keter A, Zortea-Caflisch C. So-called "wild silk" asthma: an ever current inhalation allergy to silk waste. Schweiz Med Wochenschr. 1985; 115:1387–1393.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download