Abstract
Objective
The present study aimed to develop and validate the Korean version of the European Community Respiratory Health Survey (ECRHS) screening questionnaire for adult asthma surveys.
Methods
The ECRHS screening questionnaire was translated into Korean language according to the international criteria. Study participants were prospectively recruited from six referral hospitals and one health check-up center. Comprehensibility of the translation was tested in a pilot study of 10 patients. The reliability was evaluated by internal consistency and test-retest repeatability. Validity was assess with regard to physician-diagnosed asthma.
Results
A total of 100 adult asthma patients and 134 volunteers were recruited. Reliability was examined for 10 items in 100 asthmatics; Cronbach α coefficients were 0.84, and test-retest repeatability was good (Cohen κ coefficient, 0.71-1.00). Validity was assessed for 8 items in 234 participants; in particular, 'recent wheeze' showed a high sensitivity (0.89) for physician-diagnosed asthma. 'Recent asthma attack' and 'current asthma medication' showed high specificity (0.96-0.98).
Rapid increase in the prevalence of asthma has been the motivation for initiating global epidemiologic studies [1, 2]. The increase over a short period of time was too high to be explained by genetic factors alone, and thus was supposed to be related to nongenetic factors such as hygiene or environmental changes.
To investigate the epidemiology of asthma, two multinational study projects have been initiated in the early 1990s; the European Community Respiratory Health Survey (ECRHS) [1] and the International Study on Asthma and Allergy in Children (ISAAC) [2]. In particular, the ECRHS was the first study to investigate the prevalence of asthma and allergic diseases in adults, using the identical and standardized protocols [1]. The phase I ECRHS consisted of 140,000 young middle-aged adults recruited from 25 countries, and have provided several key information for adult asthma such as its geographical variation in prevalence, risk factors, or treatment status [3, 4]. The phase II survey was conducted as a nine-year follow-up prospective survey (2000-2002), and now the phase III survey is on the progress with particular aims for adult-specific risk factors or temporal changes in prevalence of adult asthma.
These continuum of asthma surveys reflect the significance and complexity of adult asthma. Adult-onset asthma was found to be more prevalent [5] and heterogeneous [6] than previously assumed. Despite great advances in knowledge during the past decades, the pathophysiology of asthma may have more to be discovered [6]. To understand the heterogeneous pathophysiology of asthma subtypes, epidemiologic investigation is warranted [7].
Standardized questionnaires are one of the most important instruments for asthma epidemiologic studies [8]. Precise definition of asthma requires full clinical examination [9], which is not always feasible in large-scale community population surveys. Therefore, it is a prerequisite to establish the standard questionnaire equipped with essential qualities such as reliability and validity [10]. At present, the ECRHS questionnaire is one of the most suitable instruments, as it has been well validated and accepted as the standard epidemiological tool [11, 12, 13, 14, 15, 16, 17, 18]. In addition, the ECRHS screening questionnaire consists of about 10 simples but specific questions for asthma, enabling large-scale surveys. However, to our knowledge, the questionnaire has not been validated for the use in Korea. In the present study, we aimed to develop the Korean translated version of the ECRHS screening questionnaire, and to assess the reliability and validity.
The present study consisted of 106 adult asthma patients and 128 nonasthmatic controls. The first sample set consisted of 100 asthma patients recruited from six referral centers in four different regions in Korea (Seoul, Seongnam, Daegu, and Busan), designed to examine the reliability of the questionnaire. The inclusion criteria were (1) adult asthma patients (age >18 years old), (2) diagnosed by a specialist physician within recent 12 months, (3) presence of any asthma symptoms within recent 12 months, (4) currently receiving asthma treatment, and (5) recent stability (no exacerbation during the last 1 month). Asthma patients were asked to visit twice by two weeks' intervals for test-retest reliability assessment.
In addition, volunteers were recruited to examine the validity of the questionnaire. They were recruited from the health check-up examinees at a check-up center, who underwent methacholine challenge tests (MCT). A total of 134 adults agreed to participate, and 128 subjects had no history of asthma and negative MCT. MCT was performed using five breath dosimeter methods using a modified protocol based on that of Chai et al. [19]
All the recruitment was carried out between January and October 2013. All the participants were fully informed of the study protocol, and were provided written, signed statements of informed consent. The study protocol was approved by the Institutional Review Board of Seoul National University Hospital, Seoul, Korea (IRB No. C-1212-069-451).
The ECRHS questionnaire is a self-administered questionnaire originally developed in English by Burney and Chinn [20]. First, the ECRHS screening questionnaire was translated into Korean language (Supplementary Tables 1, 2). In general, the translation process followed the methodology by Ferrer et al. [21]. Briefly, the first translation into Korean language was carried out by two bilingual professionals. They were asked to keep conceptual equivalence rather than linguistic uniformity. Then, the firstversion of the Korean translation was back-translated into English by two other bilingual professionals. The equivalence between original and translated versions was confirmed by 3 specialist physicians and 2 other bilingual persons. To check the comprehensibility and to validate cross-cultural adaptation, a pilot survey was performed using the Korean version questionnaire in 10 asthma patients. They were asked to response to each questionnaire item, and to report any difficulty in interpreting or answering the questions. Finally, we determined that the Korean translation process was valid.
Reliability was assessed by the responses from 100 asthma patients. Internal consistency was statistically assessed by Cronbach α coefficient [22]. To assess test-retest reliability, the same questionnaire was applied to the same patients with a two-week interval. Test-retest reliability was determined by Cohen κ coefficients [23], by measuring the agreement over two weeks' interval. In general, Cronbach α coefficients and Cohen κ coefficients are considered as good if ≥ 0.70 (excellent if ≥ 0.90) [24], and as excellent if ≥ 0.75 [15], respectively.
To test validity, the responses from 234 participants were analyzed. Validity of the questionnaire items was examined against 'physician-diagnosed asthma', which was determined by each specialist physician for the patient based on the history and MCT. As a marker for predictability, Youden index was calculated as (sensitivity + specificity - 1) [25].
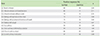
The baseline characteristics of study participants are presented in Table 1. As overall, the participants were middle-aged and had an average body mass index for Korean adults. None of them were illiterate. The self-administered questionnaire took about 5 minutes to complete the fill-up.
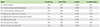
Reliability was examined among 100 adult asthma patients; the Cronbach α coefficients (for items Q1-Q6) were 0.84. Test-retest reliability was examined with about two weeks' interval, and Cohen κ coefficient was 0.71-1.00 (Table 2). Subitems such as 'Q1.1. Recent wheeze and breathlessness' and 'Q1.2. Recent wheeze without a cold' showed lower κ values than other items.
The validity of 8 questionnaire items was assessed with regard to 'physician-diagnosed asthma' among 234 participants (Table 3). Most of items showed high specificity (0.91-1.00), except for the item 'Q4. Waking with cough (specificity 0.82)'. Three items, 'Q1. Recent wheeze', 'Q5.4. Recent asthma attack', and 'Q6. Current asthma medication', showed better predictability for 'physician-diagnosed asthma
In the present study, the ECRHS screening questionnaire has been translated into Korean language. The translated version was comprehensible and reliable. The validity was assessed with regard to 'physician-diagnosed asthma'; in general, the questionnaire items had high specificity.
Originally, the ECRHS questionnaire was developed from the questionnaire of the International Union Against Tuberculosis and Lung Diseases (IUATLD) (1984) [11, 20]. The British Medical Research Council (BMRC) questionnaire was the first epidemiological method which was developed in 1960, but was not specific for asthma but rather general for chronic bronchitis, dyspnea, or wheeze [26]. The IUATLD (1984) was the advanced questionnaire in terms of asthma epidemiology, as it aimed to find the most valid combination of symptom items for identification of asthma, unlike the BMRC [11, 13]. In the process of the ECRHS, the first English version of the IUATLD has been adopted and subsequently translated into various languages. Now the multilanguage versions are available, including French, Dutch, German, Spanish, Norwegian, Turkish, Arabic, Japanese, Brazilian-Portuguese, or Mongolian [4, 14, 15, 16, 17, 18].
To date, several epidemiological surveys have been conducted in Korean adult populations [27, 28, 29, 30, 31]; however, these studies have utilized different definitions for asthma, such as 'recent wheeze' plus methacholine airway hyperresponsiveness (AHR), 'recent wheeze' plus 'ever asthma', or any of asthmatic symptoms plus AHR. Moreover, the definitions were adapted from the ISAAC questionnaire [2], or the American Thoracic Society and Division of Lung Diseases of the National Heart and Lung Institute (ATS-DLD-78) questionnaire [32]. Those questionnaires include the items similar to the ECRHS questionnaire; however, the ISAAC was originally made for childhood asthma, and the ATS-DLD-78 was later replaced by the ECRHS questionnaire [33]. Therefore, previous Korean studies had some limitations in comparing asthma prevalence with other countries.
In the present study, the Korean version showed similar diagnostic properties compared with other language versions [18]. 'Recent wheeze' showed a high sensitivity (0.89), but had a lower specificity than 'recent asthma attack' did (0.91 vs. 0.98). Thus, in cases of requiring a highly specific definition, it may be necessary to combine the symptom with methacholine AHR [34, 35].
Meanwhile, the questionnaire items containing the word 'asthma' (such as 'recent asthma attack' and 'current asthma medication') showed high specificity (0.96-0.98). There is concern that the use of term 'asthma' in the questionnaire might increase the risk of misclassification, as the 'asthma diagnosis' depends on regional quality of medical specialty care [12, 33]. However, it may be less controversial to use 'asthma' term in the survey questionnaire, particularly in developed countries. In Korea, sociomedical recognition of asthma has been recently improved and the guidelines are being further implemented to clinical practice [36, 37, 38]. In this regard, these 'asthma' items might be considered as the alternative to the MCT-combined definition for its high specificity in large-scale population surveys wherein MCT is not feasible.
In the literature, asthma has no gold standard definition for epidemiological studies [33, 39]. Methacholine AHR is not synonymous to asthma, and the MCT has potential biases in conducting or interpreting the results [40]. As shown above, each questionnaire item has weaknesses. Moreover, it is concerned whether asthma is simply definable by dichotomous questionnaire assessment [41]. Therefore, it is necessary to understand the pros and cons of each definition and properly select for the intended use, as 'the validity of an instrument depends not only on its agreement with the gold standard, but also on its intended use' as stated by Pekkanen and Pearce [42].
The present study has limitations as following. The study participants were recruited from medical institutions, and consisted of approximately 1:1 ratio of asthma patients and nonasthmatic controls. Particularly, asthmatics were recruited from referral hospitals. Therefore, the sensitivity may have been over-estimated by the participants' characteristics of disease activity [43]. Methodologically, reliability testing may be fully carried out in clinical samples, but the validity may be ideally better evaluable in the intended study populations such as general populations. Nevertheless, the present study had strengths that the participants' asthma were well-characterized by physicians, minimizing the bias of misclassification of the subjects. In addition, the Korean translated version was comprehensible and reliable. Therefore, it can be applied in further surveys for comparing the prevalence of asthma between countries.
In conclusions, the present study demonstrated that the Korean version of the ECRHS screening questionnaire was comprehensible, reliable and valid. We suggest the Korean-translated ECRHS questionnaire to be utilized in further epidemiological studies for asthma in Korean adult population.
Figures and Tables
ACKNOWLEDGEMENTS
This study was supported by a grant of Korea Healthcare technology R&D project, Ministry of Health & Welfare, Republic of Korea (A092076). The authors thank Dr. Deborah Jarvis (Imperial College, London, UK) for allowing us to use the questionnaire.
References
1. Burney PG, Luczynska C, Chinn S, Jarvis D. The European Community Respiratory Health Survey. Eur Respir J. 1994; 7:954–960.

2. Asher MI, Keil U, Anderson HR, Beasley R, Crane J, Martinez F, Mitchell EA, Pearce N, Sibbald B, Stewart AW, Strachan D, Weiland SK, Williams HC. International Study of Asthma and Allergies in Childhood (ISAAC): rationale and methods. Eur Respir J. 1995; 8:483–491.

3. Janson C, Anto J, Burney P, Chinn S, de Marco R, Heinrich J, Jarvis D, Kuenzli N, Leynaert B, Luczynska C, Neukirch F, Svanes C, Sunyer J, Wjst M. European Community Respiratory Health Survey II. The European Community Respiratory Health Survey: what are the main results so far? European Community Respiratory Health Survey II. Eur Respir J. 2001; 18:598–611.
4. Variations in the prevalence of respiratory symptoms, self-reported asthma attacks, and use of asthma medication in the European Community Respiratory Health Survey (ECRHS). Eur Respir J. 1996; 9:687–695.
5. de Nijs SB, Venekamp LN, Bel EH. Adult-onset asthma: is it really different? Eur Respir Rev. 2013; 22:44–52.

6. Wenzel SE. Asthma phenotypes: the evolution from clinical to molecular approaches. Nat Med. 2012; 18:716–725.

7. Lotvall J, Akdis CA, Bacharier LB, Bjermer L, Casale TB, Custovic A, Lemanske RF Jr, Wardlaw AJ, Wenzel SE, Greenberger PA. Asthma endotypes: a new approach to classification of disease entities within the asthma syndrome. J Allergy Clin Immunol. 2011; 127:355–360.
8. Song WJ, Kang MG, Chang YS, Cho SH. Epidemiology of adult asthma in Asia: toward a better understanding. Asia Pac Allergy. 2014; 4:75–85.

9. Pearce N, Beasley R, Burgess C, Crane J. Asthma epidemiology: principles and methods. New York: Oxford University Press;1999.
10. Samet JM. A historical and epidemiologic perspective on respiratory symptoms questionnaires. Am J Epidemiol. 1978; 108:435–446.
11. Burney PG, Laitinen LA, Perdrizet S, Huckauf H, Tattersfield AE, Chinn S, Poisson N, Heeren A, Britton JR, Jones T. Validity and repeatability of the IUATLD (1984) Bronchial Symptoms Questionnaire: an international comparison. Eur Respir J. 1989; 2:940–945.
12. Sunyer J, Basagana X, Burney P, Anto JM. International assessment of the internal consistency of respiratory symptoms. European Community Respiratory Health Study (ECRHS). Am J Respir Crit Care Med. 2000; 162(3 Pt 1):930–935.
13. Burney PG, Chinn S, Britton JR, Tattersfield AE, Papacosta AO. What symptoms predict the bronchial response to histamine? Evaluation in a community survey of the bronchial symptoms questionnaire (1984) of the International Union Against Tuberculosis and Lung Disease. Int J Epidemiol. 1989; 18:165–173.

14. Mahboub BH, Al-Hammadi S, Rafique M, Sulaiman N, Pawankar R, Al Redha AI, Mehta AC. Population prevalence of asthma and its determinants based on European Community Respiratory Health Survey in the United Arab Emirates. BMC Pulm Med. 2012; 12:4.

15. Ribeiro M, Angelini L, Robles-Ribeiro PG, Stelmach R, Santos Ude P, Terra-Filho M. Validation of the Brazilian-Portuguese version of the European Community Respiratory Health Survey in asthma patients. J Asthma. 2007; 44:371–375.

16. Sakar A, Yorgancioglu A, Dinc G, Yuksel H, Celik P, Dagyildizi L, Coskun E, Kaya E, Ozyurt B, Ozcan C. The prevalence of asthma and allergic symptoms in Manisa, Turkey (A western city from a country bridging Asia and Europe). Asian Pac J Allergy Immunol. 2006; 24:17–25.
17. Sonomjamts M, Dashdemberel S, Logii N, Nakae K, Chigusa Y, Ohhira S, Ito C, Sagara H, Makino S. Prevalence of asthma and allergic rhinitis among adult population in Ulaanbaatar, Mongolia. Asia Pac Allergy. 2014; 4:25–31.

18. Watanabe J, Taniguchi M, Takahashi K, Nakagawa T, Ooya Y, Akazawa A, Akiyama K. Validation of ECRHS Questionnaire in Japanese to use for nation-wide prevalence study of adult asthma. Arerugi. 2006; 55:1421–1428.
19. Chai H, Farr RS, Froehlich LA, Mathison DA, McLean JA, Rosenthal RR, Sheffer AL, Spector SL, Townley RG. Standardization of bronchial inhalation challenge procedures. J Allergy Clin Immunol. 1975; 56:323–327.

20. Burney P, Chinn S. Developing a new questionnaire for measuring the prevalence and distribution of asthma. Chest. 1987; 91:6 Suppl. 79S–83S.

21. Ferrer M, Alonso J, Prieto L, Plaza V, Monso E, Marrades R, Aguar MC, Khalaf A, Anto JM. Validity and reliability of the St George's Respiratory Questionnaire after adaptation to a different language and culture: the Spanish example. Eur Respir J. 1996; 9:1160–1166.

22. Cronbach LJ, Warrington WG. Time-limit tests: estimating their reliability and degree of speeding. Psychometrika. 1951; 16:167–188.

24. Nunnally JC, Bemstein IH. Psychometric theory. 3rd ed. New Delhi: Tata McGraw-Hill Education;2010.
26. Fletcher C. Standardised questionnaire on respiratory symptoms: a statement prepared and approved by the MRC Committee on the Aetiology of Chronic Bronchitis (MRC breathlessness score). Br Med J. 1960; 2:1665.
27. Kim SH, Lee JY, Son SW, Chang YS, Jung JW, Kim YK, Cho SH, Min KU, Kim YY. Prevalence of adult asthma based on questionnaires and methacholine bronchial provocation test in Seoul. J Asthma Allergy Clin Immunol. 2001; 21:618–627.
28. Kim YK, Kim SH, Tak YJ, Jee YK, Lee BJ, Kim SH, Park HW, Jung JW, Bahn JW, Chang YS, Choi DC, Chang SI, Min KU, Kim YY, Cho SH. High prevalence of current asthma and active smoking effect among the elderly. Clin Exp Allergy. 2002; 32:1706–1712.

29. Song WJ, Kim SH, Lim S, Park YJ, Kim MH, Lee SM, Lee SB, Kim KW, Jang HC, Cho SH, Min KU, Chang YS. Association between obesity and asthma in the elderly population: potential roles of abdominal subcutaneous adiposity and sarcopenia. Ann Allergy Asthma Immunol. 2012; 109:243–248.

30. Choi MH, Chang YS, Lim MK, Bae YM, Hong ST, Oh JK, Yun EH, Bae MJ, Kwon HS, Lee SM, Park HW, Min KU, Kim YY, Cho SH. Clonorchis sinensis infection is positively associated with atopy in endemic area. Clin Exp Allergy. 2011; 41:697–705.

31. Song WJ, Chang YS, Lim MK, Yun EH, Kim SH, Kang HR, Park HW, Tomassen P, Choi MH, Min KU, Cho SH, Bachert C. Staphylococcal enterotoxin sensitization in a community-based population: a potential role in adult-onset asthma. Clin Exp Allergy. 2014; 44:553–562.

32. Ferris B. Recommended respiratory disease questionnaires for use with adults and children in epidemiological research. Am Rev Respir Dis. 1978; 118:7–54.
33. Liard R, Neukirch F. Questionnaires: a major instrument for respiratory epidemiology. Eur Respir Monogr. 2000; 15:154–166.
34. Toelle BG, Peat JK, Salome CM, Mellis CM, Woolcock AJ. Toward a definition of asthma for epidemiology. Am Rev Respir Dis. 1992; 146:633–637.

35. Jenkins MA, Clarke JR, Carlin JB, Robertson CF, Hopper JL, Dalton MF, Holst DP, Choi K, Giles GG. Validation of questionnaire and bronchial hyperresponsiveness against respiratory physician assessment in the diagnosis of asthma. Int J Epidemiol. 1996; 25:609–616.

36. Kang MK, Kim BK, Kim TW, Kim SH, Kang HR, Park HW, Chang YS, Kim SS, Min KU, Kim YY, Cho SH. Physicians' preferences for asthma guidelines implementation. Allergy Asthma Immunol Res. 2010; 2:247–253.

37. Kim SH, Cho SH. Educational and decision-support tools for asthmamanagement guideline implementation. Asia Pac Allergy. 2012; 2:26–34.

38. Jo EJ, Kim MY, Jeon Y, Kwon JW, Na JI, Kim SH, Rhee CS, Cho SH, Min KU, Chang YS. Educational demand on allergic diseases from 45 public health centers in Gyeonggi-do. Allergy Asthma Respir Dis. 2013; 1:55–59.

39. Samet JM. Epidemiologic approaches for the identification of asthma. Chest. 1987; 91:6 Suppl. 74S–78S.

40. Crapo RO, Casaburi R, Coates AL, Enright PL, Hankinson JL, Irvin CG, MacIntyre NR, McKay RT, Wanger JS, Anderson SD, Cockcroft DW, Fish JE, Sterk PJ. Guidelines for methacholine and exercise challenge testing-1999. This official statement of the American Thoracic Society was adopted by the ATS Board of Directors, July 1999. Am J Respir Crit Care Med. 2000; 161:309–329.
41. Pekkanen J, Sunyer J, Anto JM, Burney P. European Community Respiratory Health Study. Operational definitions of asthma in studies on its aetiology. Eur Respir J. 2005; 26:28–35.

SUPPLEMENTARY MATERIALS
Supplementary Tables can be found via http://www.apallergy.org/src/sm/apallergy-5-25-s001.pdf. Supplementary Table 1. The European Community Respiratory Health Survey phase II screening questionnaire in English. Supplementary Table 2. The Korean translated version of the European Community Respiratory Health Survey phase II screening questionnaire.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download