1. Vanker A, Rhode D. Human immunodeficiency virus and allergic disease. Curr Allergy Clin Immunol. 2009; 22:168–172.
2. Davis CM, Shearer WT. Diagnosis and management of HIV drug hypersensitivity. J Allergy Clin Immunol. 2008; 121:826–832.e5. PMID:
18190954.

3. Todd G. Adverse cutaneous drug eruptions and HIV: a clinician's global perspective. Dermatol Clin. 2006; 24:459–472. PMID:
17010776.

4. Chaponda M, Pirmohamed M. Hypersensitivity reactions to HIV therapy. Br J Clin Pharmacol. 2011; 71:659–671. PMID:
21480946.

5. Bayard PJ, Berger TG, Jacobson MA. Drug hypersensitivity reactions and human immunodeficiency virus disease. J Acquir Immune Defic Syndr. 1992; 5:1237–1257. PMID:
1453334.

6. Temesgen Z, Beri G. HIV and drug allergy. Immunol Allergy Clin North Am. 2004; 24:521–531. PMID:
15242725.

7. Coopman SA, Johnson RA, Platt R, Stern RS. Cutaneous disease and drug reactions in HIV infection. N Engl J Med. 1993; 328:1670–1674. PMID:
8487826.

8. Khan DA, Solensky R. Drug allergy. J Allergy Clin Immunol. 2010; 125(2 Suppl 2):S126–S137. PMID:
20176256.

9. Carr A, Vasak E, Munro V, Penny R, Cooper DA. Immunohistological assessment of cutaneous drug hypersensitivity in patients with HIV infection. Clin Exp Immunol. 1994; 97:260–265. PMID:
8050175.

10. Grimwade K, Swingler G. Cotrimoxazole prophylaxis for opportunistic infections in adults with HIV. Cochrane Database Syst Rev. 2003; (3):CD003108. PMID:
12917946.

11. Grimwade K, Swingler G. Cotrimoxazole prophylaxis for opportunistic infections in children with HIV infection. Cochrane Database Syst Rev. 2003; (2):CD003508. PMID:
12804472.

12. Panel on Opportunistic Infections in HIV-Infected Adults and Adolescents. Guidelines for the prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America [Internet]. Rockbille (MD): AIDS info;c2014. updated 2014 Jan 17. cited 2014 Jan 1. Available from:
http://aidsinfo.nih.gov/contentfiles/lvguidelines/Adult_OI.pdf.
13. Chantachaeng W, Chularojanamontri L, Kulthanan K, Jongjarearnprasert K, Dhana N. Cutaneous adverse reactions to sulfonamide antibiotics. Asian Pac J Allergy Immunol. 2011; 29:284–289. PMID:
22053600.
14. Wang D, Curtis A, Papp AC, Koletar SL, Para MF. Polymorphism in glutamate cysteine ligase catalytic subunit (GCLC) is associated with sulfamethoxazole-induced hypersensitivity in HIV/AIDS patients. BMC Med Genomics. 2012; 5:32. PMID:
22824134.

15. Walmsley SL, Khorasheh S, Singer J, Djurdjev O. Canadian HIV Trials Network 057 Study Group. A randomized trial of N-acetylcysteine for prevention of trimethoprim-sulfamethoxazole hypersensitivity reactions in Pneumocystis carinii pneumonia prophylaxis (CTN 057). J Acquir Immune Defic Syndr Hum Retrovirol. 1998; 19:498–505. PMID:
9859964.

16. Moreno Escobosa MC, Cruz Granados S, Moya Quesada MC, Amat Lopez J. Enanthema and fixed drug eruption caused by trimethoprim. J Investig Allergol Clin Immunol. 2009; 19:249–250.
17. Lin D, Li WK, Rieder MJ. Cotrimoxazole for prophylaxis or treatment of opportunistic infections of HIV/AIDS in patients with previous history of hypersensitivity to cotrimoxazole. Cochrane Database Syst Rev. 2007; (2):CD005646. PMID:
17443608.

18. Schnyder B, Pichler WJ. Allergy to sulfonamides. J Allergy Clin Immunol. 2013; 131:256–257.e1-5. PMID:
23265699.

19. Zhou J, Elliott J, Li PC, Lim PL, Kiertiburanakul S, Kumarasamy N, Merati TP, Pujari S, Chen YM, Phanuphak P, Vonthanak S, Sirisanthana T, Sungkanuparph S, Lee CK, Kamarulzaman A, Oka S, Zhang F, Tau G, Ditangco R. Risk and prognostic significance of tuberculosis in patients from The TREAT Asia HIV Observational Database. BMC Infect Dis. 2009; 9:46. PMID:
19383122.

20. Lawn SD, Harries AD, Williams BG, Chaisson RE, Losina E, De Cock KM, Wood R. Antiretroviral therapy and the control of HIV-associated tuberculosis. Will ART do it? Int J Tuberc Lung Dis. 2011; 15:571–581. PMID:
21756508.
21. Naidoo K, Abdool Karim Q, Bhushan A, Naidoo K, Yende-Zuma N, McHunu PK, Frohlich J, Karim F, Upfold M, Kocheleff P, Abdool Karim SS. High rates of Tuberculosis in patients accessing HAART in rural South Africa. J Acquir Immune Defic Syndr. 2013; 11. 19. [Epub]. Available from:
http://dx.doi.org/10.1097/QAI.0000000000000060.

22. Akolo C, Adetifa I, Shepperd S, Volmink J. Treatment of latent tuberculosis infection in HIV infected persons. Cochrane Database Syst Rev. 2010; (1):CD000171. PMID:
20091503.

23. Golub JE, Pronyk P, Mohapi L, Thsabangu N, Moshabela M, Struthers H, Gray GE, McIntyre JA, Chaisson RE, Martinson NA. Isoniazid preventive therapy, HAART and tuberculosis risk in HIV-infected adults in South Africa: a prospective cohort. AIDS. 2009; 23:631–636. PMID:
19525621.

24. Grant AD, Mngadi KT, van Halsema CL, Luttig MM, Fielding KL, Churchyard GJ. Adverse events with isoniazid preventive therapy: experience from a large trial. AIDS. 2010; 24(Suppl 5):S29–S36. PMID:
21079425.

25. Forget EJ, Menzies D. Adverse reactions to first-line antituberculosis drugs. Expert Opin Drug Saf. 2006; 5:231–249. PMID:
16503745.

26. Nunn P, Kibuga D, Gathua S, Brindle R, Imalingat A, Wasunna K, Lucas S, Gilks C, Omwega M, Were J. Cutaneous hypersensitivity reactions due to thiacetazone in HIV-1 seropositive patients treated for tuberculosis. Lancet. 1991; 337:627–630. PMID:
1705647.

27. Chintu C, Luo C, Bhat G, Raviglione M, DuPont H, Zumla A. Cutaneous hypersensitivity reactions due to thiacetazone in the treatment of tuberculosis in Zambian children infected with HIV-I. Arch Dis Child. 1993; 68:665–668. PMID:
7686737.

28. Nunn P, Gicheha C, Hayes R, Gathua S, Brindle R, Kibuga D, Mutie T, Kamunyi R, Omwega M, Were J. Cross-sectional survey of HIV infection among patients with tuberculosis in Nairobi, Kenya. Tuber Lung Dis. 1992; 73:45–51. PMID:
1381970.

29. Widhani A, Yunihastuti E, Djauzi S. Cutaneous adverse drug reaction among HIV-infected patients starting antituberculosis treatment [abstract WEPE474]. In : 7th IAS Conference on HIV Pathogenesis and Treatment; 2013 Jun 30-Jul 3; Kuala Lumpur, Malaysia. Geneva: International AIDS Society;2013.
30. Thong BY. Clinical applications of drug desensitization in the Asia-Pacific region. Asia Pac Allergy. 2011; 1:2–11. PMID:
22053290.

31. Yee D, Valiquette C, Pelletier M, Parisien I, Rocher I, Menzies D. Incidence of serious side effects from first-line antituberculosis drugs among patients treated for active tuberculosis. Am J Respir Crit Care Med. 2003; 167:1472–1477. PMID:
12569078.

32. Tan WC, Ong CK, Kang SC, Razak MA. Two years review of cutaneous adverse drug reaction from first line anti-tuberculous drugs. Med J Malaysia. 2007; 62:143–146. PMID:
18705448.
33. Yan J, Huang B, Liu G, Wu B, Huang S, Zheng H, Shen J, Lun ZR, Wang Y, Lu F. Meta-analysis of prevention and treatment of toxoplasmic encephalitis in HIV-infected patients. Acta Trop. 2013; 127:236–244. PMID:
23707647.

34. Nissapatorn V, Sawangjaroen N. Parasitic infections in HIV infected individuals: diagnostic & therapeutic challenges. Indian J Med Res. 2011; 134:878–897. PMID:
22310820.
35. Katlama C, De Wit S, O'Doherty E, Van Glabeke M, Clumeck N. Pyrimethamine-clindamycin vs. pyrimethamine-sulfadiazine as acute and long-term therapy for toxoplasmic encephalitis in patients with AIDS. Clin Infect Dis. 1996; 22:268–275. PMID:
8838183.

36. Iaccheri B, Fiore T, Papadaki T, Androudi S, Janjua S, Bhaila I, Stephen Foster C. Adverse drug reactions to treatments for ocular toxoplasmosis: a retrospective chart review. Clin Ther. 2008; 30:2069–2074. PMID:
19108794.

37. Yunihastuti E, Djauzi S. The incidence of drug allergy among HIV infected adults in Jakarta. In : Poster presentation at JACI APAPARI Joint Meeting; 2006 Apr 21-23; Jakarta, Indonesia.
38. Mazur N, Greenberger PA, Regalado J. Clindamycin hypersensitivity appears to be rare. Ann Allergy Asthma Immunol. 1999; 82:443–445. PMID:
10353574.

39. Nakamura Y, Watamatsu K, Muto M. Drug-induced hypersensitivity syndrome induced by clindamycin. Acta Derm Venereol. 2013; 93:83–84. PMID:
22855006.

40. Parmar R, Sharma V, Thakkar C, Chaudhary A, Pateliya U, Ninama G, Mistry K, Goswami Y, Kavathia GU, Rajat R. Prevalence of opportunistic fungal infections in HIV positive patients in tertiary care hospital in Rajkot. Nat J Med Res. 2012; 2:463–465.
41. Volberding PA, Greene WC, Lange JMA, Gallant JE, Sewankambo N. Sande's HIV/AIDS medicine: medical management of AIDS 2013. 2nd ed. [Edinburgh]: Elsevier;2013.
42. Su FW, Perumalswami P, Grammer LC. Acute hepatitis and rash to fluconazole. Allergy. 2003; 58:1215–1216. PMID:
14616149.

43. Craig TJ, Peralta F, Boggavarapu J. Desensitization for fluconazole hypersensitivity. J Allergy Clin Immunol. 1996; 98:845–846. PMID:
8876563.

44. Pinto A, Chan RC. Lack of allergic cross-reactivity between fluconazole and voriconazole. Antimicrob Agents Chemother. 2009; 53:1715–1716. PMID:
19164151.

45. Bittleman DB, Stapleton J, Casale TB. Report of successful desensitization to itraconazole. J Allergy Clin Immunol. 1994; 94(2 Pt 1):270–271. PMID:
8064084.

46. Reed JJ, Sweiss K, Muniyappa PK. Posaconazole desensitization protocol. J Allergy Clin Immunol. 2011; 127(2 Suppl):AB244.

47. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents: developed by the HHS panel on antiretroviral guidelines foradults and adolescents - A Working Group of the Office of AIDS Research Advisory Council (OARAC) [Internet]. Rockville (MD): AIDS info;c2014. updated 2014 Jan 17. cited 2014 Jan 1. Available from:
http://aidsinfo.nih.gov/ContentFiles/AdultandAdolescentGL.pdf.
48. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: recommendations for a public health approach [Internet]. Geneva: World Health Organization;c2014. cited 2014 Jan 1. Available from:
http://www.who.int/hiv/pub/guidelines/arv2013/download/en/.
49. Borras-Blasco J, Navarro-Ruiz A, Borras C, Castera E. Adverse cutaneous reactions associated with the newest antiretroviral drugs in patients with human immunodeficiency virus infection. J Antimicrob Chemother. 2008; 62:879–888. PMID:
18653488.

50. Symonds W, Cutrell A, Edwards M, Steel H, Spreen B, Powell G, McGuirk S, Hetherington S. Risk factor analysis of hypersensitivity reactions to abacavir. Clin Ther. 2002; 24:565–573. PMID:
12017401.

51. Easterbrook PJ, Waters A, Murad S, Ives N, Taylor C, King D, Vyakarnam A, Thorburn D. Epidemiological risk factors for hypersensitivity reactions to abacavir. HIV Med. 2003; 4:321–324. PMID:
14525543.

52. Lucas A, Nolan D, Mallal S. HLA-B*5701 screening for susceptibility to abacavir hypersensitivity. J Antimicrob Chemother. 2007; 59:591–593. PMID:
17317695.

53. Montero M, García-Gibert L, Gimenez-Arnau AM, Knobel H. Toxic epidermal necrolysis associated with abacavir. Enferm Infecc Microbiol Clin. 2005; 23:247. PMID:
15826554.
54. Escaut L, Liotier JY, Albengres E, Cheminot N, Vittecoq D. Abacavirrechallenge has to be avoided in case of hypersensitivity reaction. AIDS. 1999; 13:1419–1420. PMID:
10449301.
55. Wit FW, Wood R, Horban A, Beniowski M, Schmidt RE, Gray G, Lazzarin A, Lafeuillade A, Paes D, Carlier H, van Weert L, de Vries C, van Leeuwen R, Lange JM. Prednisolone does not prevent hypersensitivity reactions in antiretroviral drug regimens containing abacavir with or without nevirapine. AIDS. 2001; 15:2423–2429. PMID:
11740193.

56. Mallal S, Phillips E, Carosi G, Molina JM, Workman C, Tomazic J, Jagel-Guedes E, Rugina S, Kozyrev O, Cid JF, Hay P, Nolan D, Hughes S, Hughes A, Ryan S, Fitch N, Thorborn D, Benbow A. PREDICT-1 Study Team. HLA-B*5701 screening for hypersensitivity to abacavir. N Engl J Med. 2008; 358:568–579. PMID:
18256392.

57. Rauch A, Nolan D, Martin A, McKinnon E, Almeida C, Mallal S. Prospective genetic screening decreases the incidence of abacavir hypersensitivity reactions in the Western Australian HIV cohort study. Clin Infect Dis. 2006; 43:99–102. PMID:
16758424.

58. Duque S, de la Puente J, Rodríguez F, Fernandez Pellon L, Maquiera E, Jerez J. Zidovudine-related erythroderma and successful desensitization: a case report. J Allergy Clin Immunol. 1996; 98:234–235. PMID:
8765840.
59. Murri R, Antinori A, Camilli G, Zannoni G, Patriarca G. Fatal toxic epidermolysis induced by zidovudine. Clin Infect Dis. 1996; 23:640–641. PMID:
8879796.

60. Product information VIREAD(R) oral tablets, tenofovir disoproxil fumarate oral tablets. Foster City (CA): Gilead Sciences Inc.;2007.
61. Woolley IJ, Veitch AJ, Harangozo CS, Moyle M, Korman TM. Lichenoid drug eruption to tenofovir in an HIV/hepatitis B virus co-infected patient. AIDS. 2004; 18:1857–1858. PMID:
15316351.

62. Lockhart SM, Rathbun RC, Stephens JR, Baker DL, Drevets DA, Greenfield RA, Salvaggio MR, Vincent S. Cutaneous reactions with tenofovir disoproxil fumarate: a report of nine cases. AIDS. 2007; 21:1370–1373. PMID:
17545718.

63. Verma R, Vasudevan B, Shankar S, Pragasam V, Suwal B, Venugopal R. First reported case of tenofovir-induced photoallergic reaction. Indian J Pharmacol. 2012; 44:651–653. PMID:
23112433.

64. Carr A, Cooper DA. Adverse effects of antiretroviral therapy. Lancet. 2000; 356:1423–1430. PMID:
11052597.

65. Montessori V, Press N, Harris M, Akagi L, Montaner JS. Adverse effects of antiretroviral therapy for HIV infection. CMAJ. 2004; 170:229–238. PMID:
14734438.
66. Pollard RB, Robinson P, Dransfield K. Safety profile of nevirapine, a nonnucleoside reverse transcriptase inhibitor for the treatment of human immunodeficiency virus infection. Clin Ther. 1998; 20:1071–1092. PMID:
9916603.

67. Warren KJ, Boxwell DE, Kim NY, Drolet BA. Nevirapine-associated Stevens-Johnson syndrome. Lancet. 1998; 351:567. PMID:
9492778.

68. Wit FW, Kesselring AM, Gras L, Richter C, van der Ende ME, Brinkman K, Lange JM, de Wolf F, Reiss P. Discontinuation of nevirapine because of hypersensitivity reactions in patients with prior treatment experience, compared with treatment-naive patients: the ATHENA cohort study. Clin Infect Dis. 2008; 46:933–940. PMID:
18271750.

69. Centers for Disease Control and Prevention (CDC). Serious adverse events attributed to nevirapine regimens for postexposure prophylaxis after HIV exposures--worldwide, 1997-2000. MMWR Morb Mortal Wkly Rep. 2001; 49:1153–1156. PMID:
11198946.
70. Murphy RL. Defining the toxicity profile of nevirapine and other antiretroviral drugs. J Acquir Immune Defic Syndr. 2003; 34(Suppl 1):S15–S20. PMID:
14562854.

71. Anton P, Soriano V, Jimenez-Nacher I, Rodriguez-Rosado R, Dona MC, Barreiro PM, González-Lahoz J. Incidence of rash and discontinuation of nevirapine using two different escalating initial doses. AIDS. 1999; 13:524–525. PMID:
10197383.

72. Mehta U, Maartens G. Is it safe to switch between efavirenz and nevirapine in the event of toxicity? Lancet Infect Dis. 2007; 7:733–738. PMID:
17961859.

73. Colebunders R, Vanwolleghem T, Meurrens P, Moerman F. Efavirenz-associated Stevens-Johnson syndrome. Infection. 2004; 32:306–307. PMID:
15624898.

74. Clarke S, Harrington P, Barry M, Mulcahy F. The tolerability of efavirenz after nevirapine-related adverse events. Clin Infect Dis. 2000; 31:806–807. PMID:
11017835.

75. Soriano V, Dona C, Barreiro P, Gonzalez-Lahoz J. Is there cross-toxicity between nevirapine and efavirenz in subjects developing rash? AIDS. 2000; 14:1672–1673. PMID:
10983663.

76. Manosuthi W, Thongyen S, Chumpathat N, Muangchana K, Sungkanuparph S. Incidence and risk factors of rash associated with efavirenz in HIV-infected patients with preceding nevirapine-associated rash. HIV Med. 2006; 7:378–382. PMID:
16903982.

77. Laureillard D, Prak N, Fernandez M, Ngeth C, Moeung S, Riel V, Chhneang V, Song S, Quillet C, Piketty C. Efavirenz replacement by immediate full-dose nevirapine is safe in HIV-1-infected patients in Cambodia. HIV Med. 2008; 9:514–518. PMID:
18554312.

78. Schiller DS, Youssef-Bessler M. Etravirine: a second-generation nonnucleoside reverse transcriptase inhibitor (NNRTI) active against NNRTI-resistant strains of HIV. Clin Ther. 2009; 31:692–704. PMID:
19446143.

79. Mills A, Grinsztejn B, Katlama C, Peeters M, Janssen K, Kakuda TN, et al. The incidence of rash observed with the NNRTI etravirine in the Phase III DUET trials using pooled 48-week data [abstract TUPE0059]. In : 17th International AIDS Conference; 2008 Aug 3-8; Mexicocity, Mexico.
80. Cohen CJ, Molina JM, Cahn P, Clotet B, Fourie J, Grinsztejn B, Wu H, Johnson MA, Saag M, Supparatpinyo K, Crauwels H, Lefebvre E, Rimsky LT, Vanveggel S, Williams P, Boven K. ECHO Study Group. Efficacy and safety of rilpivirine (TMC278) versus efavirenz at 48 weeks in treatment-naive HIV-1-infected patients: pooled results from the phase 3 double-blind randomized ECHO and THRIVE Trials. J Acquir Immune Defic Syndr. 2012; 60:33–42. PMID:
22343174.
81. Chapman TM, Plosker GL, Perry CM. Fosamprenavir: a review of its use in the management of antiretroviral therapy-naive patients with HIV infection. Drugs. 2004; 64:2101–2124. PMID:
15341507.
82. Ouagari Z, Tubiana R, Mohand HA, Dominguez S, Duvivier C, Bricaire F, Katlama C, Caumes E. Skin rash associated with atazanavir: report of three cases. AIDS. 2006; 20:1207–1208. PMID:
16691076.

83. Santos JR, Moltó J, Llibre JM, Negredo E, Bravo I, Ornelas A, Clotet B, Paredes R. Antiretroviral simplification with darunavir/ritonavir monotherapy in routine clinical practice: safety, effectiveness, and impact on lipid profile. PLoS One. 2012; 7:e37442. PMID:
22666357.

84. Shahar E, Moar C, Pollack S. Successful desensitization of enfuvirtide-induced skin hypersensitivity reaction. AIDS. 2005; 19:451–452. PMID:
15750403.

85. Walmsley SL, Antela A, Clumeck N, Duiculescu D, Eberhard A, Gutirrrez F, Hocqueloux L, Maggiolo F, Sandkovsky U, Granier C, Pappa K, Wynne B, Min S, Nichols G. SINGLE Investigators. Dolutegravir plus abacavir-lamivudine for the treatment of HIV-1 infection. N Engl J Med. 2013; 369:1807–1818. PMID:
24195548.

86. Shear NH, Milpied B, Bruynzeel DP, Phillips EJ. A review of drug patch testing and implications for HIV clinicians. AIDS. 2008; 22:999–1007. PMID:
18520343.

87. Phillips EJ, Chung WH, Mockenhaupt M, Roujeau JC, Mallal SA. Drug hypersensitivity: pharmacogenetics and clinical syndromes. J Allergy Clin Immunol. 2011; 127(3 Suppl):S60–S66. PMID:
21354501.

88. Cressey TR, Jourdain G, Lallemant MJ, Kunkeaw S, Jackson JB, Musoke P, Capparelli E, Mirochnick M. Persistence of nevirapine exposure during the postpartum period after intrapartum single-dose nevirapine in addition to zidovudine prophylaxis for the prevention of mother-to-child transmission of HIV-1. J Acquir Immune Defic Syndr. 2005; 38:283–288. PMID:
15735445.
89. Ribaudo HJ, Haas DW, Tierney C, Kim RB, Wilkinson GR, Gulick RM, Clifford DB, Marzolini C, Fletcher CV, Tashima KT, Kuritzkes DR, Acosta EP. Adult AIDS Clinical Trials Group Study. Pharmacogenetics of plasma efavirenz exposure after treatment discontinuation: an Adult AIDS Clinical Trials Group Study. Clin Infect Dis. 2006; 42:401–407. PMID:
16392089.

90. McIntyre JA, Hopley M, Moodley D, Eklund M, Gray GE, Hall DB, Robinson P, Mayers D, Martinson NA. Efficacy of short-course AZT plus 3TC to reduce nevirapine resistance in the prevention of mother-to-child HIV transmission: a randomized clinical trial. PLoS Med. 2009; 6:e1000172. PMID:
19859531.

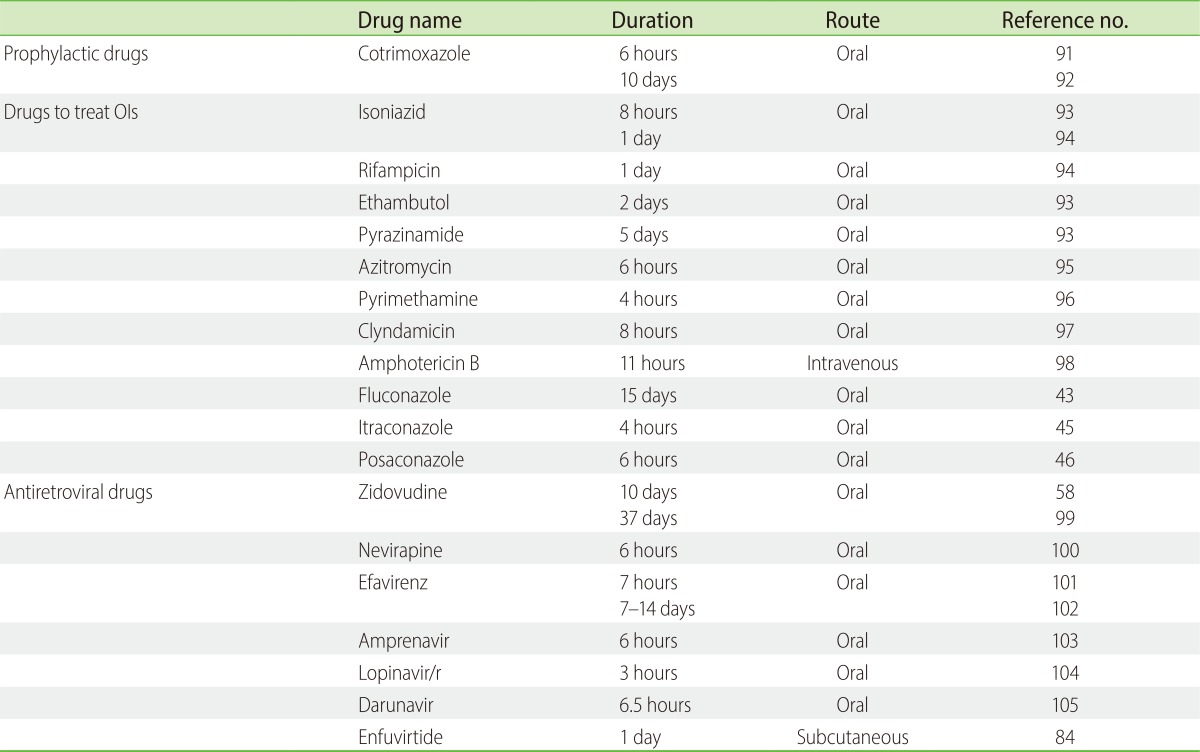
91. Demoly P, Messaad D, Sahla H, Fabre J, Faucherre V, Andre P, Reynes J, Godard P, Bousquet J. Six-hour trimethoprim-sulfamethoxazole-graded challenge in HIV-infected patients. J Allergy Clin Immunol. 1998; 102(6 Pt 1):1033–1036. PMID:
9847446.

92. Patriarca G, Schiavino D, Buonomo A, Aruanno A, Altomonte G, Nucera E. Desensitization to co-trimoxazole in a patient with fixed drug eruption. J Investig Allergol Clin Immunol. 2008; 18:309–311.
93. Rodrigues Carvalho S, Silva I, Leiria-Pinto P, Rosado-Pinto J. Rapid oral tolerance induction to isoniazid and pyrazinamide and controlled administration of ethambutol: clinical case. Allergol Immunopathol (Madr). 2009; 37:336–338. PMID:
19875222.

94. Holland CL, Malasky C, Ogunkoya A, Bielory L. Rapid oral desensitization to isoniazid and rifampin. Chest. 1990; 98:1518–1519. PMID:
2245698.

95. Aberer W, Kranke B. Provocation tests in drug hypersensitivity. Immunol Allergy Clin North Am. 2009; 29:567–584. PMID:
19563998.

96. Gonzalez E, Henriquez A, Losada A, Huertas B, Gonzalez J, Berges P, Alvarez E. Pyrimethamine desensitization in cerebral toxoplasmosis and AIDS. J Allergy Clin Immunol. 2007; 119(1 Suppl):S67.

97. Marcos C, Sopeña B, Luna I, Gonzalez R, de la Fuente J, Martinez-Vazquez C. Clindamycin desensitization in an AIDS patient. AIDS. 1995; 9:1201–1202. PMID:
8519462.

98. Dhindsa-Castanedo L, Narra M. Desensitization to liposomal amphotericin B after anaphylactic reaction. J Allergy Clin Immunol. 2012; 129(2 Suppl):AB105.

99. Carr A, Penny R, Cooper DA. Allergy and desensitization to zidovudine in patients with acquired immunodeficiency syndrome (AIDS). J Allergy Clin Immunol. 1993; 91:683–685. PMID:
8436782.
100. Demoly P, Messaad D, Fabre J, Reynes J, Bousquet J. Nevirapine-induced cutaneous hypersensitivity reactions and successful tolerance induction. J Allergy Clin Immunol. 1999; 104(2 Pt 1):504–505. PMID:
10452781.

101. Khalili H, Farasatinasab M, Hajiabdolbaghi M. Efavirenz severe hypersensitivity reaction: case report and rapid desensitization protocol development. Ann Pharmacother. 2012; 46:e12. PMID:
22535841.

102. Phillips EJ, Kuriakose B, Knowles SR. Efavirenz-induced skin eruption and successful desensitization. Ann Pharmacother. 2002; 36:430–432. PMID:
11895054.

103. Kohli-Pamnani A, Huynh P, Lobo F. Amprenavir-induced maculopapularexanthem followed by desensitization in a patient with late-stage human immunodeficiency virus. Ann Allergy Asthma Immunol. 2006; 96:620–623. PMID:
16680935.
104. Diaz JM, Kopylstova Y, Kaplan B. Successful induction of drug tolerance (IDT aka desensitization) to lopinavir/ritonavir in a patient with multidrug-resistant AIDS and drug hypersensitivity. In : Poster at EAACI-WAO World Allergy and Asthma Congress 2013; 2013 Jun 22-26; Milan, Italy. Poster no. 495.
105. Marcos Bravo MC, Ocampo Hermida A, Martinez Vilela J, Perez Rodriguez MT, Gavilan Montenegro MJ, Arenas Villarroel LJ, Miralles Alvarez C, Rodriguez Dasilva A, Martinez Vazquez C. Hypersensitivity reaction to darunavir and desensitization protocol. J Investig Allergol Clin Immunol. 2009; 19:250–251.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download