Abstract
Radiocontrast media (RCM) is a major cause of drug hypersensitivity reactions as the medical application of RCM is increasing recently. RCM induced hypersensitivity reactions are considered as unpredictable type B reactions. Underlying mechanism of RCM induced hypersensitivity was previously regarded as nonimmunological mechanisms but recent studies suggest that immunological mechanisms could also be involved. As a result, the roles of skin tests and premedication are revisiting. As there has been no report that comprehensively summarized and analyzed the results of the studies on RCM hypersensitivity in the Asia Pacific region, we aimed to review the literatures on hypersensitivity reactions to RCM in terms of prevalence clinical manifestations, diagnostic approach, and preventive measures in the Asia Pacific region.
Radiocontrast media (RCM) is a major cause of drug hypersensitivity reactions as the application of RCM is increasing recently in medicine [1]. Although the incidence of RCM induced hypersensitivity reactions was decreased after high-osmolar contrast agents were replaced by low/iso-osmolar agents, increasing number of diagnostic tests using RCM such as computed tomography makes the hypersensitivity to RCM a big issue [2]. RCM induced hypersensitivity reactions are still considered as unpredictable type B hypersensitivity reactions. Underlying mechanism of RCM induced hypersensitivity was previously regarded as nonimmunological mechanisms but recent evidences suggest that immunological mechanisms could also be involved [3, 4, 5]. As a result, the roles of skin tests and premedication are revisiting. In the Asia Pacific region, several studies on RCM induced hypersensitivity reactions have been published including the prevalence clinical manifestations, diagnostic tests and preventions [4, 6, 7]. However, there has been no report that comprehensively summarized and analyzed the results of the studies on RCM hypersensitivity in the Asia Pacific region.
In this article, we aimed to review the literatures semisystematically on hypersensitivity reactions to RCM in terms of prevalence clinical manifestations, diagnostic approach, and prevention in the Asia Pacific region. Two independent authors searched literatures from MEDLINE, Embase, and KoreaMed to identify relevant publications on RCM hypersensitivity from the Asia Pacific region. Searches were limited to articles published in English or Korean, human studies. Search terms included MeSH headings and text words; (contrast media or contrast), combined with (hypersensitivity, allergic reaction, anaphylaxis).
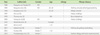
The prevalence of hypersensitivity reactions showed a difference according to the type of RCM and the onset of the reactions (Tables 1, 2). Immediate reactions that occur within an hour after exposure are nonimmunological or immunoglobulin E (IgE)-mediated reactions while delayed reactions, which occur from an hour to 7 days after exposure, are suggested to be type 4 hypersensitivity reactions that mainly mediated by T cells.
There were several studies on the prevalence of the immediate reactions from Korea (3), Japan (3), Australia (1), India (1), Thailand (1), Turkey (1), and Qatar (1) since 1988. The overall prevalence of immediate reactions was 6.4-31.2% with ionic RCM and 0.16-7.7% with nonionic RCM. In 21st century, the overall prevalence was 0.16-2.21% from the studies.
In case of delayed type hypersensitivity reactions, there were studies from Japan (5), Korea (2), Thailand (1), and Turkey (1) since 1982. The overall prevalence was 0.03-16.5% since 1982 in the Asia Pacific region. The overall prevalence was 0.03-1.95% in 21st century.
Immediate reactions are cutaneous (itching and urticaria), respiratory (bronchospasm and dyspnea), or cardiovascular (dizziness and anaphylactic shock). Delayed reactions are usually cutaneous symptoms such as itching, maculopapular exanthema, Stevens-Johnson syndrome, and toxic epidermal necrolysis [2].
Although the prevalence of severe reactions varied depending on the studies, severe life-threatening reactions was 0.04-0.28% [1, 2, 4, 6, 7, 8, 9]. It has also been reported that RCM was the most responsible drug that accounted for 18.0% of in-hospital anaphylaxis in a Korean study conducted in a tertiary hospital [1].
In a large-scale research in 1990, 70% of RCM hypersensitivity reactions occurred within 5 minutes after injection of RCM agents [10]. Another study, which used only iomeprol, reported that 46.4% of reactions were shown within 10 minutes after injection [11]. However, RCM induced anaphylaxis can also occur hours after the exposure [2].
Previous studies reported no significant difference between genders in RCM hypersensitivity reactions [9, 10, 11]. Interestingly, a recent study conducted in Turkey (1,131 subjects), in Australia (29,962 subjects), and Thailand (55,286 subjects) showed that female gender was one of significant risk factors in RCM-induced hypersensitivity reactions [12] (Table 3).
A recent Korean study showed that subjects over 50 years old showed statically significant higher incidence of hypersensitivity (p = 0.037) [7] (Table 3).
However, a Japanese study published in 1990 showed that overall RCM hypersensitivity reactions were most common in the age of 20-29, especially severe in 10 to 19 years old [10]. An Australian study showed that patients under 55 years old had significant risk of the RCM hypersensitivity reactions (odds ratio, 2.46; p = 0.005) [13].
RCM hypersensitivity reactions induced by high-osmolar ionic RCM did not show any difference according to age in Indian population [9].
In a study from Korea [2], computed tomography (CT) was the most common procedure (3.9%) that caused RCM hypersensitivity, followed by angiography (1.1%), magnetic resonance imaging (MRI) (0.8%), and fluoroscopy (0.2%). One case of anaphylaxis occurred during CT angiography.
The use of MRI dye may be safe; however, it can possibly induce anaphylaxis [14]. Thus, physicians should be aware that hypersensitivity reactions can also be caused by MRI dye. In a study from Korea, among the 112 hypersensitivity reactions caused by MRI contrast media, urticaria was the most common symptom observed with 102 cases (91.1%). In addition, respiratory symptoms occurred in 17 cases (15.2%); hypotension in 11 cases including one fatal case (9.8%); angioedema in six cases (5.4%) and other multiple symptoms in 19 cases (17.0%) [14].
Previous history of allergy could increase the risk of hypersensitivity reactions to RCM [10, 11, 15, 16]. Asthma could be related with more severe reactions (Table 3).
In a study in 1988, a group with history of allergy, asthma, urticarial, or other hypersensitivity showed 52% rate of hypersensitivity reactions compared to patients without the allergy history (7.1%) [17]. Especially, asthma has been reported as a risk factor of severe reactions. In another large scaled study [10], asthma had higher incidence of severe RCM hypersensitivity reaction compare to other allergy such as atopy, pollinosis, drug allergy, and food allergy. Similarly, recent study in Thailand [16] presented that although a history of seafood allergy increased overall incidence of RCM hypersensitivity, and that patients with asthma history has more severe reactions.
Delayed reactions to RCM are relatively difficult to be noticed because they may appear few days after injection and could be confused with symptoms induced by other factors. In one study [18], the prevalence of delayed reaction was 12.4% and none of the risk factors, such as patient's gender, age, history of allergy, were related with the prevalence of delayed reaction. The other study suggested female who were over the age of 40 was at risk of drug eruption by nonionic RCM [19]. Since CT exam is performed more often in older patients, 74.1% of all patients were older than 40 years old.
Among 11,121 patients who responded to the questionnaire in a Japanese research [20], 9.5% showed delayed reactions. There were four risk factors of delayed reactions which include no previous history of examinations using contrast media; past adverse reactions caused by contrast media; a history of allergy and a serum creatinine level greater than 2.0 mg/dL.
History taking and physical examination is the main stream in the diagnostic approach. The temporal relationship between the exposure to RCM and the onset of clinical symptom is essential. However, the data for internationally validated laboratory test to detect RCM hypersensitivity has been lacking.
Before current skin test method was widely used [4, 5], researchers tried to predict RCM induced hypersensitivity reactions by injecting a small amount of RCM intravenously before the formal injection [17]. In this study, 48% of pretest positive patients showed hypersensitivity reactions compared to 7.4% of pretest negative group showed only 7.4%. This strong indicator of increased risk of RCM hypersensitivity reaction was not associated with previous RCM exposure history. In an article published in 1991 [22], the characteristics of severe reactions by RCM were evaluated. The value of pretest (injection of small amount of RCM before the procedure) was not sufficient in both ionic and nonionic contrast media, and therefore, the pretest could not predict the risk of severe reaction.
In era of low/iso-osmolar RCM, a study reported that only two among 14 patients with a history of immediate RCM hypersensitivity showed positive skin test in 2011 [16]. Limiting all of the previous reactions to low grade (grade 1 or 2) might have caused low positive rate.
A Korean study was performed to validate the efficacy of RCM skin test to screen RCM hypersensitivity before the administration of RCMs [4]. After 1,048 prescreening skin test, only one showed immediate skin test response (0.09%). Five percent of patients with negative skin test who underwent computed tomography showed immediate reactions. This result suggested that RCM skin test did not have a clinical utility as a screening tool. However, interestingly, the positivity rate of RCM skin test increased as the severity of hypersensitivity reaction higher in patients with RCM hypersensitivity reactions (12.9% in grade I, 25.0% in grade II, 57.1% in grade III). Therefore, the skin test could be useful to identify the causative RCMs in severe hypersensitivity reactions.
Basophil activation test (BAT) could be used as a complementary tool to diagnose RCM hypersensitivity. BAT is a flow cytometry-based cellular assay that measures the activation of basophils upon allergen stimulation using CD63 or CD203c which may detect IgE or non-IgE mediated RCM hypersensitivity [3]. However, the diagnostic value of BAT had not been fully identified. One study performed in Thailand [23], the value of BAT in immediate RCM hypersensitivity was evaluated, and authors identified the activated basophil percentage was significantly higher in patients with previous history of immediate reaction induced by RCM compared with control group. Recently a review article on the value of BAT on RCM hypersensitivity suggested that the sensitivity was 46.2-61.5% and specificity 88.4-100% and that further studies were necessary [3].
Delayed reactions by RCM are usually diagnosed using patch test and delayed reading of intradermal test. The result of those tests in 10 patients with a history of delayed RCM hypersensitivity [16] showed the positive rate of patch test and intradermal test was 10% respectively, but there was no correlation between them.
Previous studies had questioned about the usefulness of premedication in RCM. In a large-scale study published in 1990 [10], the relation between hypersensitivity reactions and premedication was evaluated according to the history of allergy and ionic/nonionic RCM. As a result, the positive effect of premedication was shown only in severe hypersensitivity reactions with the ionic contrast media and premedication could not reduce the risk of hypersensitivity reactions in nonionic contrast media group. The effect of premedication in subjects with a history of severe reaction and a positive pretest was analyzed [22], and it also showed no beneficial effect on the prevention of hypersensitivity reactions. In India, patients with allergic diathesis were pretreated with medication such as hydrocortisone, promethazine, theophylline before they were administered with high-osmolar contrast media [9], however, the premedication did not show a prior effect on reduction of hypersensitivity reactions. A case report published in Australia also took the effect of premedication on RCM hypersensitivity pessimistically [24]. Prednisolone 25 mg, cetirizine 10 mg, and ranitidine 150 mg were injected to patients who were diagnosed with RCM-induced anaphylaxis before readministration, but anaphylactic reaction with hypotension recurred even after premedication.
However, recent studies in Korea showed positive outcomes. Thirty patients who had showed immediate hypersensitivity after RCM injection received premedication of prednisolone 50 mg and antihistamine before readministration, and 25 of them didn't have any symptoms after premedication [25]. The success rate of premedication was higher in previous severe hypersensitivity group than mild group (92.3% vs. 76.5%, p < 0.001). Another Korean study [6] compared premedication use and outcome before and after the initiation of a mandatory RCM hypersensitivity reporting and automatic prescription system: intensive premedication with corticosteroid was significantly increased (65% vs. 14%, p < 0.001), and it significantly reduced breakthrough reactions (6.7% vs. 15.2%, p < 0.001).
In 2011, Korean guideline for the safe use of RCM was published by Korean Academy of Asthma, Allergy and Clinical Immunology and the Korean Society of Radiology (Korean Network of Allergists & Radiologists for Research of Radio-contrast Media-associated Adverse Reactions, KOAR3A. In this guideline, if a patient has previous history of severe immediate type RCM hypersensitivity, the preventive measure is 50 mg of oral prednisolone at 13 hours, 7 hours and an hour before injection of RCM, and 4 mg of chlorpheniramine at an hour before the injection. In emergency situations, 40 mg of intravenous methylprednisolone is injected every 4 hours before RCM exposure [26].
The overall prevalence of RCM hypersensitivity reactions in the Asia Pacific regions seems to be similar to those in other continents. Immediate reactions (less than an hour after the exposure), delayed reactions (after an hour to 7 days), and severe life threatening reactions (0.04-0.28%) are possible reactions. Type of procedures, allergy and other risk factors could play a role as risk factors. Role of skin test in RCM hypersensitivity revisited especially in the evaluation of patients with severe reactions. However, the value as a prescreening tool is still questionable. Avoidance and looking for alternatives are the best way in a patient with RCM hypersensitivity. Premedication could be helpful when it is necessary and not contraindicated, but physicians should be aware of breakthrough reactions.
Figures and Tables
References
1. Yang MS, Lee SH, Kim TW, Kwon JW, Lee SM, Kim SH, Kwon HS, Park CH, Park HW, Kim SS, Cho SH, Min KU, Kim YY, Chang YS. Epidemiologic and clinical features of anaphylaxis in Korea. Ann Allergy Asthma Immunol. 2008; 100:31–36.

2. Kim MH, Park CH, Kim DI, Kim KM, Kim HK, Lim KH, Song WJ, Lee SM, Kim SH, Kwon HS, Park HW, Yoon CJ, Cho SH, Min KU, Kim YY, Chang YS. Surveillance of contrast-media-induced hypersensitivity reactions using signals from an electronic medical recording system. Ann Allergy Asthma Immunol. 2012; 108:167–171.

3. Song WJ, Chang YS. Recent applications of basophil activation tests in the diagnosis of drug hypersensitivity. Asia Pac Allergy. 2013; 3:266–280.

4. Kim SH, Jo EJ, Kim MY, Lee SE, Kim MH, Yang MS, Song WJ, Choi SI, Kim JH, Chang YS. Clinical value of radiocontrast media skin tests as a prescreening and diagnostic tool in hypersensitivity reactions. Ann Allergy Asthma Immunol. 2013; 110:258–262.

5. Brockow K, Romano A, Aberer W, Bircher AJ, Barbaud A, Bonadonna P, Faria E, Kanny G, Lerch M, Pichler WJ, Ring J, Rodrigues Cernadas J, Tomaz E, Demoly P, Christiansen C. European Network of Drug Allergy and the EAACI interest group on drug hypersensitivity. Skin testing in patients with hypersensitivity reactions to iodinated contrast media - a European multicenter study. Allergy. 2009; 64:234–241.

6. Bae YJ, Hwang YW, Yoon SY, Kim S, Lee T, Lee YS, Kwon HS, Cho YS, Shin MJ, Moon HB, Kim TB. The effectiveness of automatic recommending system for premedication in reducing recurrent radiocontrast media hypersensitivity reactions. PLoS One. 2013; 8:e66014.

7. Kim SS, Park CH, Park MJ, Choi SH, Kim YS, Park HW, Chang YS, Shin CS, Oh BH, Min KU, Kim YY, Cho SH. Adverse reactions to radio-contrast media in computed tomography (CT) in general population: incidence and clinical features. Korean J Asthma Allergy Clin Immunol. 2007; 27:157–161.
8. Munechika H, Hiramatsu Y, Kudo S, Sugimura K, Hamada C, Yamaguchi K, Katayama H. A prospective survey of delayed adverse reactions to iohexol in urography and computed tomography. Eur Radiol. 2003; 13:185–194.

9. Thomas M, Peedicayil J, Koshi T, Korah I. Adverse reactions to radiocontrast media in an Indian population. Br J Radiol. 1999; 72:648–652.

10. Katayama H, Yamaguchi K, Kozuka T, Takashima T, Seez P, Matsuura K. Adverse reactions to ionic and nonionic contrast media. A report from the Japanese Committee on the Safety of Contrast Media. Radiology. 1990; 175:621–628.

11. Katayama H, Kozuka T, Ebata K. Assessment of the side-effects of iomeprol. Eur J Radiol. 1994; 18:Suppl 1. S115–S119.

12. Pradubpongsa P, Dhana N, Jongjarearnprasert K, Janpanich S, Thongngarm T. Adverse reactions to iodinated contrast media: prevalence, risk factors and outcome-the results of a 3-year period. Asian Pac J Allergy Immunol. 2013; 31:299–306.

13. Ho J, Kingston RJ, Young N, Katelaris CH, Sindhusake D. Immediate hypersensitivity reactions to IV non-ionic iodinated contrast in computed tomography. Asia Pac Allergy. 2012; 2:242–247.

14. Jung JW, Kang HR, Kim MH, Lee W, Min KU, Han MH, Cho SH. Immediate hypersensitivity reaction to gadolinium-based MR contrast media. Radiology. 2012; 264:414–422.

15. Oi H, Yamazaki H, Matsushita M. Delayed vs. immediate adverse reactions to ionic and non-ionic low-osmolality contrast media. Radiat Med. 1997; 15:23–27.
16. Goksel O, Aydın O, Atasoy C, Akyar S, Demirel YS, Misirligil Z, Bavbek S. Hypersensitivity reactions to contrast media: prevalence, risk factors and the role of skin tests in diagnosis: a cross-sectional survey. Int Arch Allergy Immunol. 2011; 155:297–305.
17. Katayama H, Tanaka T. Clinical survey of adverse reactions to contrast media. Invest Radiol. 1988; 23:Suppl 1. S88–S89.

18. Yasuda R, Munechika H. Delayed adverse reactions to nonionic monomeric contrast-enhanced media. Invest Radiol. 1998; 33:1–5.

19. Akiyama M, Nakada T, Sueki H, Fujisawa R, Iijima M. Drug eruption caused by nonionic iodinated X-ray contrast media. Acad Radiol. 1998; 5:Suppl 1. S159–S161.

20. Hosoya T, Yamaguchi K, Akutsu T, Mitsuhashi Y, Kondo S, Sugai Y, Adachi M. Delayed adverse reactions to iodinated contrast media and their risk factors. Radiat Med. 2000; 18:39–45.
21. Munechika H, Hiramatsu Y, Kudo S, Sugimura K, Hamada C, Yamaguchi K, Katayama H. Delayed adverse reactions to nonionic contrast medium (iohexol) in IV use: multicentric study. Acad Radiol. 2002; 9:Suppl 1. S69–S71.
22. Yamaguchi K, Katayama H, Takashima T, Kozuka T, Seez P, Matsuura K. Prediction of severe adverse reactions to ionic and nonionic contrast media in Japan: evaluation of pretesting: a report from the Japanese Committee on the Safety of Contrast Media. Radiology. 1991; 178:363–367.

23. Pinnobphun P, Buranapraditkun S, Kampitak T, Hirankarn N, Klaewsongkram J. The diagnostic value of basophil activation test in patients with an immediate hypersensitivity reaction to radiocontrast media. Ann Allergy Asthma Immunol. 2011; 106:387–393.

24. Worthley DL, Gillis D, Kette F, Smith W. Radiocontrast anaphylaxis with failure of premedication. Intern Med J. 2005; 35:58–60.

25. Kim SH, Lee SH, Lee SM, Kang HR, Park HW, Kim SS, Cho SH, Min KU, Kim YY, Chang YS. Outcomes of premedication for non-ionic radio-contrast media hypersensitivity reactions in Korea. Eur J Radiol. 2011; 80:363–367.

26. Shin MJ, Cho YJ. Management of adverse reaction to iodinated radiocontrast media. J Korean Med Assoc. 2012; 55:779–790.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download