Abstract
Background
Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) are severe cutaneous adverse reactions (SCAR) with high mortality and have a significant public health impact because of high mortality and morbidity.
Objective
To describe data the epidemiological features, etiology, and treatment of retrospectively reviewed data of all patients with SJS and TEN.
Methods
Retrospective study was conducted in patients with SJS and TEN treated from January 1, 2009 to December 31, 2013 in Dr. Hasan Sadikin General Hospital Bandung, Indonesia.
Results
A total of 57 patients were enrolled in the study. Thirty-nine cases of SJS (21 males and 18 females), 7 cases of SJS overlapping TEN (4 males and 3 females), and 11 cases of TEN (5 males and 6 females) were reported. All cases of SJS and TEN were caused by drugs, such as paracetamol (16.56%), carbamazepine (7%), amoxicillin (5.73%), ibuprofen (4.46%), rifampicin (3.18%), and trihexyphenidyl (3.18%). All cases were treated systemically with corticosteroid alone (100%). Seven from 57 patients (12,28%) died; 5 cases developed sepsis and 2 cases developed respiratory failure. The mortality rate was 7.69% in SJS, 0% in SJS/TEN overlap, and 36.36% in TEN.
Severe cutaneous adverse reactions (SCAR) are one of the most common medical challenges presenting to an emergency room in any hospital. Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) are severe adverse drug reactions characterized by a low incidence but high mortality [12]. The incidence of SJS is approximately 5 cases per million people per year, and whereas TEN is approximately 2 cases per million people per year [2]. SJS and TEN are life-threatening SCAR, causing mortality in SJS is generally 5-10%, whereas TEN has a mortality rate of up to 30-40% [34]. SJS and TEN are classified as the same disease with different spectrums of severity according to the magnitude of epidermal detachment [1]. Several treatments have been reported to be beneficial but there are no clear indications for the optimal treatment [4567]. Systemic administration of corticosteroids is still controversial in many countries [8]. but this form of treatment has become the common treatment in Indonesia. The aim of this study was to present the current clinical characteristics and treatments of SJS and TEN in Indonesia.
This was a retrospective study of SJS and TEN in Dr. Hasan Sadikin General Hospital Bandung, Indonesia, between January 1, 2009 and December 31, 2013. Data of patients who diagnosed as SJS and TEN, were obtained from medical records, including demographic information (age, sex), relevant past medical history treatment, systemic corticosteroid treatment, and mortality.
Clinical symptoms for SJS should include acute conditions characterized by mucous membrane erosions and skin lesions (described as macules, atypical target-like lesions, bulla, or erosions), within in this spectrum of epidermal necrolysis, detachment of less than 10% of the total body surface area; when more than to 30% defines TEN; and while 10-30% are called SJS/TEN overlap.
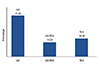
Thirty-nine cases of SJS, 7 cases of SJS overlapping TEN, and 11 cases of TEN were analysed in this study. There were 21 males and 18 females that meet criteria of SJS with range of 3 to 59 years old. The ages of patients with SJS overlapping TEN, comprising 4 males and 3 females were between 16 and 89 years old. Patients with TEN, comprising 5 males and 6 females, were between 9 and 49 years old (Fig. 1).
All subjects of SJS and TEN had received treatments and were suspected to be caused mainly by drugs, such as paracetamol (16.56%), carbamazepine (CBZ) (7%), amoxicillin (5.73%), ibuprofen (4.46%), rifampicin (3.18%), and trihexyphenidyl (3.18%) (Fig. 2). The other causes of the cases were not determined. Many other kinds of drugs were also presumed to be the causes of SJS and TEN, although the numbers of these causes were much lower than those mentioned above.
All cases were treated systemically with corticosteroid alone (100%). Fifty out of 57 cases (87.72%) were improved. The role of systemic corticosteroids in SJS and TEN is still controversial, but with a prompt and earlier treatment reduces morbidity and improves outcome of SJS and TEN patients [7]. Systemic corticosteroids (intravenous dexamethasone) equals to prednisone 1-4 mg/kg prednisone per day was given to SJS subjects, 3-4 mg/kg per day for SJS/TEN overlap, and 4-6 mg/kg per day for TEN (Table 1).
Our study demonstrated that length of hospitalization in patients with SJS and TEN varied. The mean cumulative length of hospitalization of subjects who survived were 8.06 days for SJS; 9.86 days for SJS/TEN overlap; and 6.1 days for TEN.
Sixteen cases of SJS, 1 case of SJS/TEN overlap, and 2 cases of TEN showed elevation of serum glutamic oxaloacetic transaminase (SGOT) and serum glutamic piruvic transaminase (SGPT). The SGOT and SGPT were elevated more than 35 IU/mL in females and more than 50 IU/mL in males (Fig. 3).
Respiratory disorders were shown in 2 cases of SJS. Four subjects with TEN and 1 subject with SJS developed sepsis. Sepsis was more frequent in TEN than in SJS.
SCAR are a major clinical problem [13]. Among numerous types of adverse drug hypersensitivity, SJS and TEN are the most serious and life-threatening adverse reactions [1]. SJS was first described in 1922 by two American physicians named Stevens and Johnson [29]. They described an acute mucocutaneous syndrome characterized by severe purulent conjunctivitis and severe stomatitis with extensive mucosal necrosis. It became known as Stevens-Johnson syndrome (SJS) [2]. TEN, also called Lyell's syndrome, was first described by the Scottish Dermatologist Alan Lyell in 1956 [29]. He reported four patients with an eruption resembling scalding of the skin objectively and subjectively which he called toxic epidermal necrolysis or TEN [2].
The exact pathogenesis was not clear until the recent studies, although Fas-Fas ligand (FasL) interaction was previously considered to be the main effector in triggering apoptosis of keratinocyte. Recent evidence suggested that granulysin, a cytotoxic protein produced by cytotoxic T lymphocytes and natural killer (NK) cells are the ones that actually "turn on" the extensive apoptosis in keratinocytes [1]. Involvement of cytotoxic T cells, tumor necrosis factor-alpha, and Fas-FasL interaction are considered to be relevant to these diseases [46]. A cytotoxic protein released from cytotoxic T cells or NK cells are a key mediator for disseminated keratinocyte death in SJS and TEN [13].
Optimal medical management of SJS and TEN require early diagnosis, immediate discontinuation of the causative drug(s), supportive care, and specific treatment [210]. There is no definitive specific treatment for SJS or TEN. Establishment of adequate and more effective treatment is needed [46].
To clarify the current manifestations and management of these diseases, we reviewed the clinical characteristics and treatments of patients with SJS and TEN that were reported from 2009 to 2013.
In our series, there were 57 cases of SJS and TEN over 5-year period. The ages of patients with SJS and TEN ranged from infants to elderly [46]. The ages were between approximately 20 to 29 years old in both diseases, which is as high as those reported from other countries. The most common drug implicated in our hospital was paracetamol (16.56%) and the other major causative drugs were CBZ (7%), amoxicillin (5.73%), ibuprofen (4.46%), rifampicin (3.18%), and trihexyphenidyl (3.18%). But in several Asian countries, CBZ has been reported as the most common culprit drug for SJS and TEN [346]. Strong association between HLA-B*1502 and CBZ-induced SJS and TEN has been reported in Han Chinese, Thai, Indian, and Malay patients [46].
The use of corticosteroids is based on the idea that corticosteroids can effectively suppress an excessive immune response [46]. Steroid also has been accepted as a treatment option because it suppresses the necrolytic process in the skin as well as internal organs [9]. However, its use is still controversial for many years [46101112]. In our study, corticosteroid was administered in all patients using intravenous dexamethasone.
Study conducted by Yamane et al. on 46 patients was concluded that early treatment with corticosteroid reduced morbidity and improved survival [412]. Tripathi et al. [13] have reported almost 99% recovery in patients of SJS treated with steroid. Literature search has also revealed that corticosteroid may show beneficial effect. TEN cases due to their antiapoptotic effect on keratinocytes [10]. On the other hand, steroid use has shown to decrease host resistance, prolong recovery, increases morbidity, mortality, and complications [1012].
Many patients of SJS and TEN showed liver involvement and other complications. Yamane et al. [4] reported that in both SJS and TEN, hepatitis was the most common complication. There 24 cases of SJS (46.2%) and 41 cases of TEN (63.1%) had liver involvement. The same result was reported in our study, that liver involvement was the most common complication. This study showed that SJS could cause more severe hepatitis (liver involvement) than TEN and sepsis was more frequent in TEN.
Five cases developed sepsis and 2 cases developed respiratory failure. All of these cases were treated with systemic corticosteroids. It can be presumed that control of the infections affects the outcome of treatment.
Cutaneous or allergic reactions account for approximately 14% of adverse drug reactions in hospital patients and 3% of all disabling injuries during hospitalization [11]. An earlier treatment with systemic corticosteroids could improve the disease outcome [81114]. Kim et al. [15] has reported 71 patients (85.4%) with SJS and TEN treated with dexamethasone shown good outcomes. Another study from Chantaphakul et al. [16] reported that 65% patients SJS and TEN gave beneficial effects of systemic corticosteroids.
Our review of the literature led us to conclude that systemic corticosteroid therapy is effective. Prompt and earlier treatment reduce mortality and improve outcome of SJS and TEN patients, although the selection of cases was biased because of our limitation to evaluate published cases.
Figures and Tables
 | Fig. 1Age of patients with SJS (A), SJS/TEN overlap (B), and TEN (C). SJS, Stevens-Johnson syndrome; TEN, toxic epidermal necrolysis. |
ACKNOWLEDGEMENTS
The author thank staff of Dermatology and Venereology, Dr. Hasan Sadikin Hospital Bandung, especially Hendra Gunawan, MD, PhD as the head of research division for the critical reading and editing and the other members for helpful assistance.
References
1. Chung WH, Hung SI. Genetic markers and danger signals in stevens-johnson syndrome and toxic epidermal necrolysis. Allergol Int. 2010; 59:325–332.

2. French LE. Toxic epidermal necrolysis and Stevens Johnson syndrome: our current understanding. Allergol Int. 2006; 55:9–16.

3. Valeyrie-Allanore L, Roujeau JC. Epidermal necrolysis (stevens-johnson syndrome and toxic epidermal necrolysis). In : Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell D, Wolff K, editors. Fitzpatrick's dermatology in general medicine. 8th ed. New York: McGraw Hill;2012. p. 439–448.
4. Yamane Y, Aihara M, Ikezawa Z. Analysis of Stevens-Johnson syndrome and toxic epidermal necrolysis in Japan from 2000 to 2006. Allergol Int. 2007; 56:419–425.

5. Guegan S, Bastuji-Garin S, Poszepczynska-Guigne E, Roujeau JC, Revuz J. Performance of the SCORTEN during the first five days of hospitalization to predict the prognosis of epidermal necrolysis. J Invest Dermatol. 2006; 126:272–276.
6. Verma R, Vasudevan B, Pragasam V. Severe cutaneous adverse drug reactions. Med J Armed Forces India. 2013; 69:375–383.

7. Wolkenstein PE, Roujeau JC, Revuz J. Drug-induced toxic epidermal necrolysis. Clin Dermatol. 1998; 16:399–408.

8. Roongpisuthipong W, Prompongsa S, Klangjareonchai T. Retrospective analysis of corticosteroid treatment in Stevens-Johnson syndrome and/or toxic epidermal necrolysis over a period of 10 years in Vajira Hospital, Navamindradhiraj University, Bangkok. Dermatol Res Pract. 2014; 2014:237821.

9. Harr T, French LE. Toxic epidermal necrolysis and Stevens-Johnson syndrome. Orphanet J Rare Dis. 2010; 5:39.

10. Azfar NA, Zia MA, Malik LM, Khan AR, Jahangir M. Role of systemic steroids in the outcome of Stevens-Johnson syndrome and toxic epidermal necrolysis. J Pak Assoc Dermatol. 2010; 20:158–162.
11. Martin T, Li H. Severe cutaneous adverse drug reactions: a review on epidemiology, etiology, clinical manifestation and pathogenesis. Chin Med J (Engl). 2008; 121:756–761.
12. Kardaun SH, Jonkman MF. Dexamethasone pulse therapy for Stevens-Johnson syndrome/toxic epidermal necrolysis. Acta Derm Venereol. 2007; 87:144–148.

13. Tripathi A, Ditto AM, Grammer LC, Greenberger PA, McGrath KG, Zeiss CR, Patterson R. Corticosteroid therapy in an additional 13 cases of Stevens-Johnson syndrome: a total series of 67 cases. Allergy Asthma Proc. 2000; 21:101–105.

14. Rijal A, Agrawal S. Outcome of Stevens Johnson syndrome and toxic epidermal necrolysis treated with corticosteroids. Indian J Dermatol Venereol Leprol. 2009; 75:613–614.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download