Abstract
Background
Asthma and allergies are common and cause substantial burden in symptoms and suffering, hospitalizations and medication costs. However, despite the high prevalence, asthma burden has already decreased in Finland in 2000s.
Objective
We carried out an asthma barometer survey in all Finnish pharmacies to study changes in asthma severity and control, and use of health care services from 2001 to 2010.
Methods
Asthma severity, comorbid allergic conditions, and use of medication and health care services were assessed in subjects who purchased asthma or allergy medication from the pharmacies all across the country during one week in 2001 and again in 2010. In 2001, 3,062 patients (mean age, 49 years), and in 2010, 1,114 patients (mean age, 51 years) participated.
Results
In 2001 90% and in 2010 73% of the respondents reported physician-diagnosed asthma and were entitled to special reimbursement for their drug costs, i.e., they needed regular maintenance treatment. In 2001, 10% of the asthmatics regarded their disease as severe, compared with 4% in 2010, while the figures for mild asthma were 45% and 62%, respectively (p < 0.001). The proportion of patients needing emergency care during the last year decreased from 34% (2001) to 14% (2010) (p < 0.001) and the need for hospitalizations from 18% to 6% (p < 0.001). Smoking reduced from 24% to 18% among asthmatics ( p = 0.002). In 2010, risk factors for severe asthma were older age, comorbid atopic eczema, and food allergy.
The 10-year Finnish Asthma Programme 1994-2004 aimed to improve asthma management and reduce disease burden [1]. The Programme emphasized early diagnosis, effective anti-inflammatory treatment at the very onset of the disease and patient education for guided self-management. As the result, asthma related morbidity (e.g., disability pensions) and mortality decreased, as well as hospitalizations, despite the increase in total number of patients [2, 3]. The ongoing Finnish Allergy Programme 2008-2018 has taken further steps to reduce the burden of allergy and asthma [4].
During the last 10 years asthma medication and health care services have developed. To monitor and examine these changes, the Association of Finnish Pharmacies carried out so called asthma barometer surveys in 2001 and 2010 in all Finnish Pharmacies [5]. Special focus was laid on trends in self-reported symptom severity, use of asthma drugs and need for health care services among patients with physician diagnosed asthma.
Smoking is a major risk factor for asthma onset as well as for severe diseases, according to population-based and clinical studies [6, 7, 8]. Smoking has been on the decrease in the Finnish population, more in men [9]. However, over the last decade, changes in smoking have not been reported in Finnish asthmatics.
The study cohort consisted of 3,062 patients aged 1-92 years (mean, 49 years; 62% females) who obtained asthma medication from 612 Finnish pharmacies (77% of all the 796 pharmacies) across the country in June 2001. A total of 2,748 respondents (90%) reported physician-diagnosed asthma and 2,230 of them (73%) received special reimbursement for their regular asthma medication (Fig. 1). To be eligible for special asthma medication reimbursement, the diagnosis and long-term need for regular asthma medication (exceeding 6 months) must be confirmed by the patient's physician and the Social Insurance Institution of Finland according to agreed objective criteria (strict definition of asthma). Asthma is diagnosed using international guidelines to show reversible airway obstruction during peak expiratory flow recording, or by flow-volume spirometry and bronchodilator test, or by showing markedly increased bronchial responsiveness to histamine or metacholine [10].
A questionnaire was used to assess symptoms, asthma severity (mild, moderate or severe), use of medication and use of health care services over the past 12 months. Respondents from 2001 who were uncertain of the type of medication they were on (inhaled corticosteroids [ICS], short-acting β2-agonists [SABA], or some other kind of asthma medication, n = 521), were excluded.
The new study cohort consisted of 1,114 patients aged 5-75 years (mean, 51 years; 72% females) who obtained asthma or allergy medication from 382 Finnish pharmacies (47% of all 812 pharmacies) across the country. The numbers were smaller than in 2001 as the participants were the first consecutive 1-5 clients per pharmacy purchasing asthma or allergy medication during one week in September 2010. Physician-diagnosed asthma was reported by 816 subjects (73%), and 655 of them (80%) received special reimbursement for their regular asthma medication (Fig. 1).
To compare the 2010 results to the 2001 results, same questions were used to assess symptoms, asthma severity, use of medication, and health care services over the past 12 months. Comparisons of disease severity and use of asthma medication and health care services were restricted to respondents aged 5-75 years with strict definition of asthma.
Asthma severity was estimated using a score from 0 to 10: 0-1, no asthmatic symptoms; 2-5, mild symptoms not disturbing everyday life or sleep; 6-8, moderate symptoms disturbing daily activities and causing sleep disturbances; and 9-10, severe symptoms and hospitalizations. Waking up at night because of symptoms over the past 12 months was asked: never, twice a month, 3-4 times a month, 1-2 times a week, and almost every night. The use of ICS and SABA during the last 12 months was separately enquired with the options: no, occasionally, regularly, almost daily, and daily. The use of oral corticosteroids (OCS) was assessed with the options: no, short courses (a total of X courses over the last 12 months), and regular use. In 2010, 17 of the respondents did not answer the ICS question and three did not answer the question on SABA and were excluded.
Concerns with asthma drugs were assessed. Have you worried about: timely administering of medication, understanding inhaler instruction manual, inhalation technique, handling the inhaler, safety of long-term asthma medication, no problems, or some other concern?
The utilisation of health care services over the last 12 months was enquired. Have you had an appointment with a physician/nurse because of asthma: yes, how many times, or no? Have you been treated at a hospital emergency department because of asthma: yes, how many times, or no?
The study protocol was approved by the coordinating Ethics Committee of the Helsinki and Uusimaa Hospital District (HUS).
The data is presented as means with standard deviations or as counts with percentages. The 95% confidence intervals are given for the most important outcomes. Differences between groups were compared using the chi-square test, the Mann-Whitney test or the independent samples t-test. Factors associated with severe asthma were examined using univariate and multivariate logistic regression analyses, where age was treated as a continuous variable.
In 2001, of all the 3,062 respondents, 90% reported physician-diagnosed asthma. Other allergic conditions than asthma were not asked. Ten years later, in 2010, of all the 1,114 respondents, 816 (73%) reported physician-diagnosed asthma, 62% allergic rhinitis, 30% atopic eczema, 27% food allergies, 20% allergic conjunctivitis, and 11% a history of anaphylaxis. Those 655 subjects with strict definition of asthma reported comorbid allergic rhinitis in 55%, atopic eczema in 27%, food allergies in 27%, allergic conjunctivitis in 19%, and a history of anaphylaxis in 13% of the cases.
In 2001, asthma was estimated as mild by 45%, moderate by 45% and severe by 10% of the respondents, while the corresponding figures in 2010 were 62%, 34%, and 4%, respectively (Table 1, Fig. 2). Still, the percentage of asthmatics reporting night-time symptoms was at the same level or even higher in 2010 compared to 2001. Smoking decreased from 24% (2001) to 18% (2010).
Both the use of single ICS and SABA inhalers was markedly reduced in 2010 compared to 2001; daily or almost daily ICS from 87% to 48%, and almost daily SABA from 72% to 30%. The need for regular OCS remained at a low level (3% in 2001 and 2% in 2010). In 2001 the fixed combination inhalers of ICS and long acting β2-agonists (LABA) were just entering the market, and their use was not asked. In 2010, already 50% of the respondents used them daily or almost daily. However, already in 2001, 87% of the respondents had a regular inhaled ICS maintenance therapy (96% in 2010). Asthma medication was a major source of concerns as 24% of patients worried over drug safety in 2001, but in 2010 only 10% of patients had drug safety concerns (Table 2).
From 2001 to 2010, the proportion of patients needing emergency care during the last year decreased from 34% to 14% (p < 0.001) and the need for hospitalizations from 18% to 6% (p < 0.001) (Table 1, Fig. 2).
In children 5-17 year olds, the trends were the same as in adults: in 2010 compared to 2001 there were more mild asthmatics (85% and 78%, respectively) and less severe asthmatics (0% and 5%, respectively) (Table 1). However, more children reported night-time symptoms in 2010 compared to 2001 (76% vs. 45%, p < 0.02). Much less emergency visits were reported in 2010 compared to 2001 (4% vs. 38%, p < 0.001) as well as hospitalizations (4% vs. 16%).
Severe asthma and it's risk factors have been in focus during the recent Allergy Programme 2008-2018 [4]. To analyse the determinants for severe asthma in 2010, the relevant data was dichotomized to reflect severe (score 6-10, n = 243, 40%), or mild asthma (score 0-5, n = 365, 60%). The analyses were restricted to the respondents fulfilling the strict definition for asthma and aged >18 years (n = 476). In univariate analysis, older age (odds ratio [OR], 1.02), comorbid atopic eczema (OR, 1.76) and food allergies (OR, 1.84) were related to severe asthma (Table 3). Likewise, having received guided self-management instructions for allergic rhinitis (OR, 1.49), food allergies (OR, 2.36) or severe allergy (OR, 1.93) were associated with severe asthma. In multivariate analysis with forward selection, older age (OR, 1.02), atopic eczema (OR, 1.59) and having received food allergy guidance (OR, 2.49) were associated with severe asthma.
Self-reported asthma severity has decreased significantly in 10 years despite the slightly increased prevalence of the disease in Finland [11, 12]. Reductions in the use of emergency care and need for hospitalizations are in line with previous observations [2, 13], and are objective evidence of decreasing asthma burden. Occurrence of self-reported night-time symptoms did not change, however, which may mean more sensitive perception of even the mildest sleep disturbances. It should be noted that only a small group of asthmatics regards their disease as severe, in 2010 not more than 4% (32/813) and no one of those in the age group of 5-17 years. In the population, the majority has a mild disease relatively easy to control with appropriate medication.
In the asthma literature, severe asthma is overemphasized much because of the specialist care perspective. On the other hand patients with severe asthma should be in focus as they carry most of the disease burden including costs [2]. Allergic rhinitis and asthma have generally a favourable outcome [14]. Lindstrom et al. [15] used the Finnish military register to follow 393 asthmatic young men for 20 years. At the age of 40, 52% of them were free of symptoms or had them only occasionally, 20% had mild persistent, 17% moderate persistent, 10% severe persistent asthma, and 80% had comorbid allergic rhinitis.
During the 10-year observation period fixed ICS/LABA combination inhalers gained the market as 50% of patients with chronic diseases were using them in 2010. This explained the rapidly reduced use of single ICS and SABA inhalers. Nevertheless, already in 2001, 87% of patients were on regular ICS as the major increase took place in late 1990s [2]. Combination inhalers seem to have further improved the use of regular ICS in chronic asthma and thus maintained better asthma control [16].
Smoking is associated with mixed type or airway inflammation (eosinophilic and increasingly neutrophilic), more rapid lung function decline, reduced response to ICS treatment, increased disease severity and need for acute care, all resulting in worse asthma control [17, 18]. Furthermore, the so called overlap syndrome of asthma and chronic obstructive pulmonary disease is associated with poor quality of life [19]. However, the present survey did not find any clear association between smoking and self-reported severe asthma. The study cohorts were relatively young, around 50 years in both surveys, and the smokers probably did not yet suffer from the overlap syndrome with the more rapidly decreasing lung function. Older age, regardless of smoking, was a slight independent risk factor for severe asthma as have been reported also earlier [20].
Comorbid conditions were common in the 2010 asthma cohort. Of the respondents with the strict definition for asthma, 55% reported allergic rhinitis, 27% atopic eczema, 27% food allergies, 19% allergic conjunctivitis, and 13% a history of anaphylaxis. Allergic rhinitis in asthmatics has been reported to be a risk factor for more severe asthma [11]. This was not the case in the present cohort, but allergic rhinitis may have been underreported. Chronic atopic eczema is associated with increased bronchial responsiveness, and effective topical treatment may even decrease hyperreactivity [21, 22]. In our results, comorbid atopic eczema was associated with severe asthma (OR, 1.59). Having food allergies severe enough to require special guidance was also associated with severe asthma (OR, 2.49). Previously, comorbid food allergy (particularly against egg, peanut, soy, and wheat) has associated with hospitalizations due to asthma and increased need for corticosteroid medication [23]. Having received special guidance for self-management of anaphylaxis increased the risk of severe asthma, but only in the univariate analysis, probably because of small numbers (n = 84) compared to atopic eczema (n = 175) or food allergy (n = 178).
In 2010, 69% of asthma patients reported a scheduled visit to a physician and 23% to a nurse during the past year. Compared to 2001, appointments especially to nurses reduced, while worries about the inhalation technique increased, which may reflect less guidance on inhaled medication. Networking with asthma nurses was especially active during the Finnish Asthma Programme, but may have deteriorated since 4. However, worries about medication safety decreased markedly, which may indicate less fears against ICS therapy. That may have improved adherence to treatment.
Both samples were collected in pharmacies from patients purchasing asthma medication in 2001 and 2010, making the study samples comparable. The study time interval early summer in 2001 and autumn in 2010 which may have had an impact on those purchasing asthma medication. In May-June birch allergy season typically provokes symptoms whereas in September mugwort pollen, mold spores and common colds (schools and work places) may provoke asthmatic symptoms. We find it unlikely that the seasonal variation in the study samples would have a relevant impact on the study results. If anything, the September cohort was more in risk of asthma exacerbations.
Both the samples are representative for the whole country but the participation rate of pharmacies was higher in 2001 (77%) compared to 2010 (47%). In 2010 the relative shortage of pharmacists in the country reduced the local activities making the sample size smaller compared to 2001. The sample size was still large enough for comparison. The surveys were cross-sectional and provided comparison of point prevalences in 2001 and 2010, but do not give longitudinal information on an individual level. Since we were not able to produce participation rates of individual patients, we cannot totally exclude the possibility that the study sample would not be representative for all those purchasing asthma medication in the given time period. However, more severely ill patients are usually more willing to participate medical studies concerning their health and thus even if the participation rate would be less than 50% it would probably not have change the trends of our results. The age groups remained the same (5-75 years). In 2001, 257 respondents (13%) were under the age of 18 years compared to only 46 (7%) in 2010. The latter figure is too small to make conclusions of asthma severity. We excluded small children with intermittent wheezing associated with viral infections and to focus on persistent asthma.
In conclusion, our study results suggest that asthma might be becoming a milder disease in Finland and only a minority of asthmatics suffer from severe, uncontrolled asthma. The decline in the emergency visits and hospitalizations is in line with the self-reported change in severity. Health care services have essentially remained the same in Finland during the 10-year period. Reductions in hospitalizations, emergency care, and self-reported severity are all suggestive for better asthma control. Whether this is a result of earlier diagnosis and timely treatment or a change in the natural course of disease, cannot be answered. Older age and comorbid atopic eczema and food allergy were associated with more severe asthma. More attention should be paid to the comprehensive management of the atopic syndrome, where asthma, rhinoconjunctivitis, atopic eczema, and food allergy all play a role. Night-time symptoms and guidance of inhalation therapy need further attention [24].
Figures and Tables
 | Fig. 2Change of self-reported asthma severity, emergency care (visits) and hospitalizations (hospital days) in Finland 2001 and 2010. |
Table 1
Characteristics of patients with self-reported asthma entitled to special reimbursement for drug costs (strict criteria for asthma) in 2001 and 2010
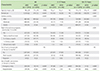
First comparison for all between 2001 and 2010 (age, 5-75 years) and then differentially for children and adolescents (5-17 years) between 2001 and 2010 and for adults (18-75 years) between 2001 and 2010.
Values are presented as number (%) unless otherwise indicated.
SD, standard deviation; NS, not significant.
*1,909 answers to the question of night time symptoms in 2001 and 645 answers in 2010. †1,899 answers to the question of oral corticosteroids in 2001 and 653 answers in 2010.
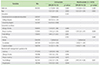
Table 2
Smoking habits, concerns on asthma treatment and use of health care services in the last 12 months in patients with self-reported asthma entitled to special reimbursement for drug costs (strict criteria for asthma) in 2001 and 2010 (age, 5-75 years)

ACKNOWLEDGEMENTS
This study is part of the follow-up of the Finnish Allergy Programme 2008-2018 supported by the Ministry of Social Affairs and Health.
References
1. Haahtela T, Laitinen LA. Asthma programme in Finland 1994-2004. Report of a Working Group. Clin Exp Allergy. 1996; 26:Suppl 1. i–ii. 1–24.
2. Haahtela T, Tuomisto LE, Pietinalho A, Klaukka T, Erhola M, Kaila M, Nieminen MM, Kontula E, Laitinen LA. A 10 year asthma programme in Finland: major change for the better. Thorax. 2006; 61:663–670.

3. Saynajakangas O, Valmari P, Tuuponen T, Keistinen T. Trends in hospitalization for childhood asthma in Finland in 1996-2004. Acta Paediatr. 2007; 96:919–923.
4. Haahtela T, von Hertzen L, Makela M, Hannuksela M. Allergy Programme Working Group. Finnish Allergy Programme 2008-2018: time to act and change the course. Allergy. 2008; 63:634–645.
5. Klaukka T, Hirvonen A, Peura S, Pakkila H. Asthma treatment in 2001, the essential results of the asthma barometer study. Finnish Med J. 2002; 57:292–294.
6. Plaschke PP, Janson C, Norrman E, Bjornsson E, Ellbjar S, Jarvholm B. Onset and remission of allergic rhinitis and asthma and the relationship with atopic sensitization and smoking. Am J Respir Crit Care Med. 2000; 162(3 Pt 1):920–924.

7. Siroux V, Pin I, Oryszczyn MP, Le Moual N, Kauffmann F. Relationships of active smoking to asthma and asthma severity in the EGEA study. Epidemiological study on the Genetics and Environment of Asthma. Eur Respir J. 2000; 15:470–477.
8. Lee JH, Haselkorn T, Borish L, Rasouliyan L, Chipps BE, Wenzel SE. Risk factors associated with persistent airflow limitation in severe or difficult-to-treat asthma: insights from the TENOR study. Chest. 2007; 132:1882–1889.
9. Laatikainen T, Critchley J, Vartiainen E, Salomaa V, Ketonen M, Capewell S. Explaining the decline in coronary heart disease mortality in Finland between 1982 and 1997. Am J Epidemiol. 2005; 162:764–773.

10. Bateman ED, Hurd SS, Barnes PJ, Bousquet J, Drazen JM, FitzGerald M, Gibson P, Ohta K, O'Byrne P, Pedersen SE, Pizzichini E, Sullivan SD, Wenzel SE, Zar HJ. Global strategy for asthma management and prevention: GINA executive summary. Eur Respir J. 2008; 31:143–178.

11. Pallasaho P, Juusela M, Lindqvist A, Sovijarvi A, Lundback B, Ronmark E. Allergic rhinoconjunctivitis doubles the risk for incident asthma--results from a population study in Helsinki, Finland. Respir Med. 2011; 105:1449–1456.
12. Browatzki A, Ulrik CS, Lange P. Prevalence and severity of self-reported asthma in young adults, 1976-2004. Eur Respir J. 2009; 34:1046–1051.

13. Kauppi P, Linna M, Martikainen J, Makela MJ, Haahtela T. Follow-up of the Finnish Asthma Programme 2000-2010: reduction of hospital burden needs risk group rethinking. Thorax. 2013; 68:292–293.

14. Teppo H, Revonta M, Haahtela T. Allergic rhinitis and asthma have generally good outcome and little effect on quality of life: a 20-year follow-up. Allergy. 2011; 66:1123–1125.
15. Lindstrom I, Suojalehto H, Pallasaho P, Luukkonen R, Karjalainen J, Lauerma A, Karjalainen A. Middle-aged men with asthma since youth: the impact of work on asthma. J Occup Environ Med. 2013; 55:917–923.
16. Bedouch P, Sadatsafavi M, Marra CA, FitzGerald JM, Lynd LD. Trends in asthma-related direct medical costs from 2002 to 2007 in British Columbia, Canada: a population based-cohort study. PLoS One. 2012; 7:e50949.

17. Osborne ML, Pedula KL, O'Hollaren M, Ettinger KM, Stibolt T, Buist AS, Vollmer WM. Assessing future need for acute care in adult asthmatics: the Profile of Asthma Risk Study: a prospective health maintenance organization-based study. Chest. 2007; 132:1151–1161.
19. Kauppi P, Kupiainen H, Lindqvist A, Tammilehto L, Kilpelainen M, Kinnula VL, Haahtela T, Laitinen T. Overlap syndrome of asthma and COPD predicts low quality of life. J Asthma. 2011; 48:279–285.

20. Tsai CL, Lee WY, Hanania NA, Camargo CA Jr. Age-related differences in clinical outcomes for acute asthma in the United States, 2006-2008. J Allergy Clin Immunol. 2012; 129:1252–1258.e1.

21. Mandelin JM, Remitz A, Virtanen HM, Malmberg LP, Haahtela T, Reitamo S. A 10-year open follow-up of eczema and respiratory symptoms in patients with atopic dermatitis treated with topical tacrolimus for the first 4 years. J Dermatolog Treat. 2010; 21:167–170.

22. Virtanen H, Remitz A, Malmberg P, Rytila P, Metso T, Haahtela T, Reitamo S. Topical tacrolimus in the treatment of atopic dermatitis: does it benefit the airways? A 4-year open follow-up. J Allergy Clin Immunol. 2007; 120:1464–1466.
23. Wang J, Visness CM, Sampson HA. Food allergen sensitization in inner-city children with asthma. J Allergy Clin Immunol. 2005; 115:1076–1080.

24. WHO Collaborating Center for Asthma and Rhinitis. Bousquet J, Anto JM, Demoly P, Schunemann HJ, Togias A, Akdis M, Auffray C, Bachert C, Bieber T, Bousquet PJ, Carlsen KH, Casale TB, Cruz AA, Keil T, Lodrup Carlsen KC, Maurer M, Ohta K, Papadopoulos NG, Roman Rodriguez M, Samolinski B, Agache I, Andrianarisoa A, Ang CS, Annesi-Maesano I, Ballester F, Baena-Cagnani CE, Basagana X, Bateman ED, Bel EH, Bedbrook A, Beghe B, Beji M, Ben Kheder A, Benet M, Bennoor KS, Bergmann KC, Berrissoul F, Bindslev Jensen C, Bleecker ER, Bonini S, Boner AL, Boulet LP, Brightling CE, Brozek JL, Bush A, Busse WW, Camargos PA, Canonica GW, Carr W, Cesario A, Chen YZ, Chiriac AM, Costa DJ, Cox L, Custovic A, Dahl R, Darsow U, Didi T, Dolen WK, Douagui H, Dubakiene R, El-Meziane A, Fonseca JA, Fokkens WJ, Fthenou E, Gamkrelidze A, Garcia-Aymerich J, Gerth van Wijk R, Gimeno-Santos E, Guerra S, Haahtela T, Haddad H, Hellings PW, Hellquist-Dahl B, Hohmann C, Howarth P, Hourihane JO, Humbert M, Jacquemin B, Just J, Kalayci O, Kaliner MA, Kauffmann F, Kerkhof M, Khayat G, Koffi N'Goran B, Kogevinas M, Koppelman GH, Kowalski ML, Kull I, Kuna P, Larenas D, Lavi I, Le LT, Lieberman P, Lipworth B, Mahboub B, Makela MJ, Martin F, Martinez FD, Marshall GD, Mazon A, Melen E, Meltzer EO, Mihaltan F, Mohammad Y, Mohammadi A, Momas I, Morais-Almeida M, Mullol J, Muraro A, Naclerio R, Nafti S, Namazova-Baranova L, Nawijn MC, Nyembue TD, Oddie S, O'Hehir RE, Okamoto Y, Orru MP, Ozdemir C, Ouedraogo GS, Palkonen S, Panzner P, Passalacqua G, Pawankar R, Pigearias B, Pin I, Pinart M, Pison C, Popov TA, Porta D, Postma DS, Price D, Rabe KF, Ratomaharo J, Reitamo S, Rezagui D, Ring J, Roberts R, Roca J, Rogala B, Romano A, Rosado-Pinto J, Ryan D, Sanchez-Borges M, Scadding GK, Sheikh A, Simons FE, Siroux V, Schmid-Grendelmeier PD, Smit HA, Sooronbaev T, Stein RT, Sterk PJ, Sunyer J, Terreehorst I, Toskala E, Tremblay Y, Valenta R, Valeyre D, Vandenplas O, van Weel C, Vassilaki M, Varraso R, Viegi G, Wang DY, Wickman M, Williams D, Wohrl S, Wright J, Yorgancioglu A, Yusuf OM, Zar HJ, Zernotti ME, Zidarn M, Zhong N, Zuberbier T. Severe chronic allergic (and related) diseases: a uniform approach--a MeDALL--GA2LEN--ARIA position paper. Int Arch Allergy Immunol. 2012; 158:216–231.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download