Abstract
Background
Nowadays, there are many methods to reduce microorganisms in the air, such as dehumidifier, air purifier or humidity and temperature controller. The Precise Climate Controller is an instrument for controlling humidity and temperature, a concept that is demonstrated.
Objective
To determine the efficacy of this device, in order to reduce the quantity of the fungi and bacteria in the closed system.
Methods
This study is a perspective experimental study and is conducted as follows - the air sample in the closed system, a 42-cubic-meter room, is collected before the installation of the Precise Climate Controller. Next, the room is fumed with Aspergillus flavus and closed for 2 days. Then the instrument is in use in order to keep the relative humidity (RH) and the temperature constant at 55% RH and 25 degrees Celsius (℃). The air samples are collected every 3 days for 5 times during the period of 15 days to identify the type and calculate the quantity of the microorganisms.
Results
Before the Precise Climate Controller has been installed. Three species of bacteria are found in the air samples, but none of the fungus exists in the testing room. Once the room has been fumed with a large amount of A. flavus and the instrument is in use for 3 days, nine colonies of A. flavus are identified, but later on when the instrument is in use for 6, 9, 12, and 15 days, the air samples contain neither fungus nor bacteria.
Allergic rhinitis, asthma and respiratory infections are major public health problems in many countries, especially in Thailand where its location is in the tropical zone. Each year, the expenses on the controls and the remedies of those problems are accounted for the significant components of the annual government statement of expenditure [1].
The most common causes of allergic rhinitis are the residential allergens - especially dust mite and fungus in the species of Alternaria, Cladosporium, Aspergillus, Mucor, Rhizopus, and Merulius [2, 3, 4]. Approximately 10% of the incidents come from these causes. Furthermore, the number is on the rise from year to year. The rise can be mainly explained by the humidity and also by the usages of humidifier in the residential areas. As a result, the allergens from dust mites and fungi increase [5]. The most effective strategies to tackle the allergy are to educate the patients and to inform them how to avoid the allergens.
Respiratory infections are commonly caused by the bacteria and virus, such as Streptococcus pneumonia, Haemophilius influenzae, Moraxella catarrhalis, Pseudomonas aeruginosa, Staphylococus aureus, Mycoplasma pneumonia, Parainfluenza, Varicella-zoster, and Adeno viruses. These pathogens can easily contaminate through the air. If the room conditions are appropriate, these pathogens can suspend in the air range from 3-4 days to even a month. Therefore, just an adequate exposure to these pathogens can cause the infections, especially for those individuals who are weak [6].
Generally, the suitable condition for the fungi to thrive is the place where the relative humidity (RH) is 75%, such as kitchen, bathroom, and ceiling [2]. A numbers of methods are available to eradicate fungi in the residential areas e.g., keeping the temperature of the residential areas to be approximately 23-25 degrees Celsius (℃) by installing the air conditioning unit within the residential areas. In addition, keeping the RH of the residential areas to be between 40-60% can also help us get rid of the fungi. This can easily be achieved by installing the air ventilation systems and by introducing the sunlight thoroughly to the residential areas. Wherever the fungi are found, it is recommended to apply the fungal antiseptic solutions, such as Lysol and Clorox, to eradicate the fungi. Moreover, ones also find out that high efficiency particulate air filters (HEPA filters) can help reduce the amount of the fungi. However, there is no sufficient evidence to conclude that using HEPA filters can help the patients who have Allergic rhinitis reduce the nasal symptoms [7, 8].
Arundel et al. [9] reports that high RH condition and the usage of humidifier increase the rate of propagating for both infectious and allergenic organisms-fungus, protozoa, mite, bacteria and virus. The increases of these infectious and allergenic organisms indirectly cause the escalation of allergy and the infectious respiratory diseases. For the low RH condition-below 20% RH, this causes the eye irritation, dry nose and throat [10, 11].
Sterling EM finds that the growth of fungi can be suppressed if the RH is kept at 50% RH. This is also true for the growth of dust mites, viruses, and bacteria [6]. American Society of Heating, Refrigerating and Air-Conditioning Engineers report that at 50% RH along with 25℃ is not only the suitable condition for the eradication of the fungi and dust mites, but also the comfortable condition for human beings [6].
According to the preliminary report about the relationship between the RH and the propagation of dust mites from Parasitology Department, Faculty of Medicine, Siriraj Hospital, it states that the dust mites are completely eradicated within 7 days if the RH is kept at 50% RH as compare to the result with the case when the RH is kept at 75% RH along with 25℃ in the closed system - the perfect condition for the propagation of dust mites [12]. Since the RH and the temperature of the closed system can be kept constant by using the humidifier connected to air conditioning unit, this leads to the hypothesis that if the RH of the closed system can be kept constant at 50% RH at all times along with the appropriate temperature, we can then control the amount of fungi, bacteria and also dust mites.
Thus, the aim of this study is to determine the efficacy of controlling atmospheric conditions by using the Precise Climate Controller to reduce the amount of the fungi and bacteria. In this study we have considered both quantity and specie of the pathogens, we compare the results between before and after the RH and temperature of the closed system are controlled. If controlling the RH and temperature can significantly reduce the quantity and species of fungi and bacteria, this finding will be considerably beneficial for the patients with respiratory infections and allergy in term of reducing the severity of the disease and the frequent of the disease occurrence.
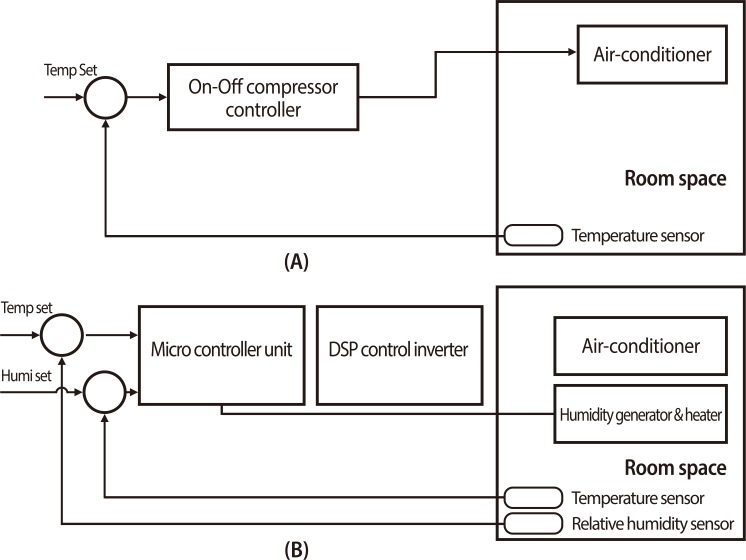
This study is a perspective experimental study, conducted from June 1, 2012 through September 30, 2012 at the Department of Otolaryngology, Phramongkutklao Hospital. Prior to the collection of the air sample, the daily RH and the temperature inside the testing room were recorded on 7 AM and 5 PM, consecutively for 45 days. The average RH of the data is 77% RH with the maximum of 83% RH and the minimum of 72% RH. The average temperature of the data is 32.5℃ with the maximum of 34.0℃ and the minimum of 26.0℃. The air sample inside the testing room was collected and identified the type and calculated the quantity of microorganisms, every three days for 5 times during the period of 15 days. Then the arranged Aspergillus flavus was fumed into the closed system, 4.0 m × 3.5 m × 3.0 m (42 cubic meters) room. The room has been installed with the Precise Climate Controller invented by Dr. Veerapon Monyakul, King Mongkut's University of Technology Thonburi [13]. This equipment is demonstrated in the Figs. 1, 2.
The Precise Climate Controller consists of a unit of humidifier and a unit of dehumidifier within the same case. The device has the dimension of 0.3 m × 1.0 m × 1.2 m (width × length × height) and is similar to a 10,000 BTU air condition (type TURBO A.P.S., Saijo Denki International Co., Muang Nonthaburi, Thailand). This device does operate with air-conditioning under the automatic control by microprocessor in order to keep the RH and temperature constant at all times, 55% RH and 25℃. This device has never been used as a commercial product.
The testing room is located in the microbiological lab of the microbiological research unit Phramongkutklao Hospital, Bangkok. This room, a closed space is estimated 3.5 m width, 4.0 m length, and 3.0 m height (approximated volume 42 m3). The room has been installed with the Precise Climate Controller and has been kept the RH at 55% RH and temperature at 25℃ constant at all times. Furthermore the active air sampler was located 1.5 m above the ground.
After the room had been closed for two days, then the fungi and bacteria in the room were collected by active air sampler (type, Impacter; model, RCS High Flow; Biotest Pharmaceuticals Co., Boca Raton, FL, USA). The 200-L air per two minutes were sucked through a culture media installed in the equipment. Then the culture media strip was sent for culturing. After culturing for 48 hours, the quantity of the microorganisms was reported in the term of the mean colony-forming units per plate and was also classified by the standard microbiological techniques.
Then the Precise Climate Controller, in which the RH and the temperature were set constant at 55% RH and 25℃, was turned on. We sampled the air from the testing room every 3 days for 5 times. The culture media was then cultured before the quantity of the fungi and bacteria was determined.
In this study, when we collected the sample every 3 days, for 5 times during the period of 15 days. Furthermore, each time we collected 3 collections of sample. Then the statistical analysis of the data regarding the species and the quantity of fungi and bacteria before and after controlling the RH and temperature was performed.
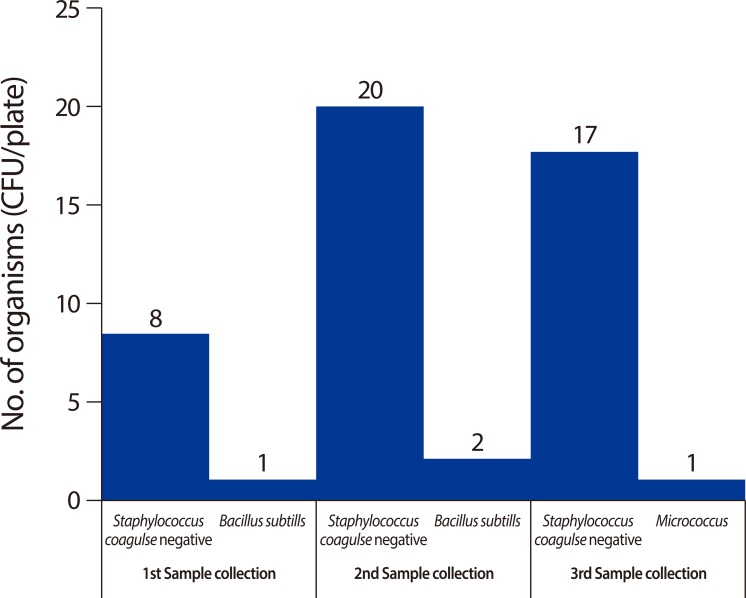
The room at Phramongkutklao Hospital was used as a closed system in this study. The air samples in this room were collected before the Precise Climate Controller was installed. Once the samples were cultured, three species of bacteria were found, Staphylococcus coagulse negative, Bacillus subtilis, and Micrococcus spp., but no fungus was found. The results are shown in Fig. 3.
Next, the A. flavus was fumed in the room. The room was kept closed for 2 days. We then collected the air samples from the closed room and cultured them. We have found a significantly large amount of A. flavus. The outside air was also cultured, 3 species of bacteria were found, S. coagulse negative, B. subtilis, and Micrococcus spp., together with 2 species of fungus, Curvularia spp. and A. flavus.
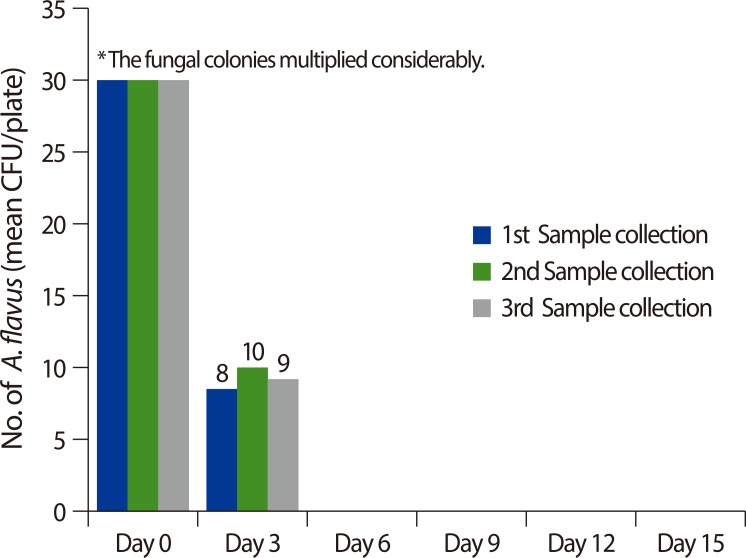
Thereafter, the Precise Climate Controller was turned on and operated with air-conditioning in order to control the RH at 55% RH and the temperature at 25℃ constantly. We then collected the air samples again and cultured them. The results are shown in Fig. 4.
When the Precise Climate Controller was in used, only the first batch of air samples - that were collected after the instrument was in used for 3 days, contained 9 colonies of A. flavus on average, but no bacteria. Other than the first batch of air samples that were collected after the instrument was in use for 6, 9, 12, and 15 days, contained neither fungus nor bacteria.
Since Thailand is located in the tropical zone, according to the Weather Forecast Bureau 2012, Thailand's average RH and temperature in rainy season are in the range of 70-80% RH and 24-32℃, respectively. These conditions are appropriate for indoor allergens-fungi and dust mites, to reproduce; therefore, these indoor allergens are major causes of the allergic diseases of airway in Thailand. This claim is also consistent with Gravesen's study that fungi would best thrive in the places with RH at 75% RH, such as kitchen and bathroom, the home area with high level of humidity [2]. As the matter of fact that nowadays the air conditions are prevalently used in the residential areas especially in bedrooms - closed systems, the temperatures of these closed systems are kept constant at 25℃ while putting no restriction on the RH of the rooms. Consequently, at this temperature allows the fungi to vastly reproduce.
The findings of this study are that once A. flavus is fumed into the room and the room is closed for 2 days, we cannot even determine the number of its colony since the fungi vastly reproduce. However, once the RH and the temperature are set constant at 55% and 25℃, the quantity of the fungi and bacteria continuously reduce; in addition, after the 5th time of culturing, the number of colony is not significant at the clinical significance level. These findings imply that controlling atmospheric conditions - the RH and temperature, has an efficacious result in term of limiting the quantity of the fungi and bacteria in the closed room. Our findings are consistent with Sterling RM's finding that keeping the RH at 50% can effectively inhibit the fungal growth [6].
According to the study of Bernstein [14] reported the first study to investigate the effect of dehumidification in conjunction with HEPA filtration [15]. They were able to show the reduction in airborne mold levels (p < 0.05) but it was not possible to determine whether the reduction of airborne mold spore levels was due mainly to dehumidification or air filtration intervention (HEPA). As compare to the results of our present study, the Precise Climate Controller could determine the reduction of the quantity of indoor microorganisms by mean of controlling the RH and the temperature.
Moreover, our study also finds that prior to the controlling atmospheric conditions-the RH and temperature, the air in the room contains bacteria such as S. coagulase negative, B. subtilis, and Micrococcus. But once the RH and temperature has been controlled and the air samples has been cultured for 5 times, those bacteria that were earlier found contained in the air completely vanish. Those bacteria are commonly found in many public places such as the hospitals according to the study of Kim et al. [16] states that Staphylococcus are found 50%, Micrococcus 15-20%, Corynebacterium 5-20% and Bacillus 5-15%. Our finding insists the fact that controlling atmospheric conditions has an efficacious result in term of limiting the quantity of the fungi and bacteria. This finding could help reduce the number of incidence of the respiratory infections caused by these pathogens especially for those patients with immunodeficiency that could be easily infected.
Another advantage of controlling the RH and temperature at the appropriate level is the capability to reduce the growth of dust mite. Arlian et al. [17] reports that dust mites will die within 5-11 days if the RH is less than 50%. And if the RH is higher than the Critical equilibrium humidity-its critical value is at 58% RH, for more than two hours per day, this allows the dust mites to survive.
According to this study, we can conclude that keeping the RH and the temperature constant at all times can significantly control the quantity and limit the growth of the fungi and bacteria - including dust mites, at clinical significance level. Therefore, this finding will be beneficial for the patients who suffer from allergy that is caused by allergens, such as fungi contaminated in the air. Furthermore, since Thailand is located in the tropical zone, it is common to find the allergens-both fungi and dust mites, considerably contaminated in the local atmosphere. We strongly believe that our findings can be applied for either economic purposes or medical purposes if there are some other in-depth studies supporting this topic. The authors, therefore, recommend that the further studies should be carried out in the real conditions, for instance, in the living room, bedroom or in the hospital ward so that outcomes can then be evaluated before recommendation and application to protect the infection for the patients who suffer from allergy and immunodeficiency.
In conclusion, controlling the RH and temperature at 55% and 25℃ by using the Precise Climate Controller yields a significant result in term of high efficaciousness in controlling the quantity of the indoor microorganisms in the closed system room.
ACKNOWLEDGEMENTS
This work was dedicated to Dr. Veerapon Monyakul, King Mongkut's University of Technology Thonburi. We thank him for providing a temporary loan of the Precise Climate Controller used in this study free of charge.
References
1. Bunnag C, Jareoncharsri P, Tantilipikorn P, Vichyanond P, Pawankar R. Epidemiology and current status of allergic rhinitis and asthma in Thailand: ARIA Asia-Pacific Workshop report. Asian Pac J Allergy Immunol. 2009; 27:79–86. PMID: 19548633.
3. Denning DW, O'Driscoll BR, Hogaboam CM, Bowyer P, Niven RM. The link between fungi and severe asthma: a summary of the evidence. Eur Respir J. 2006; 27:615–626. PMID: 16507864.

4. Li DW, Kendrick B. A year round comparison of fungal spores in indoor and outdoor air. Mycologia. 1995; 87:190–195.
5. Wraith DG, Cunnington AM, Seymour WM. The role and allergenic importance of storage mites in house dust and other environments. Clin Allergy. 1979; 9:545–561. PMID: 519837.

6. Sterling EM, Arundel A, Stering TD. Criteria for human exposure to humidity in occupied buildings. ASHRAE Trans. 1985; 91(Pt 1):611–622.
7. Reisman RE, Mauriello PM, Davis GB, Georgitis JW, DeMasi JM. A double-blind study of the effectiveness of a high-efficiency particulate air (HEPA) filter in the treatment of patients with perennial allergic rhinitis and asthma. J Allergy Clin Immunol. 1990; 85:1050–1057. PMID: 2191991.
8. Sheikh A, Hurwitz B, Shehata Y. House dust mite avoidance measures for perennial allergic rhinitis. Cochrane Database Syst Rev. 2007; (1):CD001563. PMID: 17253461.

9. Arundel AV, Sterling EM, Biggin JH, Sterling TD. Indirect health effects of relative humidity in indoor environments. Environ Health Perspect. 1986; 65:351–361. PMID: 3709462.

10. MacIntyre DA. Response to atmospheric humidity at comfortable air temperature: a comparison of three experiments. Ann Occup Hyg. 1978; 21:177–190. PMID: 697270.
11. Eng WG. Survey on eye comfort in aircraft: I. Flight attendants. Aviat Space Environ Med. 1979; 50:401–404. PMID: 464966.
12. Siriraj Dust Mite Center for Services and Research. Department of Parasitology, Faculty of Medicine Siriraj Hospital. Mahidol University. Precise climate controller for eliminating house dust mites: test report. Salaya: Mahidol University;2012.
13. Sookahaiya T, Monyakul V, Thepa S. Assessment of the thermal environment effect a human comfort and health for the development of novel air conditioning system in tropical regions. Energy Build. 2010; 42:1692–1702.
14. Bernstein JA, Levin L, Crandall MS, Perez A, Lanphear B. A pilot study to investigate the effects of combined dehumidification and HEPA filtration on dew point and airborne mold spore counts in day care centers. Indoor Air. 2005; 15:402–407. PMID: 16268830.

15. Sublett JL. Effectiveness of air filters and air cleaners in allergic respiratory diseases: a review of the recent literature. Curr Allergy Asthma Rep. 2011; 11:395–402. PMID: 21773748.

16. Kim KY, Kim YS, Kim D. Distribution characteristics of airborne bacteria and fungi in the general hospitals of Korea. Ind Health. 2010; 48:236–243. PMID: 20424357.

17. Arlian LG, Neal JS, Morgan MS, Vyszenski-Moher DL, Rapp CM, Alexander AK. Reducing relative humidity is a practical way to control dust mites and their allergens in homes in temperate climates. J Allergy Clin Immunol. 2001; 107:99–104. PMID: 11149998.

Fig. 1
The Precise Climate Controller invented by Dr. Veerapon Monyakul, King Mongkut's University of Technology Thonburi.

Fig. 2
Diagram comparing the conventional air conditioning system (A) and the Precise Climate Controller system (B). DSP, digital signal processor.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download