Abstract
Eosinophilic myocarditis is a condition resulting from various eosinophilic diseases, including helminth infection, drug hypersensitivity, systemic vasculitis or idiopathic hypereosinophilic syndromes. Clinical manifestations of eosinophilic myocarditis may vary from early necrosis to endomyocardial fibrosis. Eosinophilic myocarditis is one of the most fatal complications of hypereosinophilia. However, eosinophilic myocarditis has been rarely reported in the literature, particularly in Asia Pacific regions, reflecting the under-recognition of the disease among clinicians. Early recognition is crucial for improving clinical outcomes of eosinophilic myocarditis. Early administration of systemic corticosteroid is necessary in eosinophilic myocarditis regardless of underlying causes, as delayed treatment may result in fatal outcomes. In addition, differential diagnoses of underlying causes for eosinophilia are necessary to improve long-term outcomes.
Eosinophilic myocarditis is a condition resulting from various eosinophilic diseases, including helminth infection, drug hypersensitivity, systemic vasculitis or idiopathic hypereosinophilic syndromes (HES). Clinical manifestations of eosinophilic myocarditis may vary from early necrosis to endomyocardial fibrosis. Eosinophilic myocarditis is one of the most fatal complications of hypereosinophilia [1]. However, eosinophilic myocarditis has been rarely reported in the literature, particularly in Asia Pacific regions, reflecting the under-recognition of the disease among clinicians. In this case report, we present four cases of eosinophilic myocarditis from a single center, along with literature review.
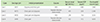
A 21-year-old man was referred to hospital due to recent dyspnea and chest pain for 2 weeks. He had a previous history of atopic dermatitis during infancy, but did not take any recent medications. He denied ingestion of any raw meat, freshwater fish, or liver. He was acute looking, and had bilateral crackles and jugular venous engorgement. Blood pressure (BP) was 84/53 mmHg, pulse rate (PR) was 104/min, respiratory rate (RR) was 16-22/min, body temperature (BT) was 37.2℃. Initial blood tests revealed elevated cardiac enzymes (creatine kinase-myoglobin [CK-MB], 10.5 g/mL [normal range, 0-2.8 ng/mL], and troponin I, 0.09 ng/mL [normal range, 0-0.045 ng/mL]) and brain natriuretic peptide (BNP, 2,824 pg/mL [normal range, 0-88 pg/mL]). Initial emergent complete blood count (CBC) showed blood eosinophil count was within normal range (495/µL) with marked leukocytosis (21,500/µL). However, revealed persistent eosinophilia (810/µL on day 3; 1,485/µL on day 5; 1,960/µL on day 6). Coronary angiography was unremarkable, and transthoracic echocardiography revealed biventricular dysfunction with decreased ejection fraction (EF) of 35%-40%, increased left ventricle (LV) wall thickness, and dilated LV (LV end diastolic diameter, 58 mm). Then initial presumptive diagnosis was made as acute viral myocarditis. However, as blood hypereosinophilia was detected, eosinophilic myocarditis was suspected. Endomyocardial biopsy confirmed the diagnosis, demonstrating myocardial disarray, and diffuse eosinophilic infiltration in myocardial tissues (Fig. 1). Serum total IgE was 214 U/mL (normal range, 0-100 U/mL) and eosinophil cationic protein (ECP) levels were >200 µg/L (normal range, 2-18 µg/L). Antineutrophilic cytoplasmic antibody was negative (Table 1). PDGFRβ(5q33) and CHIC2 del(4)(q12q12) fluorescence in situ hybridization were negative. Thus, intravenous prednisolone 60 mg was started, and blood eosinophil counts and dyspnea began to improve. In a month, he discharged with full recovery in LV functions.
A 72-year-old man visited the emergency department for sudden chest pain and dyspnea. He often consumed raw cow liver. He was diagnosed as asthma several decades ago, but had no asthma symptoms for recent years. The vital signs were BP 138/78 mmHg, PR 69/min, RR 20/min, BT 36.1℃. Initial laboratory investigations revealed elevated cardiac enzyme (CK-MB, 148/µL; troponin I, 0.863/µL; BNP, 1,688 pg/mL; and eosinophilia, 2,340/µL). Serum total IgE level was 419 IU/mL, and ECP level was 20.9 µg/L. Coronary angiography was unremarkable. Echocardiogram revealed concentric left ventricular hypertrophy (LVH) with preserved LV systolic function but whole apex akinesia and pericardial effusion. He underwent cardiac magnetic resonance imaging (MRI), which showed LVH with dysfunction and akinesia at apical global walls. As he had a recent history of raw cow liver consumption, we initiated albendazole and systemic steroid (oral prednisolone 30 mg). Toxocara canis larva excretory-secretory antigen-specific IgG using an enzyme-linked immunosorbent assay kit (TES-ELISA; Bordier Affinity Products SA, Crissier, Switzerland) showed high titer (2.674; cutoff, 1.052). He got recovered his cardiac functions, and now he is free of symptoms.
A 33-year-old man was admitted for sudden chest pain and progressive dyspnea. His previous medical history was unremarkable. However, his initial BP was 90/66 mmHg, and both jugular veins were engorged. Chest x-rays showed enlarged cardiac border suggestive of pericardial effusion, and electrocardiogram (ECG) showed nonspecific T wave and ST changes on inferior and anterolateral leads. The laboratory finding revealed elevated cardiac enzymes (CK-MB, 14.2/µL; troponin I, 7.12/µL) and blood hypereosinophilia (3,535/µL). Serum total IgE level was 218 IU/mL, and ECP level was 75.6 µg/L.
Emergent coronary angiography was performed but demonstrated normal coronary arteries. Echocardiography showed lower normal LVEF (56%) with increased LV wall thickness and base to apical septal and inferior wall akinesia. Systolic BP was dropped, less than 60 mmHg. He was then started with methylprednisolone 60 mg three times a day and intravenous immunoglobulin 2 g/kg continuous infusion for 3 consecutive days with intra-aortic balloon pump support. He responded dramatically to the treatments, and rapidly recovered from cardiogenic shock state. He was negative for all serologic tests including viruses and parasites, culture study, and stool exams.
Since there was no evidence of eosinophilia caused from parasite infection, drug hypersensitivity, vasculitis, or malignancy, he was diagnosed as idiopathic HES and related eosinophilic myocarditis. He received systemic corticosteroid therapy, and fully recovered from cardiac dysfunction in a month.
A 45-year-old male was admitted for acute chest pain. He denied any history of significant medical illness except dyslipidemia. About 40 minutes after his arrival, the vital signs became BP 90/71 mmHg, PR 105/min, RR 29/min, BT 36.5℃. Baseline laboratory tests revealed elevated prohormone of brain natriuretic peptide level (12,361.6 pg/mL), and elevated cardiac enzymes (CK, 311/µL; CK-MB, 12.4/µL; troponin I, 5.99/µL) and ECG showed sinus tachycardia and low voltage with no definite ST change. Non-ST elevation myocardial infarction was considered as a differential diagnosis. However, as elevated blood eosinophil counts (4,453/µL) was noted and the echocardiography revealed increased LV wall thickness, edematous LV wall and severe hypokinesia at mid posterolateral, midinferior, midanterior wall, low normal LV systolic function, small amount of pericardial effusion, eosinophilic myocarditis was considered as the diagnosis. In cardiac MRI, multifocal patchy delayed enhancement of epimyocardium not following vascular territory was found. In computed tomography, multifocal ill-defined ground glass lesions in both upper lungs suggesting nonspecific inflammatory lesions, probably related with eosinophilic infiltration and small low attenuated lesions with fuzzy surrounding enhancement suggesting focal eosinophilic infiltration were found in S4 and S5 of liver. Serum total IgE level was 532 IU/mL and ECP level was 57.2 µg/L. Toxocariasis canis ELISA was positive (1.975; cutoff, 0.999). He was treated with methylprednisolone pulse therapy for cardiogenic shock with pulmonary edema resulting from eosinophilic myocarditis. In addition, Albendazole was given. He recovered from cardiogenic shock, and later from cardiac dysfunction. He completely recovered for more than 4 months now.
Eosinophilic myocarditis poses a considerable morbidity and mortality, resulting from various conditions that cause eosinophilia. Proportion of eosinophilic myocarditis among myocarditis remains unclear, but is suggested to be greater than previously supposed; eosinophilic myocarditis was observed in 0.5% of unselected autopsy cases and up to 20% among the heart transplant recipients secondary to drug-induced hypersensitivity [2]. Moreover, eosinophilic myocarditis is a cause of mortality among patients with HES (48% to 75%) [3, 4]. If untreated, eosinophilic myocarditis leads to the formation of mural thrombus and scarring on myocytes; progressive eosinophilia leads to endomyocardial fibrosis and restrictive cardiomyopathy in the advanced stage [1]. Therefore, early suspicion and diagnosis of eosinophilic myocarditis is mandatory.
Eosinophilic myocarditis can be categorized into several distinct forms. First, Drug hypersensitivity has been described as one of the most common causes [5]. In general, frequently implicated drugs were methyldopa, hydrochlorothiazide, ampicillin, furosemide, digoxin, tetracycline, aminophylline, phenytoin, benzodiazepines, and tricyclic antidepressants [6]. Second, eosinophilic myocarditis can be associated with systemic eosinophilia such as CSS [7, 8]. Third, eosinophilic myocarditis also results from idiopathic HES. HES is a heterogeneous collection of disorders marked by eosinophilia, multiorgan involvement and must be distinguished from other etiologies as the approach to therapy differ. The FIP1L1-PDGFRA gene rearrangement is a recently discovered clonal abnormality and it is a relatively infrequent but treatment-relevant mutation in primary HES [9]. Lastly, eosinophilic myocarditis could be triggered by parasite infection, especially Toxocariasis. Toxocariasis is the most common helminthiasis in industrialized Asian countries, including Korea [10, 11]. As eosinophilic myocarditis may occur in various disease conditions, they need to be taken into consideration for differential diagnoses.
As endomyocardial biopsy is the gold standard test but not always possible, the diagnoses of eosinophilic myocarditis may often be challenged. However, underdiagnosis of eosinophilic myocarditis may result in fatal outcomes such as heart failure, arrhythmias, or sudden death. The diagnostic criteria proposed by the Japanese Circulation Society Task Force may be practically useful for early recognition and treatment; essential diagnostic features include blood eosinophilia >500 µL, cardiac symptoms, elevated cardiac enzymes, ECG changes, and abnormal echocardiography, in the setting of unremarkable coronary angiography [12].
Peripheral blood eosinophilia is one of the diagnostic criteria and important clues for early suspicion of eosinophilic myocarditis, but it is not always correlated with tissue damages [1]. In this regard, serum ECP levels have been suggested as a marker for eosinophil-induced organ damages including heart [13]. All of four cases revealed elevated serum ECP during early stages of eosinophilic myocarditis.
Systemic corticosteroid is the mainstay of treatment for reducing eosinophil-induced organ damages in patients with eosinophilic myocarditis. Also it is important to identify any underlying conditions, as it relates to specific treatment for the conditions, such as parasite infection, drug hypersensitivity, or HES. In cases with refractoriness to corticosteroid therapy, Aggarwal et al. [14] proposed the utility of adjunct azathioprine (2 mg/kg) in a patient who presented eosinophilic myocarditis with cardiogenic shock. Imatinib (Gleevec, Novartis, Basel, Switzerland) has also been shown to have efficacy in patients with HES with FIP1L1-PDGFRa mutation [9].
In conclusions, early recognition is crucial for improving clinical outcomes of eosinophilic myocarditis. Early administration of systemic corticosteroid is necessary in eosinophilic myocarditis regardless of underlying causes, as delayed treatment may result in fatal outcomes. In addition, differential diagnoses of underlying causes for eosinophilia are necessary to improve longterm outcomes.
Figures and Tables
References
3. Al Ali AM, Straatman LP, Allard MF, Ignaszewski AP. Eosinophilic myocarditis: case series and review of literature. Can J Cardiol. 2006; 22:1233–1237.

4. Assa'ad AH, Spicer RL, Nelson DP, Zimmermann N, Rothenberg ME. Hypereosinophilic syndromes. Chem Immunol. 2000; 76:208–229.
5. Amini R, Nielsen C. Eosinophilic myocarditis mimicking acute coronary syndrome secondary to idiopathic hypereosinophilic syndrome: a case report. J Med Case Rep. 2010; 4:40.

6. Burke AP, Saenger J, Mullick F, Virmani R. Hypersensitivity myocarditis. Arch Pathol Lab Med. 1991; 115:764–769.
7. Chang YS, Son JW, Lee SR, Park JK, Cho SH, Min KU, Kim YY. Are Churg-Strauss syndrome and idiopathic hypereosinophilic syndrome in the same spectrum?: a case with overlapping features. J Asthma Allergy Clin Immunol. 1999; 19:208–218.
8. Churg A. Recent advances in the diagnosis of Churg-Strauss syndrome. Mod Pathol. 2001; 14:1284–1293.

9. Cools J, DeAngelo DJ, Gotlib J, Stover EH, Legare RD, Cortes J, Kutok J, Clark J, Galinsky I, Griffin JD, Cross NC, Tefferi A, Malone J, Alam R, Schrier SL, Schmid J, Rose M, Vandenberghe P, Verhoef G, Boogaerts M, Wlodarska I, Kantarjian H, Marynen P, Coutre SE, Stone R, Gilliland DG. A tyrosine kinase created by fusion of the PDGFRA and FIP1L1 genes as a therapeutic target of imatinib in idiopathic hypereosinophilic syndrome. N Engl J Med. 2003; 348:1201–1214.
10. Park HY, Lee SU, Huh S, Kong Y, Magnaval JF. A seroepidemiological survey for toxocariasis in apparently healthy residents in Gangwon-do, Korea. Korean J Parasitol. 2002; 40:113–117.

11. Kang SY, Kang MK, Kim MY, Lee SY, Kim TW, Lee SH, Kim SH, Kang HR, Park HW, Chang YS, Kim SS, Cho SH, Min KU. A case of severe hypereosinophilia caused by toxocara infection after ingestion of raw ostrich liver. Korean J Asthma Allergy Clin Immunol. 2011; 31:144–147.
12. Japanese Circulation Society Task Force Committee on Acute and Chronic Myocarditis. Guidelines for diagnosis and treatment of myocarditis (JCS 2009) [Internet]. Tokyo: Japanese Circulation Society;cited 2015 Mar 10. Available from: http://www.j-circ.or.jp/guideline/pdf/JCS2009_izumi_h.pdf.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download