Abstract
Background
Anaphylaxis is a serious allergic reaction that may cause death. The signs and symptoms of anaphylaxis have not been examined in the Saudi population before.
Objective
The present study examined the signs, symptoms, triggers, and demographic patterns of patients treated for anaphylaxis at a large tertiary care hospital in Riyadh, Saudi Arabia.
Methods
All the patients who were prescribed new prescriptions of adrenaline auto-injectors (AAs) between February 1, 2010 and December 31, 2011 were included in this study. Information was collected using a standardized form.
Results
There were 238 patients who were analyzed. The median age at the time of first AA prescription was 15.5 years. Female to male ratio was 52:48 and 54% of the subjects were more than 18 years of age. There were some differences in the presenting signs and symptoms observed in our study compared with similar studies from around the world. Urticaria and angioedema were the most common at about 70% across all ages, followed by shortness of breath at 28%. Some triggers were found to be more common in our region. Food was the commonest trigger for anaphylaxis including tree nuts, egg, and sesame. Drug allergy was also a common trigger, with penicillins and nonsteroidal anti-inflammatory drugs being the commonest. Regarding insect allergy, samsam ant was the commonest trigger in our study.
Conclusion
To our knowledge, this is the first study on anaphylaxis in Saudi Arabia. Some of the manifestations of anaphylaxis are significantly different in our population study compared to previously published data from other parts of the world. While managing anaphylaxis, we should be mindful of these differences. This improved understanding should help reduce the morbidity and mortality associated with anaphylaxis in our region.
Anaphylaxis is a serious allergic reaction that is rapid in onset and may cause death [1]. Anaphylactic reactions can be triggered by allergic responses to a wide range of substances including food, medications, insect stings, and latex. Lifetime prevalence of anaphylaxis is up to 2% with the largest number of cases being reported among children and adolescents [2]. Anaphylaxis occurs in 30 per 100,000 people annually in the United States with a reported mortality of 1-2% [3]. The rate of occurrence is increasing in industrialized countries [4]. The incidence and prevalence of anaphylaxis in Saudi Arabia is unknown.
Common symptoms and signs of anaphylaxis include skin and respiratory manifestations in up to 90%, and 70% respectively. In addition, gastrointestinal and cardiovascular systems are involved up to 45% each [5678].
Prompt assessment and treatment are critical in anaphylaxis, as respiratory or cardiac arrest and death can occur within minutes [9]. Prompt intramuscular injection of adrenaline is one of the cornerstones of treatment of anaphylaxis [10]. It is therefore important to study the dispensing of adrenaline in different geographical regions. This will help us understand the epidemiology of anaphylaxis and aid ongoing efforts to reduce morbidity and mortality associated with it and could provide important clues for its primary prevention. Global agenda for anaphylaxis research according to the World Allergy Organization anaphylaxis guidelines also stress the importance of epidemiologic research in anaphylaxis [11]. Similar work has already been published from other parts of the world [1213].
The aim of the study was to examine the frequency of signs, symptoms, triggers, and demographic patterns of anaphylaxis using the prescription pattern of AAs at a large tertiary care center in Riyadh, Saudi Arabia.
All patients given new prescriptions of AAs at our hospital between February 1, 2010 and December 31, 2011 were included in this study.
Patients prescribed AAs were identified using hospital Pharmacy database and the case records of these patients were retrospectively reviewed. Clinical data was collected using a standardized form that included information on demographics and indications for AA prescriptions.
The data was subclassified by age, gender, nationality, triggers, signs and symptoms, as well as the geographical location within Saudi Arabia.
The protocol was approved by the Research Advisory Committee of the hospital. This was a retrospective review of our hospital records which did not require any intervention, device or patient interaction and presented no risk to the patients at all. All patients who had received AAs during the study period outlined above were reviewed for descriptive data such as age, gender, and indications. Patients were not contacted during the duration of the chart review. All the data collected was anonymous and patient identifiers such as medical record number, date of birth were deleted once data was analysed using the SPSS ver. 12.0. Only the principal investigator had access to the complete data and other coinvestigators did not store the data but passed it on to him for analyses and filing in the SPSS software.
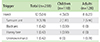
This study looked at 238 new patients who were prescribed AAs over a period of 2 years. There were 238 patients who were analyzed. The median age at the time of first AA prescription was 15.5 years. Female to male ratio was 52:48 and 54% of the subjects were more than 18 years of age. Most of these prescriptions were given to Saudi patients mainly from Riyadh area but also from most other parts of the Kingdom. However about 18% were given to Non Saudis living in the Riyadh region. Most of these were employees of the hospital or their dependents (Table 1).
Urticaria and angioedema were the most common sign or symptom with about 70% across adults and children. The second most common symptom was shortness of breath which was about 33% in adults and 23% in children. Nausea and vomiting was reported in about 9% of our subjects. Itching without rash was noticed in about 8%. Other infrequent signs or symptoms are detailed (Table 2).
Food was the commonest trigger for anaphylaxis, out of which tree nuts and egg were the most frequent, followed by sesame, milk, and peanut, respectively (Table 3). Dates are commonly consumed in this part of the world and were also reported as a trigger in a few individuals. As expected, overall food allergy was more common in children, but shrimp allergy was more frequently reported in adults.
Anaphylaxis signs and symptoms are being reported from many areas around the world. It is also observed that allergies and anaphylaxis incidence is on the rise. It is therefore important to understand more about this life threatening condition in our region.
The only approved indication for AAs is anaphylaxis. It is available only at a few centers in Saudi Arabia. In a large tertiary care hospital it should provide us with a good estimate of the anaphylaxis patterns in our population. However, as the AAs are also available at a few other hospitals in the country, our data may not reflect the complete burden of anaphylaxis in our region.
The observation regarding signs and symptoms again reiterates an important fact regarding anaphylaxis recognition and management. Not all patients with anaphylaxis would present with skin signs or symptoms. Although most of the signs and symptoms were similar to other published data, there were some differences observed in our study population [14] (Table 2).
As observed in many of the other populations, the commonest sign or symptom of anaphylaxis in our study population was also urticaria/angioedema. However it was slightly less common and was reported in about 71% of people. Shortness of breath was reported in 28% of the other studies. This was also less commonly observed compared to some of the other populations. Dizziness, syncope, and hypotension were seen equally (about 8% of the study population) and were significantly less compared with some of the other areas. In addition to ethnic differences that may be present, suboptimal recognition of patients with anaphylaxis may have resulted in the observed differences between reported signs and symptoms in our population. Further studies are needed from our part of the world to validate this finding.
Food allergy was the commonest trigger for anaphylaxis in our study population (Table 3). The leading triggers were tree nut, egg, sesame, peanut, and milk, respectively. Another interesting fact was that sesame allergy was much more common in our region compared to peanut allergy. Ethnic differences in food exposures and consumptions may explain some of these differences.
Among the other triggers, penicillin, NSAIDs and sulfa were the most commonly encountered (Table 4). Cholinergic urticaria also known as generalized heat urticaria which is triggered by a rise in body temperature and can be complicated by bronchial hyperresponsiveness and anaphylaxis was found in about 6% of patients [14].
Latex allergy was seen in 3.4% of our study subjects. Food allergy as a cause of anaphylaxis was observed more commonly in children, while other triggers for anaphylaxis were more commonly observed in adults (Fig. 1).
Among the insects (Table 5), samsam ant which is native to our region was the commonest insect allergy in our study population. There is no commercial extract available for testing or desensitization and there is an urgent need for its development for our population. There were no cases reported for hornet/yellow jacket or wasp allergy. The exact triggers for food dependent exercise-induced anaphylaxis were not identified.
In conclusion, this is the first study on anaphylaxis in Saudi Arabia. While there are many similarities to other published data, some of the presenting signs, symptoms, and triggers of anaphylaxis are significantly different in our study population. While managing anaphylaxis, we should be mindful of these differences. This improved understanding should help reduce the morbidity and mortality associated with anaphylaxis in our region.
Figures and Tables
Fig. 1
Common triggers. Comparison of triggers between children and adults. Incidence specified according to age. NSAID, nonsteroidal antiinflammatory drug.

References
1. Sampson HA, Munoz-Furlong A, Campbell RL, Adkinson NF Jr, Bock SA, Branum A, Brown SG, Camargo CA Jr, Cydulka R, Galli SJ, Gidudu J, Gruchalla RS, Harlor AD Jr, Hepner DL, Lewis LM, Lieberman PL, Metcalfe DD, OConnor R, Muraro A, Rudman A, Schmitt C, Scherrer D, Simons FE, Thomas S, Wood JP, Decker WW. Second symposium on the definition and management of anaphylaxis: summary report: Second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network symposium. J Allergy Clin Immunol. 2006; 117:391–397.
2. Lieberman P, Camargo CA Jr, Bohlke K, Jick H, Miller RL, Sheikh A, Simons FE. Epidemiology of anaphylaxis: findings of the American College of Allergy, Asthma and Immunology Epidemiology of Anaphylaxis Working Group. Ann Allergy Asthma Immunol. 2006; 97:596–602.

3. Golden DB. Patterns of anaphylaxis: acute and late phase features of allergic reactions. Novartis Found Symp. 2004; 257:101–110.

4. Liew WK, Williamson E, Tang ML. Anaphylaxis fatalities and admissions in Australia. J Allergy Clin Immunol. 2009; 123:434–442.

5. Ewan PW, Dugue P, Mirakian R, Dixon TA, Harper JN, Nasser SM. BSACI. BSACI guidelines for the investigation of suspected anaphylaxis during general anaesthesia. Clin Exp Allergy. 2010; 40:15–31.

6. Chacko T, Ledford D. Peri-anesthetic anaphylaxis. Immunol Allergy Clin North Am. 2007; 27:213–230.

7. Harboe T, Benson MD, Oi H, Softeland E, Bjorge L, Guttormsen AB. Cardiopulmonary distress during obstetrical anaesthesia: attempts to diagnose amniotic fluid embolism in a case series of suspected allergic anaphylaxis. Acta Anaesthesiol Scand. 2006; 50:324–330.

8. Ebo DG, Bosmans JL, Couttenye MM, Stevens WJ. Haemodialysisassociated anaphylactic and anaphylactoid reactions. Allergy. 2006; 61:211–220.

9. Pumphrey RS. Lessons for management of anaphylaxis from a study of fatal reactions. Clin Exp Allergy. 2000; 30:1144–1150.

10. Simons FE. First-aid treatment of anaphylaxis to food: focus on epinephrine. J Allergy Clin Immunol. 2004; 113:837–844.

11. Simons FE, Ardusso LR, Bilo MB, El-Gamal YM, Ledford DK, Ring J, Sanchez-Borges M, Senna GE, Sheikh A, Thong BY. World Allergy Organization. World Allergy Organization anaphylaxis guidelines: summary. J Allergy Clin Immunol. 2011; 127:587–593.e1-22.

12. Mullins RJ, Clark S, Camargo CA Jr. Regional variation in epinephrine autoinjector prescriptions in Australia: more evidence for the vitamin D-anaphylaxis hypothesis. Ann Allergy Asthma Immunol. 2009; 103:488–495.

13. Tham EH, Tay SY, Lim DL, Shek LP, Goh AE, Giam YC, Chng HH, Lee BW. Epinephrine auto-injector prescriptions as a reflection of the pattern of anaphylaxis in an Asian population. Allergy Asthma Proc. 2008; 29:211–215.

14. Handfield KS, Dolan CK, Kaplan M. Cholinergic urticaria with anaphylaxis: hazardous duty of a deployed US marine. Cutis. 2015; 95:241–243.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download