Abstract
Background
Chronic urticaria is a common skin condition that causes significant impact on patient's quality of life.
Objective
The purpose of the study was to assess adherence to therapy and quality of life of patients with chronic urticaria. We also aimed to study the relationship of medication adherence and quality of life of patients with chronic urticaria.
Methods
A cross sectional study was conducted with 103 patients from the dermatology clinic of National University Hospital, Singapore. Patients with chronic urticaria were asked to fill out a questionnaire for assessment of adherence to therapy and quality of life. We used the Morisky 8-Item Medication Adherence Scale to categorize adherence as high, medium, low. For assessment of quality of life, we used the validated chronic urticaria quality of life questionnaire (CU-Q2oL) by Bairadani et al.
Results
The highest median scores for the items measuring quality of life were interference with sleep and pruritus. We also observed that the majority of patients (71.9%) had low adherence to medical therapy. No difference in adherence was noted in patients on once daily medication or more frequent dosing. There was no significant difference in the quality of life among patients with low and medium adherence to therapy.
Conclusion
Quality of life of patients with chronic urticaria does not depend on the patients' adherence to medications. Dosing frequency does not affect adherence in our study population. It is also important to recognize the symptoms and issues most affecting quality of life of patients with chronic urticaria, so as to improve overall management.
Chronic urticaria (CU) is a common skin disease that is characterized by the appearance of fleeting itchy wheals which each last between 1 to 24 hours, and/or angioedema, which is present on a regular basis for at least 6 weeks. It is estimated that lifetime prevalence for any subtype of urticaria is approximately 20% [1]. The etiology of CU is unknown for the majority of cases. This has led to difficulties of adequate pharmacological treatment and symptom control, thus causing a significant impact on patients' quality of life (QoL). The first line treatment is second-generation nonsedating H1 antihistamines and if standard dosing is not effective, increasing the dosage up to fourfolds is recommended. Second-line therapies should be added if patients still fail to respond. In addition to a decrease in QoL, CU also affects performance at work and school and as such, is a member of the group of severe allergic diseases [1].
Many studies have been done to establish the extent of QoL impairment in CU patients. The physical discomfort and effect on activities of daily living are comparable to those suffering from atopic dermatitis and more severe than psoriasis [2]. To date, there have been no studies assessing patient's adherence to therapy and the relationship between medication adherence and QoL of patients with CU. Because CU often lasts for many years, it would be useful to find out the adherence to treatment, and whether adherence to treatment affects QoL. If a positive relationship is found, more emphasis can be placed on reinforcing adherence to therapy so as to improve patients' QoL. It is crucial for physicians to understand the factors affecting adherence to medications, so as to tailor more effective treatment regimens for patients.
The purpose of the study was to assess adherence to therapy, evaluate patients' QoL and the relationship between adherence to therapy and QoL. We also aim to describe the characteristics of patients seeking treatment, the frequency of the different types of CU and how different treatment regimens affect adherence to therapy.
A prospective, cross-sectional investigation was conducted in 2014 over a course of one year. Patients with CU attending the University Dermatology Clinic in National University Hospital, Singapore, were invited to do fill out a questionnaire. Data was collected primarily by self-administered questionnaires. Diagnosis of CU was made based on history and physical examination by the attending dermatologist. The inclusion criteria were: (1) individuals with erythematous wheals with or without angioedema every day or almost every day lasting for at least 6 weeks, (2) patients that were at least 21 years old and (3) patients who could read and answer the questions on the questionnaire by themselves. The following groups of patients were excluded: (1) patients with other skin disorders or serious systemic diseases that could also impact QoL and (2) patients who did not answer all the questions in the questionnaire.
The European Academy of Allergy and Clinical Immunology/Global Allergy and Asthma European Network/European Dermatology Forum/World Allergy Organization (EAACI/GA2LEN/EDF/WAO) guideline [1] was used to categorize urticaria cases into the following three types: chronic spontaneous urticaria, physical urticaria (which includes delayed physical urticaria, cold/heat contact urticaria, solar urticaria, dermographic urticaria, and vibratory urticaria), and other types of urticaria (which includes aquagenic, cholinergic, contact, and exercise-induced urticaria). The local ethics committee approved this study.
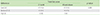
For assessment of medication adherence, the Morisky 8-Item Medication Adherence Scale [3] (MMAS-8) was used. Adherence on the MMAS-8 was categorized as high, medium, and low (MMAS-8 scores of 0, 1 to 2, and 3 to 8, respectively) (Table 1). The MMAS-8 has been demonstrated to have good concurrent and predictive validity and function as a screening tool in outpatient settings with different patient groups. The validated chronic urticaria quality of life questionnaire (CU-Q2oL) by Baiardini et al. [4] with modifications was used to evaluate the impact of CU on QoL (Table 2). We omitted the questions on interferences with physical activities and eating behaviour, difficulties in keeping concentration and feeling nervous. In the original article by Baiardini et al. [4], these four questions did not show a statistically significant difference in patients who reported significant diminished symptoms. The questions on eye and lip swelling were combined to form a question on swelling. The CU-Q2oL questionnaire was specifically developed for use in patients with CU and encompasses the physical, emotional, social, and practical domains that characterize this condition. With a total of 18 items, each item was scored from 1 to 5; score 1 was given when the patient was not affected and 5 was given when the patient was most affected. The total QoL scores were calculated; lower QoL scores represents a better QoL whereas higher QoL scores shows that the patient was more affected. A case-note audit was done to obtain the patients' sociodemographic characteristics, disease duration, urticaria subtype, comorbidities, and their medication regimens.
Data was analyzed using the IBM SPSS Statistics ver. 22.0 (IBM Co., Armonk, NY, USA). The median and interquartile range of the 18 questions of the CU-Q2oL were described and compared by gender, age, and duration of CU. Hypothesis testing was conducted using the Kruskal-Wallis one-way analysis of variance by ranks. probability (p) of <0.05 was considered statistically significant.
In total, 103 patients with CU completed the questionnaire and data was analyzed. Forty-nine men and 54 women participated. The mean age of the patients was 43.18 ± 0.24 years (range, 21-79 years). The median duration of CU was more than 2 years, with a range from 1.5 to 120 months. Table 3 summarises the characteristics of the study population.
Overall, patients were most affected by urticaria interfering with their sleep (median, 5; mean, 3.24; standard deviation [SD], 1.34) and pruritus (median, 4; mean, 3.72; SD, 1.13). This is followed by feeling tired during the day because of a bad night sleep (median, 3; mean, 3.05; SD, 1.32) and interference with spare time (median, 3; mean, 2.92; SD, 1.29). Patients were least affected by the side effects from their medications (median, 1; mean, 1.77; SD, 1.14) and problems using cosmetics (median, 1; mean, 1.38; SD, 0.85) (Table 2).
Females had more interference with sleep as compared to males (mean rank score: 57.93 vs. 45.47, p < 0.05). In addition, urticaria significantly affected the mood of females more than males (mean rank score: 45.41 vs. 57.98, p < 0.05). Females were also more affected by embarrassment of their conditions (mean rank score: 45.99 vs. 57.45, p < 0.05) and embarrassment when going out into public places (mean rank score: 43.16 vs. 60.02, p < 0.01). Females were also more affected by having limits on choosing the material of their clothes (mean: 45.28 vs. 58.10, p < 0.05). Those older than 40 years of age were more likely to wake up at night by CU (mean rank score: 43.49 vs. 58.35, p < 0.05) and they were also more likely to place limits on clothing material (mean rank score: 44.67 vs. 57.47, p < 0.05). There was no significant difference observed when comparing the duration of CU on the various parameters (Table 2).
The total score of the CU-Q2oL in patients with CU ranged from 21 to 80 with a median of 45.0. Majority of the patients had low adherence to medical therapy (71.9%). In our study population, 25.2% had medium adherence to therapy whilst 2.9% had high adherence scores to therapy. Patients who had once daily medication compared to those with more frequent dosing did not have any difference in adherence (Table 4). There was no significant difference in the QoL amongst patients with low and medium adherence to therapy (Table 5). Three patients with high adherence to therapy had lower total QoL scores compared to the median.
The current EAACI/GA2LEN/EDF/WAO guidelines on the definition, classification and diagnosis of urticaria [1] recommend the use of the disease-specific QoL questionnaire for assessing QoL impairment and to monitor disease activity. The CU-Q2oL meets the standards for validity with good construct validity, internal consistency, reliability, and responsiveness. This study was performed to evaluate the impact of CU on patients' QoL and investigate the relationship between QoL impairment and adherence to therapy by using the tools recommended by the guidelines.
We analyzed the impact of CU on the various aspects of QoL. Previous studies [56] have described that CU has a significant impact on QoL especially on sleep and energy levels and this is consistent with our results. Our population was also significantly affected by itch. The sensation of itch might have been exacerbated by the warm and humid climate in Singapore. Patients were least affected by the side effects from their medications and had no difficulties with make-up application. We also calculated the total QoL scores for each patient which showed that the median score was 45.0, indicating a "moderate impairment" of QoL.
Gender-based and age-based differences were also noted in QoL. Our study results showed that women had more interference with sleep compared to men, and women tended to be more embarrassed by their condition than men. It is also not surprising to find that women find more limitations in choosing the material of their clothes, and that women find their mood more significantly affected than men. We propose that more attention should be placed on patients' psychological wellbeing, especially for female patients. Older patients were more affected by waking up during the night and a possible solution is to prescribe longer-acting medications at night when treating older patients, so that their sleep will be less interrupted. The use of a sedative antihistamine may seem as an attractive measure but physicians should carefully balance the benefit against the risk of daytime somnolence and falls in the elderly.
CU often lasts for many years and many CU patients remain afflicted by the condition despite medications. Treatment is provided on an outpatient basis and adherence to therapy is largely at the discretion of the patients. Many previous studies on acne, psoriasis and eczema consistently show that QoL is better when there is higher adherence to medication [789]. Our study showed a surprising lack of correlation. The overall low adherence rate (71.9%) may be attributed to concerns about taking regular oral medications, inconvenience, forgetfulness and lack of efficacy of the medications. Our results also showed a general absence of side effects to medications.
In addition, it is known that with a higher the dosing frequency of medication, there is poorer adherence [10]. CU patients prescribed with once daily dosages did not show any difference in adherence when compared with those on more frequent dosing regimens. Confounding factors such as severity of disease, patient's knowledge about their condition, patients' attitudes towards long-term oral medication, may have accounted for such unusual phenomena.
In conclusion, our study showed that CU has a significant impact on QoL (moderate impairment) especially on sleep and energy levels. We have also shown that medication adherence did not affect QoL, and dosing frequency did not affect adherence. There are likely to be other confounding factors at play and further studies with higher subject numbers could be conducted to elucidate these factors.
Figures and Tables
References
1. Zuberbier T, Aberer W, Asero R, Bindslev-Jensen C, Brzoza Z, Canonica GW, Church MK, Ensina LF, Gimenez-Arnau A, Godse K, Gonçalo M, Grattan C, Hebert J, Hide M, Kaplan A, Kapp A, Abdul Latiff AH, Mathelier-Fusade P, Metz M, Nast A, Saini SS, Sanchez-Borges M, Schmid-Grendelmeier P, Simons FE, Staubach P, Sussman G, Toubi E, Vena GA, Wedi B, Zhu XJ, Maurer M. European Academy of Allergy and Clinical Immunology. Global Allergy and Asthma European Network. European Dermatology Forum. World Allergy Organization. The EAACI/GA(2) LEN/EDF/WAO Guideline for the definition, classification, diagnosis, and management of urticaria: the 2013 revision and update. Allergy. 2014; 69:868–887.
2. Grob JJ, Revuz J, Ortonne JP, Auquier P, Lorette G. Comparative study of the impact of chronic urticaria, psoriasis and atopic dermatitis on the quality of life. Br J Dermatol. 2005; 152:289–295.

3. Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich). 2008; 10:348–354.

4. Baiardini I, Pasquali M, Braido F, Fumagalli F, Guerra L, Compalati E, Braga M, Lombardi C, Fassio O, Canonica GW. A new tool to evaluate the impact of chronic urticaria on quality of life: chronic urticaria quality of life questionnaire (CU-QoL). Allergy. 2005; 60:1073–1078.
5. Yun J, Katelaris CH, Weerasinghe A, Adikari DB, Ratnayake C. Impact of chronic urticaria on the quality of life in Australian and Sri Lankan populations. Asia Pac Allergy. 2011; 1:25–29.

6. O'Donnell BF, Lawlor F, Simpson J, Morgan M, Greaves MW. The impact of chronic urticaria on the quality of life. Br J Dermatol. 1997; 136:197–201.
7. Augustin M, Holland B, Dartsch D, Langenbruch A, Radtke MA. Adherence in the treatment of psoriasis: a systematic review. Dermatology. 2011; 222:363–374.

8. Jones-Caballero M, Pedrosa E, Peñas PF. Self-reported adherence to treatment and quality of life in mild to moderate acne. Dermatology. 2008; 217:309–314.

9. Staab D, Diepgen TL, Fartasch M, Kupfer J, Lob-Corzilius T, Ring J, Scheewe S, Scheidt R, Schmid-Ott G, Schnopp C, Szczepanski R, Werfel T, Wittenmeier M, Wahn U, Gieler U. Age related, structured educational programmes for the management of atopic dermatitis in children and adolescents: multicentre, randomised controlled trial. BMJ. 2006; 332:933–938.

10. Saini SD, Schoenfeld P, Kaulback K, Dubinsky MC. Effect of medication dosing frequency on adherence in chronic diseases. Am J Manag Care. 2009; 15:e22–e33.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download