Abstract
Background
Studies have reported that early febrile episodes and febrile episodes with infections are associated with a decreased risk of developing atopy.
Objective
To examine further the association between presence of and number of febrile episodes are with atopy and atopic diseases and if there was a difference between all fevers and fever after vaccination.
Methods
We studied 448 infants in a Singapore mother-offspring cohort study (Growing Up in Singapore Towards Healthy Outcomes) which had complete data for the exposures and outcomes of interest. Fever was defined as more than 38.0℃ and was self-reported. The presence of and number of febrile episodes were examined for association with outcome measures, namely parental reports of doctor-diagnosed asthma and eczema, and rhinitis, which was evaluated by doctors involved in the study at 18 and 36 months. These outcomes were considered atopic if there were 1 or more positive skin prick tests.
Results
The presence of all fevers from 0–6 months of age was associated with reduced odds of having atopy at 36 months of age (unadjusted odds ratio [OR], 0.628; 95% confidence interval [CI], 0.396–0.995). The presence of fever after vaccination from 0–24 months of age was associated with reduced odds of having atopy at 36 months of age (OR, 0.566; 95% CI, 0.350–0.915). The presence of all fevers from 0–6 months of age was associated with reduced odds of having atopic eczema at 36 months (OR, 0.430; 95% CI, 0.191–0.970). Fever was associated with increased odds of having doctor-diagnosed asthma and rhinitis.
There has been a rise in the global prevalence of asthma, allergic rhinitis and eczema [1]. The pathogenesis and risk factors for allergy are not completely understood. One of the factors being studied is the presence of fever in childhood. A study by Williams et al. [2] reported that each febrile episode in the first year was associated with reduced odds of allergic sensitization at age 6 to 7, and that each episode of fever between 7 and 12 months of age was associated with a lower unadjusted odds of allergic sensitization and asthma with allergic sensitization, with only the latter holding when adjusted for confounders [3]. von Mutius et al. [4] reported that the number of fever episodes was inversely related to the prevalence of atopy in asthmatic children, and found that the number of fever episodes and childhood infections was associated with the presence of asthma. Calvani et al. [5] reported similar findings, with fever episodes in the first 12 months of life having an inverse association with the risk of being atopic in asthmatics. Martinez et al. [6] suggested that nonatopic individuals were more capable of producing TH1-type memory cell cytokines than atopic individuals.
Another factor being studied is vaccination. Gruber [7] provided a commentary on how cohort and cross-sectional studies on vaccination have shown conflicting results on its association with atopic dermatitis, asthma and allergic rhinitis. It is possible that fever after vaccination is responsible for the inverse association with atopic disorders.
In light of the above, we aimed to further examine the association between fever, including fever after vaccinations, and the subsequent development of atopy (i.e., a positive skin prick test [SPT]), eczema, doctor-diagnosed asthma, and allergic rhinitis.
Growing Up in Singapore Towards Healthy Outcomes (GUSTO) is currently Singapore's largest birth cohort study [8]. A total of 1,152 participants were recruited.
For this study, there were 140 dropouts, 460 participants with missing clinical data, and 104 participants who did not complete the allergic assessment. A complete case analysis of 448 participants was done.
Fever was defined as more than 38.0℃. Parents were asked if their children developed fever and fever due to vaccination since the last GUSTO follow-up at 3, 6, 9, 12, 15, 18, and 24 months of age. The child was excluded from the study if parents did not know if the fever was more or less than 38.0℃. Fever and fever after vaccination were added together to give all fevers.
The data obtained was merged into presence of and number of febrile episodes of all fevers or fever after vaccination from 0–24, 0–6, 7–12, 13–18, and 19–24 months.
Atopy was defined as a positive SPT [9]. An SPT was performed at 18 and 36 months of age. The SPT was done on the volar aspect of the arm using antigen extracts of cow's milk, peanut, whole egg, and 3 dust mite species Dermatophagoides farinae, Dermatophagoides pteronyssinus, and Blomia tropicalis, along with saline and histamine for negative and positive controls (B. tropicalis: in-house laboratory; all other extracts and controls: Greer Laboratories, Lenoir, NC, USA). Measurement of wheal and flare was taken at 15 minutes after the test. An SPT result was considered positive when the wheal diameter was 3 mm greater than that elicited by the negative control.
At 18 and 36 months of age, participants were asked if their children had ever been diagnosed with eczema or asthma by a physician.
Allergic symptoms in a typical atopic individual (at least one SPT positive) can be referred to as atopy [9]. Therefore, we defined children with atopic eczema and atopic asthma as those who had ever been diagnosed with eczema and asthma by a doctor, and had at least 1 positive SPT.
Pearson chi-square and Fisher exact tests were used to examine differences in clinical characteristics between subjects included in the analysis and those who did not have a complete assessment of allergic disorders.
The relationship between the presence of all fevers and fever after vaccination in the first 2 years of life and outcome measures was evaluated with Pearson chi-square and Fisher exact tests. For the association between the number of febrile episodes in the first year of life and outcome measures, a linear logistic regression was used.
Potential confounders included in analyses were the child's sex, paternal and maternal history of allergy and asthma, maternal education, history of being breast-fed in the first 6 months of life, number of siblings, exposure to cigarette smoke in the first year of life, oral antibiotic use in the first year of life, birth weight, and gestational age. None of them were consistently associated with the exposure data (p > 0.2).
There were no differences in characteristics between the children who completed and did not complete the allergic assessments at 18 and 36 months of age. Characteristics evaluated included exposure and outcome data, and those expected to be confounders.
Sixty (13.4%) and 92 (20.5%) of the participants had at least 1 positive SPT by 18 and 36 months of age respectively. The presence of all fevers from 0–6 months of age was associated with reduced odds of having atopy at 36 months of age (unadjusted odds ratio [OR], 0.628; 95% confidence interval [CI], 0.396–0.995). The presence of fever after vaccination from 0–24 months of age was associated with reduced odds of having atopy at 36 months of age (OR, 0.566; 95% CI, 0.350–0.915; p < 0.05 for all).
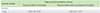
The number of participants who had eczema was 59 (13.2%) at 18 months of age and 73 (16.3%) at 36 months of age. Of this, 21 (4.7%) and 26 (5.8%) were atopic by 18 and 36 months of age respectively (Table 1).
The presence of all fevers from 0–6 months was associated with reduced odds of having eczema at 18 months (OR, 0.522;95% CI, 0.300–0.907) and atopic eczema at 36 months (OR, 0.430; 95% CI, 0.191–0.970). The number of febrile episodes from 0–6 months was associated with reduced odds of having non-atopic eczema at 18 months (OR, 0.657; 95% CI, 0.439–0.985). No association was seen for eczema and fever after vaccination.
Six (1.3%) and 18 (4.0%) of the participants had asthma by 18 and 36 months of age respectively. None were atopic at 18 months of age, but 5 (1.1%) were atopic at 36 months of age.
There were increased odds of having asthma (OR, 1.465; 95% CI, 1.122–1.913; p < 0.01) and nonatopic asthma (OR, 1.540; 95% CI, 1.149–2.064; p < 0.01) at 36 months with an increasing number of febrile episodes from 19–24 months. However, the number of febrile episodes from 0–24 months was associated with decreased odds of having asthma (OR, 0.141; 95% CI, 0.016–0.220; p < 0.05), and increased odds of having non-atopic asthma (OR, 1.161; 95% CI, 1.013–1.331; p < 0.01) at 36 months of age.
The presence of fever after vaccination from 19–24 months was associated with increased odds of having asthma (OR, 2.808; 95% CI, 1.018–7.747; p < 0.05) and nonatopic asthma (OR, 3.494; 95% CI, 1.109–11.010; p < 0.05) at 36 months of age. There was no association with atopic asthma.
Twenty-five (5.6%) and 51 (11.4%) of the participants had rhinitis by 18 and 36 months of age respectively, of which 8 (1.8%) and 15 (3.3%) were allergic by 18 and 36 months of age respectively.
The number of febrile episodes from 0–24 months of age was associated with increased odds of having rhinitis at 18 (OR, 1.119; 95% CI, 1.080–1.331; p < 0.01) and 36 (OR, 1.126; 95% CI, 1.037–1.224; p < 0.01) months of age, allergic rhinitis at 18 months of age (OR, 1.244; 95% CI, 1.066–1.452; p < 0.01) and nonallergic rhinitis at 18 (OR, 1.151; 95% CI, 1.017–1.302; p < 0.05) and 36 (OR, 1.117; 95% CI, 1.016–1.227; p < 0.05) months of age.
The presence of all fevers from 7–12 months was associated with increased odds of having rhinitis at 18 (OR, 5.750; 95% CI, 1.337–24.734; p < 0.01) and 36 (OR, 2.066; 95% CI, 1.003–4.252; p < 0.05) months of age, as well as nonallergic rhinitis 18 (OR, 7.862; 95% CI, 1.032–59.874, p < 0.05) and 36 (OR, 2.491; 95% CI, 1.013–6.128, p < 0.05) months of age. The presence of all fevers from 13–18 months was associated with increased odds of having rhinitis (OR, 2.301; 95% CI, 1.050–5.042, p < 0.05) and nonallergic rhinitis (OR, 2.491; 95% CI, 1.013–6.128, p < 0.05) at 36 months of age. The presence of all fevers from 19–24 months was associated with increased odds of having rhinitis (OR, 2.669; 95% CI, 1.330–5.353; p < 0.01) and nonallergic rhinitis (OR, 4.533; 95% CI, 1.728–1.893; p < 0.01) at 36 months of age.
The number of febrile episodes from 0–6 (OR, 1.356; 95% CI, 1.115–1.648; p < 0.05) and 7–12 (OR, 1.253; 95% CI, 1.032–1.522; p < 0.05) months was associated with increased odds of having rhinitis at 36 months of age. The number of febrile episodes from 13–18 months was associated with having rhinitis (OR, 1.475; 95% CI, 1.159–1.876; p < 0.01) and non-allergic rhinitis (OR, 1.370; 95% CI, 1.030–1.821; p < 0.05) at 36 months of age. The number of febrile episodes from 19–24 months was associated with increased odds of having nonallergic rhinitis at 36 months of age (OR, 1.330; 95% CI, 1.069–1.655; p < 0.05).
The presence of fever after vaccination from 19–24 months was associated increased odds of having nonallergic rhinitis at 36 months of age (OR, 2.581; 95% CI, 1.207–5.520; p < 0.05). The number of febrile episodes after vaccination from 19–24 months was associated with increased odds of having rhinitis (OR, 1.806; 95% CI, 1.119–2.913; p < 0.05) and nonallergic rhinitis (OR, 1.742; 95% CI, 1.044––2.907; p < 0.05) at 36 months of age.
Our study indicates decreased odds of having atopy and eczema after experiencing fever in the first 6 months of life. This is consistent with Williams et al. [2]'s study which demonstrated that fever was not associated with atopy alone, but that each febrile episode in the first year was associated with reduced odds of allergic sensitization.
Regarding asthma, our study findings were similar to the findings of von Mutius et al. [4], which showed that an increased number of febrile episodes was associated with an increased prevalence of asthma. von Mutius et al. [4] and Bonnelykke et al; [10] also demonstrated an association between the number of febrile episodes and the development of both nonatopic and atopic asthma later in life respectively. We hypothesize that the increased odds of having doctor-diagnosed asthma, especially nonatopic asthma, per febrile episode may be attributed to fever caused by lower respiratory tract infections. These infections are postulated to be triggers of wheezing symptoms.
The prevalence of asthma is 4% at 36 months of age in our study. As part of the International Study of Asthma and Allergies in Childhood studies, the prevalence of doctor-diagnosed asthma among a cohort of 6- to 7-year-old children in Singapore was found to be 18.5% in 1994 and 16.3% in 2001 [11]. Another Singaporean study reported a prevalence of 22.9% for cumulative presence of wheeze at 2 years of age [12]. However, there is a lack epidemiologic studies on prevalence of asthma and atopic asthma in Singapore for people of the same age group as our study, making comparisons inaccurate.
In this study, fever was associated with increased odds of having rhinitis and nonallergic rhinitis. This could be attributed to the high incidence of infectious rhinitis in childhood. The effect of fever on doctor-diagnosed asthma and rhinitis might in fact be a result of reverse causation, stemming from the nonallergic nature of early asthma and rhinitis, especially in young children.
With regards to allergic rhinitis, Tantilipikorn [13] suggested that while many recent studies show that early infections protect against allergy, certain viral infections, depending on the viral strain and the host, can exacerbate symptoms of airway allergy. This could explain the increased odds of having allergic rhinitis in our study.
The results suggested that fever after vaccination was had less associations with atopic diseases as compared to all fevers in general. A possible explanation would be that vaccinations provoke an immune response similar to a subclinical infection. The mechanisms of a vaccine-induced fever and how it affects the development of atopy might be different from that of fevers caused by other illnesses, given the discordant results between fever after vaccination and all fevers.
Also, results of the presence of fever were different from the number of febrile episodes with regards to the development of atopy and atopic diseases. Studies so far have only showed results of the effect of the number of febrile episodes [2345]. The presence of fever, as compared to repeated stimulation, might exert different effects on atopy via unknown mechanisms.
Regarding the timing of fever, Williams et al. [3] observed that in the first 2 years of life, febrile infections occurring at 7 to 12 months of age were most strongly associated with a reduction in the likelihood of both allergic sensitization and asthma with allergic sensitization at age 6 to 7 years. Their findings were concordant with those of Kramer et al. [14], who examined the relationship between the age of entry into daycare—a proxy for infectious exposure—and asthma and allergic outcomes at age 5 to 14 years, and found that entry to daycare between 6 and 11 months of age was associated with the lowest likelihood of SPT reactivity, asthma, hay fever, and positive specific IgE when compared with daycare entry at other time periods. We caution against specifying a certain time period on fever and early infections with the limited data available so far, as our findings showed varying time periods of significance for the development of atopy and atopic conditions, as well as varying results with fever in general versus fever after vaccination.
The study has several limitations. The response rate was low and only 448 out of 1,152 participants (38.9%) were included, which could contribute to responder bias. However, after statistical analysis, there were no significant differences between responders and nonresponders. Next, the case definitions relied on parental recall of diagnoses, instead of more objective measures of the disease. This may affect validity of the inclusion criteria. In the case of asthma, for example, the disease is difficult to distinguish from viral wheeze at times at 36 months of age, and lung function tests that secure the diagnosis cannot be performed yet at that age; yet doctors may make a clinical diagnosis of asthma. Also, recall bias may have been present as the data collected for fever and atopic symptoms relied on parental reports, but this was minimized as subjects were followed up within 3 months of the required reported event. During the data collection for fever after vaccination, the number of days between the vaccination and subsequent fever, and the presence of concurrent symptoms were not recorded. Therefore, a fever after vaccination might have in fact been due to an unrelated febrile illness.
The results suggest that there is an association between early fever and the presence of atopy and its associated conditions; however, we are unable to demonstrate cause and effect between the two. As such, despite the results showing a link between fever after vaccination and atopy and atopic disorders, it is not possible to establish in this study that fever after vaccination indeed confers a protective benefit against atopy.
In conclusion, the risk of having atopy and eczema at 36 months of life was reduced if fever of any type was present in the first 6 months of life. There was a positive association between fever in general and asthma and rhinitis; fever after vaccination had a similar result. However, this result may be attributed to the largely nonallergic, infectious nature of early asthma and rhinitis which inherently induce a fever, inadvertently producing a positive association. It is possible that fevers of different etiologies might have different effects on the development of atopic conditions.
Figures and Tables
ACKNOWLEDGEMENTS
We would like to thank the GUSTO study group and all clinical and home-visit staff involved. The voluntary participation of all participants is greatly appreciated.
The GUSTO study group includes Pratibha Agarwal, Arijit Biswas, Choon Looi Bong, Birit F.P. Broekman, Shirong Cai, Jerry Kok Yen Chan, Yiong Huak Chan, Cornelia Yin Ing Chee, Helen Chen, Yin Bun Cheung, Amutha Chinnadurai, Chai Kiat Chng, Mary Foong-Fong Chong, Yap-Seng Chong, Shang Chee Chong, Mei Chien Chua, Doris Fok, Marielle V. Fortier, Yam Thiam Daniel Goh, Joshua J. Gooley, Wee Meng Han, Mark Hanson, Christiani Jeyakumar Henry, Joanna D. Holbrook, Chin-Ying Hsu, Hazel Inskip, Jeevesh Kapur, Ivy Yee-Man Lau, Yung Seng Lee, Ngee Lek, Sok Bee Lim, Iliana Magiati, Lourdes Mary Daniel, Michael Meaney, Cheryl Ngo, Krishnamoorthy Niduvaje, Wei Wei Pang, Anqi Qiu, Boon Long Quah, Victor Samuel Rajadurai, Mary Rauff, Salome A. Rebello, Jenny L. Richmond, Anne Rifkin-Graboi, Allan Sheppard, Borys Shuter, Leher Singh, Shu-E Soh, Walter Stunkel, Lin Lin Su, Kok Hian Tan, Mya Thway Tint, Rob M. van Dam, Inez Bik Yun Wong, P. C. Wong, Fabian Yap, and George Seow Heong Yeo.
The GUSTO study is supported by the Singapore National Research Foundation under its Translational and Clinical Research (TCR) Flagship Programme, and administered by the Singapore Ministry of Health's National Medical Research Council (NMRC), Singapore- NMRC/TCR/004-NUS/2008; NMRC/TCR/012-NUHS/2014. Additional funding is provided by the Singapore Institute for Clinical Sciences, and the Agency for Science Technology and Research (A*STAR), Singapore. KMG is supported by the National Institute for Health Research through the NIHR Southampton Biomedical Research Centre and by the European Union's Seventh Framework Programme (FP7/2007-2013), projects EarlyNutrition and ODIN under grant agreement numbers 289346 and 613977.
References
1. Asher MI, Montefort S, Bjorkstén B, Lai CK, Strachan DP, Weiland SK, Williams H. ISAAC Phase Three Study Group. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Lancet. 2006; 368:733–743.

2. Williams LK, Peterson EL, Ownby DR, Johnson CC. The relationship between early fever and allergic sensitization at age 6 to 7 years. J Allergy Clin Immunol. 2004; 113:291–296.

3. Williams LK, Peterson EL, Pladevall M, Tunceli K, Ownby DR, Johnson CC. Timing and intensity of early fevers and the development of allergies and asthma. J Allergy Clin Immunol. 2005; 116:102–108.

4. von Mutius E, Illi S, Hirsch T, Leupold W, Keil U, Weiland SK. Frequency of infections and risk of asthma, atopy and airway hyperresponsiveness in children. Eur Respir J. 1999; 14:4–11.

5. Calvani M Jr, Alessandri C, Bonci E. Fever episodes in early life and the development of atopy in children with asthma. Eur Respir J. 2002; 20:391–396.

6. Martinez FD, Stern DA, Wright AL, Taussig LM, Halonen M. Association of non-wheezing lower respiratory tract illnesses in early life with persistently diminished serum IgE levels. Group Health Medical Associates. Thorax. 1995; 50:1067–1072.

7. Gruber C. Childhood immunisations and the development of atopic disease. Arch Dis Child. 2005; 90:553–555.

8. Soh SE, Lee SS, Hoon SW, Tan MY, Goh A, Lee BW, Shek LP, Teoh OH, Kwek K, Saw SM, Godfrey K, Chong YS, Gluckman P, van Bever HP. The methodology of the GUSTO cohort study: a novel approach in studying pediatric allergy. Asia Pac Allergy. 2012; 2:144–148.

9. Johansson SG, Bieber T, Dahl R, Friedmann PS, Lanier BQ, Lockey RF, Motala C, Ortega Martell JA, Platts-Mills TA, Ring J, Thien F, Van Cauwenberge P, Williams HC. Revised nomenclature for allergy for global use: Report of the Nomenclature Review Committee of the World Allergy Organization, October 2003. J Allergy Clin Immunol. 2004; 113:832–836.

10. Bonnelykke K, Vissing NH, Sevelsted A, Johnston SL, Bisgaard H. Association between respiratory infections in early life and later asthma is independent of virus type. J Allergy Clin Immunol. 2015; 136:81–86.e4.
11. Wang XS, Tan TN, Shek LP, Chng SY, Hia CP, Ong NB, Ma S, Lee BW, Goh DY. The prevalence of asthma and allergies in Singapore; data from two ISAAC surveys seven years apart. Arch Dis Child. 2004; 89:423–426.

12. Tan TN, Lim DL, Lee BW, Van Bever HP. Prevalence of allergy-related symptoms in Singaporean children in the second year of life. Pediatr Allergy Immunol. 2005; 16:151–156.

13. Tantilipikorn P. The relationship between allergic rhinitis and viral infections. Curr Opin Otolaryngol Head Neck Surg. 2014; 22:249–252.

14. Kramer U, Heinrich J, Wjst M, Wichmann HE. Age of entry to day nursery and allergy in later childhood. Lancet. 1999; 353:450–454.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download