Abstract
Background
Severe asthmatics are thought to have severer rhinitis than mild asthmatics. A pale nasal mucosa is a typical clinical finding in subjects with severe allergic rhinitis.
Objective
The aim of this study was to investigate whether a pale nasal mucosa affects airflow limitations in the upper and lower airways in asthmatic children.
Methods
Rhinomanometry, nasal scraping, and spirometry were performed in 54 asthmatic children (median age, 10 years). The nasal mucosa was evaluated by an otolaryngologist. Thirty-seven patients were treated with inhaled corticosteroids, and 11 patients were treated with intranasal corticosteroids.
Results
Subjects with a pale nasal mucosa (n = 23) exhibited a lower nasal airflow (p < 0.05) and a larger number of nasal eosinophils (p < 0.05) in the upper airway as well as lower pulmonary functional parameters (p < 0.05 for all comparisons), i.e., the forced vital capacity (FVC), the forced expiratory volume in 1 second, and the peak expiratory flow, compared with the subjects who exhibited a normal or pinkish mucosa (n = 31). No significant difference in the forced expiratory flow between 25%–75% of the FVC, regarded as indicating the peripheral airway, was observed between the 2 groups.
Conclusion
A pale nasal mucosa may be a predictor of eosinophil infiltration of the nasal mucosa and central airway limitations in asthmatic children. When allergists observe a pale nasal mucosa in asthmatic children, they should consider the possibility of airflow limitations in not only the upper airway, but also the lower airway.
Many studies have shown that rhinitis and asthma are commonly associated [1]. About 80% of patients with asthma also have allergic rhinitis [2], suggesting the concept of 'one airway, one disease'. The presence of allergic rhinitis commonly exacerbates asthma, increasing the risk of an asthma exacerbation and the frequency of emergency visits and hospitalizations for asthma. The basic principle is that these 2 conditions are manifestations of one syndrome in 2 areas of the respiratory tract: the more severe the rhinitis, the more severe the asthma [3].
The nasal and bronchial mucosae exhibit similarities. In asthma and rhinitis, inflammation of the nasal and bronchial mucosae is sustained by a similar inflammatory infiltrate that includes eosinophils, mast cells, T lymphocytes, cells of monocytic lineage [4], similar pro-inflammatory mediators (histamine, cysteinyl leukotrienes), Th2 cytokines, and chemokines [5]. Even in children with rhinitis, examination of the nasal mucosa is possible using an anterior rhinoscopy [6]. Typical allergic mucosa appears pale and swollen, while the mucosa is reddened in acute infections and after the overuse of topical medications, although these distinctions are not absolute [7]. If no allergen exposure has occurred, the nasal mucosa may be totally normal. However, chronic edema and a pale mucosa may occur in patients with perennial allergic rhinitis who have suffered from rhinitis for several years [8].
The main purpose of the present study was to investigate whether a pale nasal mucosa is correlated with airflow limitations in the upper and lower airways in asthmatic children.
Fifty-four children (32 boys, 22 girls; median age, 10.0 years) diagnosed as having asthma were recruited from the outpatient clinic of the Department of Pediatrics of the Fukuoka National Hospital. Bronchial asthma was diagnosed by pediatricians as episodes of dyspnea and wheezing according to the recommendations of the Global Initiative for Asthma guidelines [9]. All the subjects were clinically stable and their asthmatic conditions were considered to be well controlled. Children with a history of viral infections or asthma exacerbations during the month preceding the start of the trial were excluded. Measurements were made during midsummer and midwinter; both of these time periods are no-pollen seasons in Japan. Thirty-seven patients were receiving treatment that included inhaled corticosteroids (ICS). Forty-seven patients were diagnosed as having allergic rhinitis by an otolaryngologist. Eleven patients were being treated with intranasal corticosteroids. The atopic status was determined by measuring the serum IgE levels and the level of IgE specific for house-dust mites. The blood eosinophil percentage was measured; none of the patients were receiving systemic corticosteroids at the time of the study enrollment.
Parental consent was obtained for each child. The study was approved by the Fukuoka National Hospital Ethics Board.
The following nasal findings were described by an otolaryngologist, who was authorized as a specialist by the Oto-Rhino-Laryngological Society of Japan. The nasal observations were made by a single otolaryngologist who was unaware of the clinical findings. The otolaryngologist used a headlight (Clinica Headlight, Nagashima Medical Instruments Co., Tokyo, Japan) with a light source (SL-7, Nagashima Medical Instruments Co.) to observe the nasal findings, which included the color and presence of swelling of the inferior turbinates and the quantity of the nasal secretion. Each finding was evaluated using the following 4-point systems [10]: color of the inferior turbinates (0, normal; 1, pinkish; 2, red; 3, pale), swelling of the inferior turbinates (0, normal; 1, visible center of the middle turbinates; 2, partial visibility of the middle turbinates; 3, middle turbinates not visible), and quantity of nasal secretion (0, no secretion; 1, attachment of secretion; 2, semi-opaque secretion; 3, opaque secretion).
Nasal specimens were obtained by scraping the inferior turbinate with a cotton swab. The contents of the sample were spread over a glass slide, air-dried, fixed, and stained with a Giemsa stain (Muto Pure Chemicals, Co., Tokyo, Japan). The number of eosinophils on each slide was then counted using an optic microscope (Olympus BH-2; Olympus, Tokyo, Japan) for a mean of 10 optical fields at ×100 magnification; the results were then evaluated using the following 4-point system [1011]: 0. no eosinophils in any of the fields; 1, a few scattered eosinophils in some fields; 2, a moderate number of eosinophils and small clumps of eosinophils in some fields (i.e., between grades 1 and 3); and 3, large clumps of eosinophils in some fields. The slides were examined by a single investigator who was unaware of the clinical findings.
Nasal airflow was measured using active anterior rhinomanometry. To overcome the presence of mucus in the nose, patients were asked to blow their nose gently before each measurement of nasal resistance. Patients were asked to wear a tight-fitting facemask and, with their mouths closed, to breathe through one nostril. A sensor placed in the contralateral nostril recorded data on the prenasal and postnasal pressures via airflow and pressure transducers. The instrument (Chestgraph rhinomanometry HI-801, Chest Ltd., Tokyo, Japan) measured the transnasal airflow and pressure values used in a subsequent statistical analysis. Nasal airflow was reported as the sum of the recorded airflow through the right and left nostrils in milliliters per second at a pressure difference of 1.5 cmH2O across the nasal passage. Four or more airflow measurements were performed for each patient, and the mean was recorded when reproducible values were achieved.
Short-acting beta2-agonists were withheld for 8 hours prior to the test. Spirometric measurements were performed using a hot-wired spirometer (Chestgraph HI-801, Chest Ltd.). Forced expiratory maneuvers were repeated until two acceptable values of the forced expiratory volume in 1 second (FEV1) were obtained; the larger value was used for the analysis in accordance with the guidelines of the American Thoracic Society [12]. We recorded the values for FEV1, the forced vital capacity (FVC), the peak expiratory flow (PEF), and the forced expiratory flow between 25%–75% of the FVC (FEF25%–75%) as percentages of the predicted values for the Japanese population, as reported by Nishima et al. [13].
Patient age, height, nasal airflow, and pulmonary function were expressed as the median (interquartile range). The demographic characteristics, pulmonary function test parameters, nasal airflow, age, and height were compared using nonparametric tests (Mann-Whitney test or Kruskal-Wallis test). The use of inhaled and intranasal steroids and the grade of rhinitis were compared between groups using chi-square tests. The relationship between nasal airflow and pulmonary function was analyzed using the Spearman correlation test. A p-value of <0.05 was considered significant.
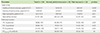
All 54 asthmatic children were tested. The subject characteristics and use of ICS and intranasal corticosteroids are shown in Table 1. Twenty-three asthmatic children had a pale nasal mucosa, whereas 10 subjects had a normal mucosa and 21 had a pinkish nasal mucosa. None of the patients had a red nasal mucosa. No significant differences in age, height, sex, use of ICS, intranasal corticosteroids, peripheral blood eosinophil count, serum IgE, or nonatopic cases were observed between the group with a normal, pinkish nasal mucosa and the group with a pale nasal mucosa.
Differences in the upper and lower airways between the normal, pinkish nasal mucosa group and the pale nasal mucosa group are shown in Table 2. In the upper airway, the pale nasal mucosa group had a severer grade of swelling of the inferior turbinates (p < 0.001), quantity and quality of nasal secretion (p <0.001, p < 0.05), and nasal eosinophils (p < 0.01) than the normal, pinkish nasal mucosa group. In addition, the pale nasal mucosa group had a lower nasal airflow than the normal, pinkish nasal mucosa group (p < 0.05). In the lower airway, the pale nasal mucosa group had a lower FVC (p < 0.05), FEV1 (p < 0.05), and PEF (p < 0.05; all the values were the percentages of the predicted values for the Japanese population) than the normal, pinkish nasal mucosa group. No significant difference in the FEF25%–75% (percentages of the predicted values for the Japanese population) was observed between the pale nasal mucosa group and the normal, pinkish nasal mucosa group.
This is the first study to report that a pale nasal mucosa is related to severe allergic rhinitis, nasal eosinophilic inflammation, and airflow limitations in the upper and lower airways of asthmatic children. Some reports have indicated that a nasal allergen challenge can induce bronchial inflammation [1415]. A pale nasal mucosa that exhibits inflammatory mucosal edema and vascular congestion with eosinophilic inflammation might suggest that airflow limitations of not only the upper airway, but also the lower airway should be considered in asthmatic children.
The pathogenesis of nasal obstruction is comprised of three components: inflammatory mucosal edema, vascular congestion, and mucus hypersecretion [16]. On the other hand, bronchial obstruction is sustained by smooth muscle spasms, inflammatory edema, and mucus hyperproduction [17]. Smooth muscle spasms are specific to the bronchus and do not occur in the nose. Ciprandi et al. [1819] mentioned that the number of eosinophils infiltrating the nasal mucosa was correlated with nasal airflow and the FEV1 and that nasal airflow was significantly correlated with FEV1 in steroid-naïve adults with perennial allergic rhinitis and asthma. A study comparing patients before and after treatment with nasal corticosteroids has indicated that nasal corticosteroids might reduce the number of admissions to Emergency Departments for asthma exacerbation and might improve respiratory symptoms and spirometry results [20]. Intranasal corticosteroids reportedly improved narrowing of the peripheral airway in children suffering from allergic rhinitis with abnormal lung function [21]. These findings constitute objective proof concerning the close link between nasal and bronchial functions in treated asthmatic children. In this study, asthmatic children with a pale nasal mucosa exhibited not only nasal eosinophilic inflammation and nasal airflow limitations, but also limitations of the lower airway. In other words, a pale nasal mucosa appears to be associated with nasal obstruction and inflammation through some pathophysiologic mechanisms, including oral respiration, the systemic absorption of mediators and cytokines, postnasal drip, and nervous reflex, thereby significantly affecting the central bronchial airflow in well-controlled asthmatic children.
Recently published guidelines for the diagnosis and management of rhinitis have presented assessments of nasal or non-nasal symptom severity and quality of life [22]. Nasal examinations were not mentioned. On the other hand, eosinophilic inflammation of the nose exists in asthmatics without nasal symptoms [23]. In a questionnaire for patients aged 1–4 years and 7 years, positive responses regarding the presence of nasal symptoms had a low specificity (62%) and a low agreement with a diagnosis of allergic rhinitis diagnosis (63%) [24]. In another report regarding the onset of allergic rhinitis in the young, 7.9% of the rhinitis cases were asymptomatic [25]. To assess the severity of allergic rhinitis, it might be useful to evaluate the grade of nasal examination [10], particularly in children. Joko et al. [26] reported that the nasal mucosa in patients with perennial allergic rhinitis showed a reduced red component of color when examined using a chromametric assessment: this means that the color of the nasal mucosa in patients with perennial allergic rhinitis is relatively pale. They reported that a change in the nasal mucosal color was related to an improvement in their subjective symptoms [27]. The color of the mucosa changed from pale to red when azelastin was administered in perennial allergic rhinitis patients [26]. In this study, a single otolaryngologist determined the nasal color in a blinded manner. The objective examination of nasal mucosa color has been established by the Oto-Rhino-Laryngological Society of Japan [10]. Further studies examining the manner of nasal examinations in asthmatic children by allergists may be needed.
In conclusion, this study provided consistent observations supporting the effect of allergic rhinitis, characterized by a pale nasal mucosa, on the upper and lower airways in asthmatic children treated with inhaled and/or intranasal corticosteroids. For allergists trained in performing nasal examinations, an examination of the nasal mucosa color in asthmatic children might indicate whether a narrowing of the lower airway should be suspected.
Figures and Tables
References
1. Bousquet J, Van Cauwenberge P, Khaltaev N. Aria Workshop Group. World Health Organization. Allergic rhinitis and its impact on asthma. J Allergy Clin Immunol. 2001; 108:5 Suppl. S147–S334.

2. Leynaert B, Bousquet J, Neukirch C, Liard R, Neukirch F. Perennial rhinitis: an independent risk factor for asthma in nonatopic subjects: results from the European Community Respiratory Health Survey. J Allergy Clin Immunol. 1999; 104(2 Pt 1):301–304.
3. Durham SR, Ying S, Varney VA, Jacobson MR, Sudderick RM, Mackay IS, Kay AB, Hamid QA. Cytokine messenger RNA expression for IL-3, IL-4, IL-5, and granulocyte/macrophage-colony-stimulating factor in the nasal mucosa after local allergen provocation: relationship to tissue eosinophilia. J Immunol. 1992; 148:2390–2394.
4. Bousquet J, Jeffery PK, Busse WW, Johnson M, Vignola AM. Asthma. From bronchoconstriction to airways inflammation and remodeling. Am J Respir Crit Care Med. 2000; 161:1720–1745.
5. Bousquet J, Khaltaev N, Cruz AA, Denburg J, Fokkens WJ, Togias A, Zuberbier T, Baena-Cagnani CE, Canonica GW, van Weel C, Agache I, Aït-Khaled N, Bachert C, Blaiss MS, Bonini S, Boulet LP, Bousquet PJ, Camargos P, Carlsen KH, Chen Y, Custovic A, Dahl R, Demoly P, Douagui H, Durham SR, van Wijk RG, Kalayci O, Kaliner MA, Kim YY, Kowalski ML, Kuna P, Le LT, Lemiere C, Li J, Lockey RF, Mavale-Manuel S, Meltzer EO, Mohammad Y, Mullol J, Naclerio R, O'Hehir RE, Ohta K, Ouedraogo S, Palkonen S, Papadopoulos N, Passalacqua G, Pawankar R, Popov TA, Rabe KF, Rosado-Pinto J, Scadding GK, Simons FE, Toskala E, Valovirta E, van Cauwenberge P, Wang DY, Wickman M, Yawn BP, Yorgancioglu A, Yusuf OM, Zar H, Annesi-Maesano I, Bateman ED, Ben Kheder A, Boakye DA, Bouchard J, Burney P, Busse WW, Chan-Yeung M, Chavannes NH, Chuchalin A, Dolen WK, Emuzyte R, Grouse L, Humbert M, Jackson C, Johnston SL, Keith PK, Kemp JP, Klossek JM, Larenas-Linnemann D, Lipworth B, Malo JL, Marshall GD, Naspitz C, Nekam K, Niggemann B, Nizankowska-Mogilnicka E, Okamoto Y, Orru MP, Potter P, Price D, Stoloff SW, Vandenplas O, Viegi G, Williams D. World Health Organization. GA(2)LEN. AllerGen. Allergic Rhinitis and its Impact on Asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen). Allergy. 2008; 63:suppl 86. 8–160.
6. Scadding GK, Durham SR, Mirakian R, Jones NS, Leech SC, Farooque S, Ryan D, Walker SM, Clark AT, Dixon TA, Jolles SR, Siddique N, Cullinan P, Howarth PH, Nasser SM. British Society for Allergy and Clinical Immunology. BSACI guidelines for the management of allergic and non-allergic rhinitis. Clin Exp Allergy. 2008; 38:19–42.

7. International Consensus Report on the diagnosis and management of rhinitis. International Rhinitis Management Working Group. Allergy. 1994; 49:19 Suppl. 1–34.
8. Dykewicz MS, Fineman S, Skoner DP, Nicklas R, Lee R, Blessing-Moore J, Li JT, Bernstein IL, Berger W, Spector S, Schuller D. Diagnosis and management of rhinitis: complete guidelines of the Joint Task Force on Practice Parameters in Allergy, Asthma and Immunology. American Academy of Allergy, Asthma, and Immunology. Ann Allergy Asthma Immunol. 1998; 81(5 Pt 2):478–518.
9. Definition, pathophysiology and pathogenesis of asthma, and natural history of asthma. Expert Panel Report 3: guidelines for the diagnosis and management of asthma. Full Report 2007. Bethesda (MD): U.S. Department of health and human services; National Heart, Lung, and Blood Institute;2007. p. 12–27.
10. Nasal allergy practice guidelines making Committee. Practical guideline for the management of allergic rhinitis in Japan. Tokyo: Life Science;2009.
11. Howarth PH, Persson CG, Meltzer EO, Jacobson MR, Durham SR, Silkoff PE. Objective monitoring of nasal airway inflammation in rhinitis. J Allergy Clin Immunol. 2005; 115:3 Suppl 1. S414–S441.

12. American Thoracic Society. Standardization of Spirometry, 1994 Update. Am J Respir Crit Care Med. 1995; 152:1107–1136.
13. Nishima S. Flow-volume curve in healthy and asthmatic children. Rinsho To Kenkyu. 1977; 54:185–190.
14. Bonay M, Neukirch C, Grandsaigne M, Leçon-Malas V, Ravaud P, Dehoux M, Aubier M. Changes in airway inflammation following nasal allergic challenge in patients with seasonal rhinitis. Allergy. 2006; 61:111–118.

15. Braunstahl GJ, Overbeek SE, Kleinjan A, Prins JB, Hoogsteden HC, Fokkens WJ. Nasal allergen provocation induces adhesion molecule expression and tissue eosinophilia in upper and lower airways. J Allergy Clin Immunol. 2001; 107:469–476.

18. Ciprandi G, Cirillo I, Vizzaccaro A, Milanese M, Tosca MA. Correlation of nasal inflammation and nasal airflow with forced expiratory volume in 1 second in patients with perennial allergic rhinitis and asthma. Ann Allergy Asthma Immunol. 2004; 93:575–580.

19. Ciprandi G, Vizzaccaro A, Cirillo I, Tosca M, Massolo A, Passalacqua G. Nasal eosinophils display the best correlation with symptoms, pulmonary function and inflammation in allergic rhinitis. Int Arch Allergy Immunol. 2005; 136:266–272.

20. Adams RJ, Fuhlbrigge AL, Finkelstein JA, Weiss ST. Intranasal steroids and the risk of emergency department visits for asthma. J Allergy Clin Immunol. 2002; 109:636–642.

21. Kessel A. The impact of intranasal corticosteroids on lung function in children with allergic rhinitis. Pediatr Pulmonol. 2014; 49:932–937.

22. Wallace DV, Dykewicz MS, Bernstein DI, Blessing-Moore J, Cox L, Khan DA, Lang DM, Nicklas RA, Oppenheimer J, Portnoy JM, Randolph CC, Schuller D, Spector SL, Tilles SA. Joint Task Force on Practice. American Academy of Allergy. Asthma & Immunology. American College of Allergy. Asthma and Immunology. Joint Council of Allergy, Asthma and Immunology. The diagnosis and management of rhinitis: an updated practice parameter. J Allergy Clin Immunol. 2008; 122:2 Suppl. S1–S84.

23. Gaga M, Lambrou P, Papageorgiou N, Koulouris NG, Kosmas E, Fragakis S, Sofios C, Rasidakis A, Jordanoglou J. Eosinophils are a feature of upper and lower airway pathology in non-atopic asthma, irrespective of the presence of rhinitis. Clin Exp Allergy. 2000; 30:663–669.

24. Kim H, Levin L, LeMasters GK, Villareal M, Evans S, Lockey JE, Khurana Hershey GK, Bernstein DI. Validating childhood symptoms with physician-diagnosed allergic rhinitis. Ann Allergy Asthma Immunol. 2012; 108:228–231.

25. Masuda S, Fujisawa T, Katsumata H, Atsuta J, Iguchi K. High prevalence and young onset of allergic rhinitis in children with bronchial asthma. Pediatr Allergy Immunol. 2008; 19:517–522.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download