Abstract
Background
Objective
Methods
Results
Figures and Tables
Table 3
Scores of RQoLQ and TSS4 (n = 25)
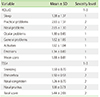
RQoLQ, rhinoconjunctivitis quality of life questionnaire; TSS, total symptom score; SD, standard deviation.
The score of each item of RQoLQ ranges from 0 (not troubled) to 6 (extremely troubled). The severity level of each dimension of RQoLQ is expressed as 1 to 3 (The levels were scores ranging between 0 and 2, between 2 and 4, between 4 and 6); The score of each symptom of TSS4 ranges from 0 to 3 (0, no symptoms; 1, mild symptoms [symptoms clearly present but minimal awareness, easily tolerated], 2, moderate symptoms [awareness of bothersome but tolerable symptoms], and 3, severe symptoms [symptoms hard to tolerate and/or causing interference with activities of daily living, sleeping or both]).
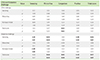
Table 4
Correlations of nasal responses to LTD4 and histamine nasal provocation and TSS4 with quality of life

LTD4, leukotriene D4; TSS, total symptom score; NAR, nasal airway resistance; VAS, visual analogue scale.
Significant correlations of both nasal symptom scores induced by LTD4 and histamine nasal provocation and the scores of TSS4 with the scores of quality of life questionnaire (RQoLQ) were shown in bold in the table.
Histamine nasal challenge induced sneezing and increase of nasal resistant were correlated with most of the dimensions (general, practical, nasal, eye problems, and quality of sleep), while LTD4 nasal challenge induced sneezing and increase of nasal resistant only correlated with nasal and ocular problems of RQoLQ; Symptom severity scores of TSS4 were significantly correlated with nasal and practical problems of RQoLQ.
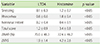
Table 5
Correlations of nasal responses to LTD4 and histamine nasal provocation with severity scores of TSS4
LTD4, leukotriene D4; TSS, total symptom score.
Significant correlations between nasal symptom scores induced by nasal provocation and the scores of TSS4 were shown in bold in the table. Only histamine nasal provocation induced nasal symptom scores were well correlated with nasal symptom severity scores assessed by TSS4.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download