Abstract
Background
Allergic rhinitis is characterized by eosinophil inflammation. Allergic inflammation may induce susceptibility to respiratory infections (RI). House dust mite (HDM) sensitization is very frequent in childhood. Allergen immunotherapy may cure allergy as it restores a physiologic immune and clinical tolerance to allergen and exerts anti-inflammatory activity.
Objective
This study investigated whether six-month high-dose, such as 300 IR (index of reactivity), HDM-sublingual immunotherapy (SLIT) could affect RI in allergic children.
Methods
Globally, 40 HDM allergic children (18 males; mean age, 9.3 years) were subdivided in 2 groups: 20 treated by symptomatic drugs (group 1) and 20 by high-dose HDM-SLIT (group 2), since September 2012 to April 2013. The daily maintenance dose of HDM-SLIT was 4 pressures corresponding to 24, 4.8, and 60 µg, respectively of the major allergens Dermatophagoides pteronyssinus (Der p) 1, Der p 2, and Dermatophagoides farinae (Der f) 1. RI was diagnosed when at least 2 symptoms or signs, and fever were present for at least 48 hours. A family pediatrician provided diagnosis on a clinical ground.
Results
SLIT-treated children had significantly (p = 0.01) less RI episodes (3.5) than control group (5.45). About secondary outcomes, SLIT-treated children had less episodes of pharyngo-tonsillitis (p < 0.05) and bronchitis (p < 0.005), and snoring (p < 0.05) than control group. In addition, SLIT-treated children had less fever (p < 0.01) and took fewer medications, such as antibiotics (p < 0.05) and fever-reducers (p < 0.01), than control group.
Social and economic costs of allergic rhinitis (AR) are relevant as AR may significantly impact school attendance and performance, quality of life, sleep, and is associated with many comorbidities, including asthma and respiratory infections (RI) [12].
The AR immunopathology is characterized by T helper 2 (Th2)-dependent inflammation and Th1-response impairment. This imbalance is sustained by dysfunction of immune system: allergic patients have a functional defect of allergen-specific T regulatory cells, so Th2 cells may polarize the immune response to allergen and produce large quantity of some interleukins, including interleukin (IL) 4, IL-5, and IL-13, that in turn promote IgE synthesis and eosinophil production, recruitment, and activation at nasal level. Th2-cytokines up-regulate the endothelial and epithelial expression of adhesion molecules (such as intercellular adhesion molecule [ICAM-1]), which interact with other adhesion molecules (e.g., leukocyte functional adhesion-1 expressed by leukocytes) to induce the mucosal infiltration by eosinophil. In addition, involvement of other T helper subsets, namely Th17 and Th9, has been reported. Severity of AR may be associated with increased levels of IL-17 and IL-9. This complex pathogenesis highlights the relevant impairment of immune response in AR. In addition, Th2-, Th1-, and Th9-dependent cytokines are involved in inflammatory events. Therefore, allergic inflammation represents the main characteristic of AR.
It is strengthened belief that allergic patients could present higher susceptibility to contract RI than nonallergic subjects. In this regard, it has been evidenced that allergic children have more numerous and severe RI than nonallergic children [3]. The involved pathways may be: (1) impaired immune defence because of interferon (IFN)-γ defective production, consequent to Th2-polarization [45], (2) overexpression of ICAM-1 (the main rhinovirus receptor) depending on allergen exposure, (3) augmented mucus production together with impaired mucus consistency, and (4) persistent mucosal inflammation as pabulum for microbes overgrowth [56]. In addition, it is well known that AR is a main risk for asthma [7], both concerning the onset and the worsening [8]. In other words, allergic reaction may be considered the promoter of different sequential steps: (1) allergen exposure induces expression of adhesion molecules, (2) so allergic inflammation flares, (3) symptoms occur, (4) overexpression of ICAM-1 favours viral adherence, (5) RI cause asthma attack. Therefore, adequate control of allergic inflammation in AR patients is important as it induces symptom relief and could prevent infections recurrence [9]. In this regard, allergen immunotherapy (AIT) may restore a physiological immune and clinical tolerance to the causal allergen and exert anti-inflammatory effects, mainly concerning a fast increase of IFN-γ production after AIT [1011]. In addition, it has been reported that sublingual immunotherapy (SLIT) may reduce the number of RI in children with AR [12]. Children treated with SLIT actually had less allergic symptoms than control children as well as they had significantly less sore throat, headache, productive cough, and antibiotic use than children treated with medications alone [12]. In this regard, it may be hypothesized that these beneficial effects might be based on a restored physiological Th1-polarization and a damping of allergic inflammation [13].
House dust mite (HDM) sensitization is very frequent in childhood and is characterized by a persistence of Th2-dependent allergic inflammation [14]. Therefore, the present preliminary study investigated whether six-month SLIT at high dose may reduce the number of RI in HDM allergic children.
Forty children, aging between 7-14 years, with AR to HDM were included. For inclusion, patients had to have typical symptoms of AR (such as sneezing, itching, watery rhinorrhea, and nasal obstruction) throughout the year with fall-winter peak for at least 2 consecutive years, moderate-severe AR (according to Allergic Rhinitis and its Impact on Asthma [ARIA] criteria), and a documented positive skin prick test to HDM extracts consistent with symptom occurrence after exposure to dust. The main exclusion
criteria were AR caused by cosensitization and likely to influence symptoms evaluation during the study, previous AIT, and the usual contraindications to AIT.
This observational study was conducted at Pediatrics Department of the San Paolo Hospital (Milan, Italy) from September 2012 to April 2013. Allergic children were subdivided in 2 groups: 20 patients were treated by symptomatic drugs (antihistamines, nasal corticosteroids) (group 1) and 20 children by high dose, such as 300 IR (index of reactivity) SLIT (group 2).
AR severity was assessed according to the ARIA criteria, such as AR could be intermittent or persistent on the basis of the symptom duration [1].
The primary objective of the study was to investigate whether high-dose SLIT was able to reduce the total number of RI in patients with HDM-AR.
The secondary objectives were to assess whether high-dose SLIT could affect: the number of episodes of acute rhinosinusitis, otitis, pharyngotonsillitis, laryngitis, bronchitis, and pneumonia, the presence of fever, the snoring, the use of antibiotics, anti-inflammatory drugs, oral corticosteroids, and fever-reducers.
For data collection, parents had a diary card. Parents daily collected on the card the presence of signs and symptoms, including fever, rhinorrhea, stuffy and dripping nose, snoring, sore-throat, earache, dysphonia, cough, and dyspnea.
Written informed consent was obtained by both parents before entering the study. The study was conducted in accordance with good clinical practice guidelines. The study was approved by the Ethics Committee of the San Paolo Hospital (Milan, Italy).
RI diagnosis was based on a clinical ground [15]. The RI diagnosis was made when symptoms, reported by parents in the diary, and fever (axillary temperature ≥ 38℃) were present for at least 48 hours. The symptoms (in addition to fever) taken into consideration for this diagnostic purpose were: (1) mucopurulent rhinorrhea, stuffy or dripping nose, headache for <10 days for common cold, for >10 days for rhinosinusitis, (2) sore-throat, and cough for pharyngotonsillitis, (3) otalgia (earache) for otitis, (4) dysphonia and dry cough for laryngitis, (5) cough (dry and/or productive) and dyspnea for lower RI. RI diagnosis was usually confirmed by a family pediatrician.
The most widely used antibiotic was amoxicillin (or amoxicillin with clavulanic acid), and it was usually prescribed for 7 days at a dose of 50 mg/kg per day, divided into 3 doses. Clarithromycin was the second most prescribed antibiotic by pediatricians at a dose of 15 mg/kg per day, divided in 2 doses, and prescribed for 14 days. Cefpodoxime proxetile was prescribed only 3 times for 10 days at a dose of 8 mg/kg per day, divided in 2 doses.
SLIT was performed using an allergen extract of HDM at 300 IR/mL (Stallergenes S.A., Antony, France). Staloral 300 contains equal proportions of Dermatophagoides pteronyssinus (Der p) and Dermatophagoides farinae (Der f) and is available as a minipump-predosed actuator. It was administered according to a 6-month schedule. The daily maintenance dose of HDM SLIT was 4 pressures corresponding to 24, 4.8, and 60 µg, respectively of the major allergens: Der p 1, Der p 2, and Der f 1. Any local or systemic adverse effect of SLIT was recorded by the patients.
Children were checked at the clinic every two months. During each visit, diary cards were assessed, physical examination was performed, and SLIT compliance and tolerance were considered.
The sample size was calculated by log-rank test with power at 90% and a error at 5%: 20 subjects per arm were considered sufficient based a supposed difference in efficacy of at least 20%.
A central organization (IBIS Informatica, Milan, Italy) undertook the data entry and statistical analysis. Nominal and discrete parameters were reported as contingency tables (frequency and percentage). The statistical analysis was conducted with parametric (analysis of variance) and nonparametric methods (Mann-Whitney test). The contingency tables were assessed through chi-square test with Yate correction in the case of 2×2 tables. Statistical analysis was carried out using BMDP Dynamic 2009 ver. 8.2 (BMDP Statistical Software, Inc., Los Angeles, CA, USA).
We assessed 40 paediatric patients (18 males; mean age, 9.3 ± 1.8 years), 20 undergoing symptomatic drugs alone (group 1) and 20 treated by SLIT (group 2).
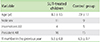
The two groups were well matched concerning age, gender, AR severity, RI episodes in the previous year, as reported in Table 1.
The total number of infections was significantly different in the two groups: Group 1 had more (p < 0.05) RI episodes (5.45) than SLIT group (3.5) (Fig. 1). In particular, the number of pharyngo-tonsillitis episodes was minor (p < 0.05) in SLIT-treated patients (Fig. 2A) as well as the bronchitis episodes was significantly minor (p < 0.05) in group 2 (Fig. 2B). Snoring was significantly (p < 0.05) reduced in SLIT group in comparison with control group as shown in Fig. 2C. About fever, 18 children treated with medications alone had fever, whereas only 8 SLIT-treated children had fever (p < 0.01), as shown in Fig. 2D. On the other hand, there was no difference about the number of common colds episodes in the two groups: 3.1 in control group and 2.2 in SLIT group.
SLIT-treated children took significantly less antibiotics (p < 0.05) and fever-reducers (p < 0.01) than control group (Fig. 3).
Th2-dependent inflammation is the hallmark of AR. Allergic inflammation promotes frequent RI episodes. Previously, it has been evidenced that allergic patients have a two-fold increase of RI risk, and duration almost 3 weeks longer of the symptoms than in nonallergic subjects [16]. In addition, it has been demonstrated that rhinovirus-induced infection in atopic subjects heightened susceptibility to the detrimental effects of colds both concerning immunological and clinical aspects [17]. Another study reported that atopic asthmatics suffer from more frequent lower-respiratory-tract infections and have more severe and persistent lower-respiratory-tract symptoms than normal subjects [18]. Thus, a relevant link between RI and AR exists as underlined by several studies [1920212223242526]
Allergen-specific immunotherapy exerts profound effects on immune response, mainly concerning the balance between Th1 and Th2 cells. Particularly, immunotherapy induces an increased IFN-γ production [27]. Therefore, this study aimed at evaluating whether high-dose SLIT may affect RI in children with AR due to HDM sensitization.
Effectively, SLIT-treated patients showed a significant reduction of the total number of RI, associated with diminished use of both antibiotics and fever-reducers in comparison with drug-treated patients. A possible explanation of this relevant effect might be due to the modulation of Th2-polarized immune response in SLIT-treated patients. Indeed, it has been evidenced that SLIT was able of both increasing IFN-γ production and reducing allergic inflammation, assessed by the biomarker soluble HLA-G [28].
The present study confirms a previous multicentre real-life study that evidenced the SLIT ability in exerting "extra antiallergic" effects, mainly concerning RI [12]. Therefore, there is evidence that SLIT is an effective a safe route of AIT [2930] and may have additional activity as provided by preliminary studies, including this preliminary experience.
However, the present study should be considered preliminary because it has some main limitations: it was an open study, recruiting a relatively restricted number of patients; cytokines, chemokines, and mediators, including adhesion molecules, were not evaluated; the SLIT treatment duration was short (6 months) as well as the clinical observation period was short. We decided to design this short course because it is well known that AIT is a long-term treatment, but this involves a relevant drawback: an inadequate adherence to AIT. Thus, the perception of achieving clinically relevant outcome, such an impact on RI, could reinforce the awareness of AIT efficacy. We have to consider another important limitation: the absence of cultural, viral or bacterial, determination. In addition, as RI are more common in younger children, such as from 3 to 6 years old, the present study in children aged 7 onward gives preliminary and partial information. Therefore, this preliminary experience should be confirmed by controlled and lab-based trials recruiting larger cohorts, mainly enrolling younger children (<6 years) and considering longer SLIT treatment and observation time.
Additionally, it is to consider that also omalizumab administration was able to eliminate spring and fall asthma exacerbations [31], which are primarily caused by viral RI [32].
In conclusion, AR should be adequately treated, mainly concerning the comorbidities, including RI, as its impact on social and economic aspects is relevant. This preliminary study might suggest that also a short course (6 months) of high-dose SLIT, titrated in µg of major allergens, could reduce RI in allergic children.
Figures and Tables
 | Fig. 1Total number of respiratory infections in the control group and in children treated with allergen immunotherapy (AIT). |
 | Fig. 2(A) Number of pharyngotonsillitis episodes in control group and allergen immunotherapy (AIT) group; (B) Number of bronchitis episodes in control group and AIT group; (C) Number of patients with unmodified, improved, or worsened snoring in control group and AIT group; (D) Number of patients with fever in control group and AIT group. |
References
1. Bousquet J, Khaltaev N, Cruz AA, Denburg J, Fokkens WJ, Togias A, Zuberbier T, Baena-Cagnani CE, Canonica GW, van Weel C, Agache I, Aït-Khaled N, Bachert C, Blaiss MS, Bonini S, Boulet LP, Bousquet PJ, Camargos P, Carlsen KH, Chen Y, Custovic A, Dahl R, Demoly P, Douagui H, Durham SR, van Wijk RG, Kalayci O, Kaliner MA, Kim YY, Kowalski ML, Kuna P, Le LT, Lemiere C, Li J, Lockey RF, Mavale-Manuel S, Meltzer EO, Mohammad Y, Mullol J, Naclerio R, O'Hehir RE, Ohta K, Ouedraogo S, Palkonen S, Papadopoulos N, Passalacqua G, Pawankar R, Popov TA, Rabe KF, Rosado-Pinto J, Scadding GK, Simons FE, Toskala E, Valovirta E, van Cauwenberge P, Wang DY, Wickman M, Yawn BP, Yorgancioglu A, Yusuf OM, Zar H, Annesi-Maesano I, Bateman ED, Ben Kheder A, Boakye DA, Bouchard J, Burney P, Busse WW, Chan-Yeung M, Chavannes NH, Chuchalin A, Dolen WK, Emuzyte R, Grouse L, Humbert M, Jackson C, Johnston SL, Keith PK, Kemp JP, Klossek JM, Larenas-Linnemann D, Lipworth B, Malo JL, Marshall GD, Naspitz C, Nekam K, Niggemann B, Nizankowska-Mogilnicka E, Okamoto Y, Orru MP, Potter P, Price D, Stoloff SW, Vandenplas O, Viegi G, Williams D. World Health Organization. GA(2)LEN. AllerGen. Allergic Rhinitis and its Impact on Asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen). Allergy. 2008; 63:Suppl 86. 8–160.
2. Miraglia Del Giudice M, Marseglia A, Leonardi S, La Rosa M, Salpietro C, Brunese FP, Arrigo T, Perrone L. Allergic rhinitis and quality of life in children. Int J Immunopathol Pharmacol. 2011; 24:4 Suppl. 25–28.

3. Ciprandi G, Tosca MA, Fasce L. Allergic children have more numerous and severe respiratory infections than non-allergic children. Pediatr Allergy Immunol. 2006; 17:389–391.

4. Fenoglio D, Ferrera A, Ferrera F, Sormani MP, Di Gioacchino M, Ciprandi G. Patients with allergic rhinitis show an allergen-specific interferon-gamma defect. Eur J Inflamm. 2008; 6:87–91.

5. Ciprandi G, Buscaglia S, Pesce G, Pronzato C, Ricca V, Parmiani S, Bagnasco M, Canonica GW. Minimal persistent inflammation is present at mucosal level in patients with asymptomatic rhinitis and mite allergy. J Allergy Clin Immunol. 1995; 96(6 Pt 1):971–979.

6. Gelardi M, Peroni DG, Incorvaia C, Quaranta N, De Luca C, Barberi S, Dell'albani I, Landi M, Frati F, de Beaumont O. Seasonal changes in nasal cytology in mite-allergic patients. J Inflamm Res. 2014; 7:39–44.
7. Yilmaz O, Bakirtas A, Ertoy Karagol HI, Topal E, Demirsoy MS. Allergic rhinitis may impact the recovery of pulmonary function tests after moderate/severe asthma exacerbation in children. Allergy. 2014; 69:652–657.

8. Szefler SJ. Advances in pediatric asthma in 2013: coordinating asthma care. J Allergy Clin Immunol. 2014; 133:654–661.

9. Tantilipikorn P. The relationship between allergic rhinitis and viral infections. Curr Opin Otolaryngol Head Neck Surg. 2014; 22:249–252.

10. Linkov G, Toskala E. Sublingual immunotherapy: what we can learn from the European experience. Curr Opin Otolaryngol Head Neck Surg. 2014; 22:208–210.
11. Ciprandi G, Fenoglio D, Ferrera F, De Amici M, Marseglia G. ELISPOT and ELISA assessment of interferon-gamma after sublingual immunotherapy. Eur J Inflamm. 2010; 8:31–35.

12. Ciprandi G, Incorvaia C, Dell'Albani I, Di Cara G, Barberi S, Puccinelli P, Frati F. RINOBIT Study Group. Allergen immunotherapy may exert an extra-anti-allergic activity in children. J Biol Regul Homeost Agents. 2013; 27:1053–1057.
13. Canonica GW, Cox L, Pawankar R, Baena-Cagnani CE, Blaiss M, Bonini S, Bousquet J, Calderón M, Compalati E, Durham SR, van Wijk RG, Larenas-Linnemann D, Nelson H, Passalacqua G, Pfaar O, Rosário N, Ryan D, Rosenwasser L, Schmid-Grendelmeier P, Senna G, Valovirta E, Van Bever H, Vichyanond P, Wahn U, Yusuf O. Sublingual immunotherapy: World Allergy Organization position paper 2013 update. World Allergy Organ J. 2014; 7:6.

14. Michaud B, Gouvis-Echraghi R, Candon S, Couderc R, Jais JP, Bach JF, Chatenoud L, Just J. Quantification of circulating house dust mite-specific IL-4- and IL-13-secreting T cells correlates with rhinitis severity in asthmatic children and varies with the seasons. Clin Exp Allergy. 2014; 44:222–230.

15. Varricchio A, Capasso M, Di Gioacchino M, Ciprandi G. Inhaled thiamphenicol and acetylcysteine in children with acute bacterial rhinopharyngitis. Int J Immunopathol Pharmacol. 2008; 21:625–629.
16. Cirillo I, Marseglia G, Klersy C, Ciprandi G. Allergic patients have more numerous and prolonged respiratory infections than nonallergic subjects. Allergy. 2007; 62:1087–1090.

17. Bardin PG, Fraenkel DJ, Sanderson G, Dorward M, Lau LC, Johnston SL, Holgate ST. Amplified rhinovirus colds in atopic subjects. Clin Exp Allergy. 1994; 24:457–464.

18. Corne JM, Marshall C, Smith S, Schreiber J, Sanderson G, Holgate ST, Johnston SL. Frequency, severity, and duration of rhinovirus infections in asthmatic and non-asthmatic individuals: a longitudinal cohort study. Lancet. 2002; 359:831–834.

19. Kusel MM, Kebadze T, Johnston SL, Holt PG, Sly PD. Febrile respiratory illnesses in infancy and atopy are risk factors for persistent asthma and wheeze. Eur Respir J. 2012; 39:876–882.

21. Kim JH, Moon BJ, Gong CH, Kim NH, Jang YJ. Detection of respiratory viruses in adult patients with perennial allergic rhinitis. Ann Allergy Asthma Immunol. 2013; 111:508–511.

22. Santillan Salas CF, Mehra S, Pardo Crespo MR, Juhn YJ. Atopic conditions other than asthma and risk of the 2009 novel H1N1 infection in children: a case-control study. Allergy Asthma Proc. 2013; 34:459–466.

23. Rantala A, Jaakkola JJ, Jaakkola MS. Respiratory infections in adults with atopic disease and IgE antibodies to common aeroallergens. PLoS One. 2013; 8:e68582.

24. del Giudice MM, Leonardi S, Ciprandi G, Galdo F, Gubitosi A, La Rosa M, Salpietro C, Marseglia G, Perrone L. Probiotics in childhood: allergic illness and respiratory infections. J Clin Gastroenterol. 2012; 46:S69–S72.
25. Sedaghat AR, Gray ST, Wilke CO, Caradonna DS. Risk factors for development of chronic rhinosinusitis in patients with allergic rhinitis. Int Forum Allergy Rhinol. 2012; 2:370–375.

26. Veling MC. The role of allergy in pediatric rhinosinusitis. Curr Opin Otolaryngol Head Neck Surg. 2013; 21:271–276.

27. Cosmi L, Santarlasci V, Angeli R, Liotta F, Maggi L, Frosali F, Rossi O, Falagiani P, Riva G, Romagnani S, Annunziato F, Maggi E. Sublingual immunotherapy with Dermatophagoides monomeric allergoid down-regulates allergen-specific immunoglobulin E and increases both interferon-gamma- and interleukin-10-production. Clin Exp Allergy. 2006; 36:261–272.

28. Ciprandi G, Continia P, Fenoglio D, Sormani MP, Negrini S, Puppo F, Indiveri F. Relationship between soluble HLA-G and HLA-A,-B,-C serum levels, and interferon-gamma production after sublingual immunotherapy in patients with allergic rhinitis. Hum Immunol. 2008; 69:409–413.
29. Cox L. Sublingual immunotherapy for aeroallergens: status in the United States. Allergy Asthma Proc. 2014; 35:34–42.

30. Pajno GB, Caminiti L, Passalacqua G. Changing the route of immunotherapy administration: an 18-year survey in pediatric patients with allergic rhinitis and asthma. Allergy Asthma Proc. 2013; 34:523–526.

31. Busse WW, Morgan WJ, Gergen PJ, Mitchell HE, Gern JE, Liu AH, Gruchalla RS, Kattan M, Teach SJ, Pongracic JA, Chmiel JF, Steinbach SF, Calatroni A, Togias A, Thompson KM, Szefler SJ, Sorkness CA. Randomized trial of omalizumab (anti-IgE) for asthma in inner-city children. N Engl J Med. 2011; 364:1005–1015.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download