1. Joint Task Force on Practice Parameters. American Academy of Allergy, Asthma and Immunology. American College of Allergy, Asthma and Immunology. Joint Council of Allergy, Asthma and Immunology. Drug allergy: an updated practice parameter. Ann Allergy Asthma Immunol. 2010; 105:259–273. PMID:
20934625.
2. Gadde J, Spence M, Wheeler B, Adkinson NF Jr. Clinical experience with penicillin skin testing in a large inner-city STD clinic. JAMA. 1993; 270:2456–2463. PMID:
8230623.

3. Gomes E, Cardoso MF, Praca F, Gomes L, Marino E, Demoly P. Self-reported drug allergy in a general adult Portuguese population. Clin Exp Allergy. 2004; 34:1597–1601. PMID:
15479276.

4. Branellec A, Thomas M, Fain O, Kettaneh A, Stirnemann J, Letellier E. Frequency of self-reported penicillin allergy in the area of Seine-Saint-Denis (France). Rev Med Interne. 2008; 29:271–276. PMID:
17950958.
5. Sagar PS, Katelaris CH. Utility of penicillin allergy testing in patients presenting with a history of penicillin allergy. Asia Pac Allergy. 2013; 3:115–119. PMID:
23667835.

6. Park M, Markus P, Matesic D, Li JT. Safety and effectiveness of a preoperative allergy clinic in decreasing vancomycin use in patients with a history of penicillin allergy. Ann Allergy Asthma Immunol. 2006; 97:681–687. PMID:
17165279.

7. Solensky R, Earl HS, Gruchalla RS. Clinical approach to penicillin-allergic patients: a survey. Ann Allergy Asthma Immunol. 2000; 84:329–333. PMID:
10752918.

8. Kwan T, Lin F, Ngai B, Loeb M. Vancomycin use in 2 Ontario tertiary care hospitals: a survey. Clin Invest Med. 1999; 22:256–264. PMID:
10664867.
9. MacLaughlin EJ, Saseen JJ, Malone DC. Costs of beta-lactam allergies: selection and costs of antibiotics for patients with a reported beta-lactam allergy. Arch Fam Med. 2000; 9:722–726. PMID:
10927711.

10. Puchner TC Jr, Zacharisen MC. A survey of antibiotic prescribing and knowledge of penicillin allergy. Ann Allergy Asthma Immunol. 2002; 88:24–29. PMID:
11814274.

11. Lee CE, Zembower TR, Fotis MA, Postelnick MJ, Greenberger PA, Peterson LR, Noskin GA. The incidence of antimicrobial allergies in hospitalized patients: implications regarding prescribing patterns and emerging bacterial resistance. Arch Intern Med. 2000; 160:2819–2822. PMID:
11025792.
12. Rao GG. Risk factors for the spread of antibiotic-resistant bacteria. Drugs. 1998; 55:323–330. PMID:
9530540.

13. Murray BE. Vancomycin-resistant enterococcal infections. N Engl J Med. 2000; 342:710–721. PMID:
10706902.

14. Martínez JA, Ruthazer R, Hansjosten K, Barefoot L, Snydman DR. Role of environmental contamination as a risk factor for acquisition of vancomycin-resistant enterococci in patients treated in a medical intensive care unit. Arch Intern Med. 2003; 163:1905–1912. PMID:
12963563.

15. Borch JE, Andersen KE, Bindslev-Jensen C. The prevalence of suspected and challenge-verified penicillin allergy in a university hospital population. Basic Clin Pharmacol Toxicol. 2006; 98:357–362. PMID:
16623858.

16. Solley GO, Gleich GJ, Van Dellen RG. Penicillin allergy: clinical experience with a battery of skin-test reagents. J Allergy Clin Immunol. 1982; 69:238–244. PMID:
7056954.

17. Messaad D, Sahla H, Benahmed S, Godard P, Bousquet J, Demoly P. Drug provocation tests in patients with a history suggesting an immediate drug hypersensitivity reaction. Ann Intern Med. 2004; 140:1001–1006. PMID:
15197017.

18. Levine BB, Ovary Z. Studies on the mechanism of the formation of the penicillin antigen. III. The N-(D-alpha-benzylpenicilloyl) group as an antigenic determinant responsible for hypersensitivity to penicillin G. J Exp Med. 1961; 114:875–904. PMID:
14464604.
19. Levine BB, Redmond AP. Minor haptenic determinant-specific reagins of penicillin hypersensitivity in man. Int Arch Allergy Appl Immunol. 1969; 35:445–455. PMID:
5781774.

20. Parker CW, Shapiro J, Kern M, Eisen HN. Hypersensitivity to penicillenic acid derivatives in human beings with penicillin allergy. J Exp Med. 1962; 115:821–838. PMID:
14483916.

21. Romano A, Gueant-Rodriguez RM, Viola M, Amoghly F, Gaeta F, Nicolas JP, Gueant JL. Diagnosing immediate reactions to cephalosporins. Clin Exp Allergy. 2005; 35:1234–1242. PMID:
16164453.

22. Blanca M, Vega JM, Garcia J, Carmona MJ, Terados S, Avila MJ, Miranda A, Juarez C. Allergy to penicillin with good tolerance to other penicillins; study of the incidence in subjects allergic to beta-lactams. Clin Exp Allergy. 1990; 20:475–481. PMID:
2253079.

23. Vega JM, Blanca M, Garcia JJ, Carmona MJ, Miranda A, Perez-Estrada M, Fernandez S, Acebes JM, Terrados S. Immediate allergic reactions to amoxicillin. Allergy. 1994; 49:317–322. PMID:
8092427.

24. Blanca M, Romano A, Torres MJ, Fernandez J, Mayorga C, Rodriguez J, Demoly P, Bousquet PJ, Merk HF, Sanz ML, Ott H, Atanaskovic-Markovic M. Update on the evaluation of hypersensitivity reactions to betalactams. Allergy. 2009; 64:183–193. PMID:
19133923.

25. Sampson HA, Munoz-Furlong A, Campbell RL, Adkinson NF Jr, Bock SA, Branum A, Brown SG, Camargo CA Jr, Cydulka R, Galli SJ, Gidudu J, Gruchalla RS, Harlor AD Jr, Hepner DL, Lewis LM, Lieberman PL, Metcalfe DD, O'Connor R, Muraro A, Rudman A, Schmitt C, Scherrer D, Simons FE, Thomas S, Wood JP, Decker WW. Second symposium on the definition and management of anaphylaxis: summary report--Second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network symposium. J Allergy Clin Immunol. 2006; 117:391–397. PMID:
16461139.

26. Torres MJ, Blanca M, Fernandez J, Romano A, Weck A, Aberer W, Brockow K, Pichler WJ, Demoly P. ENDA. EAACI Interest Group on Drug Hypersensitivity. Diagnosis of immediate allergic reactions to beta-lactam antibiotics. Allergy. 2003; 58:961–972. PMID:
14510712.

27. Aberer W, Bircher A, Romano A, Blanca M, Campi P, Fernandez J, Brockow K, Pichler WJ, Demoly P. European Network for Drug Allergy (ENDA). EAACI interest group on drug hypersensitivity. Drug provocation testing in the diagnosis of drug hypersensitivity reactions: general considerations. Allergy. 2003; 58:854–863. PMID:
12911412.

28. Abdulazeez S, Al Tajir GK, Sulieman H. Assessment of the current practice of antibiotic skin testing in a tertiary hospital in United Arab Emirates. J Infect Dev Ctries. 2011; 5:759–764. PMID:
22112728.

29. Doña I, Blanca-Lopez N, Torres MJ, Garcia-Campos J, Garcia-Nunez I, Gomez F, Salas M, Rondon C, Canto MG, Blanca M. Drug hypersensitivity reactions: response patterns, drug involved, and temporal variations in a large series of patients. J Investig Allergol Clin Immunol. 2012; 22:363–371.
30. Macy E, Poon KY. Self-reported antibiotic allergy incidence and prevalence: age and sex effects. Am J Med. 2009; 122:778.e1–778.e7. PMID:
19635279.

31. Celik GE, Aydin O, Dogu F, Cipe F, Boyvat A, Ikinciogullari A, Akyol A, Demirel YS. Diagnosis of immediate hypersensitivity to β-lactam antibiotics can be made safely with current approaches. Int Arch Allergy Immunol. 2012; 157:311–317. PMID:
22056615.

32. Bousquet PJ, Co-Minh HB, Arnoux B, Daures JP, Demoly P. Importance of mixture of minor determinants and benzylpenicilloyl poly-L-lysine skin testing in the diagnosis of beta-lactam allergy. J Allergy Clin Immunol. 2005; 115:1314–1316. PMID:
15940154.
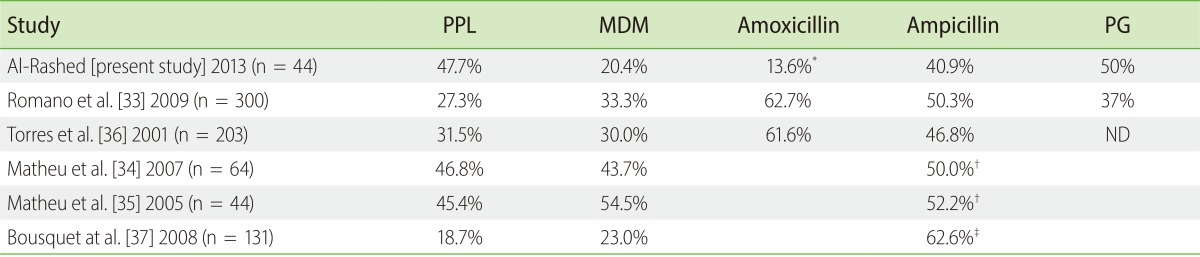
33. Romano A, Bousquet-Rouanet L, Viola M, Gaeta F, Demoly P, Bousquet PJ. Benzylpenicillin skin testing is still important in diagnosing immediate hypersensitivity reactions to penicillins. Allergy. 2009; 64:249–253. PMID:
19133924.

34. Matheu V, Perez E, Gonzalez R, Poza P, de la Torre F, Sanchez-Machin I, Garcia-Robaina JC. Assessment of a new brand of determinants for skin testing in a large group of patients with suspected beta-lactam allergy. J Investig Allergol Clin Immunol. 2007; 17:257–260.
35. Matheu V, Perez-Rodriguez E, Sanchez-Machin I, de la Torre F, Garcia-Robaina JC. Major and minor determinants are high-performance skin tests in beta-lactam allergy diagnosis. J Allergy Clin Immunol. 2005; 116:1167–1168. author reply 1168-9. PMID:
16275398.
36. Torres MJ, Romano A, Mayorga C, Moya MC, Guzman AE, Reche M, Juarez C, Blanca M. Diagnostic evaluation of a large group of patients with immediate allergy to penicillins: the role of skin testing. Allergy. 2001; 56:850–856. PMID:
11551249.

37. Bousquet PJ, Pipet A, Bousquet-Rouanet L, Demoly P. Oral challenges are needed in the diagnosis of beta-lactam hypersensitivity. Clin Exp Allergy. 2008; 38:185–190. PMID:
17976216.
38. Greenberger PA. 8. Drug allergy. J Allergy Clin Immunol. 2006; 117(2 Suppl Mini-Primer):S464–S470. PMID:
16455348.

39. Silva R, Cruz L, Botelho C, Cadinha S, Castro E, Rodrigues J, Castel-Branco MG. Work up of patients with history of beta-lactam hypersensitivity. Allergol Immunopathol (Madr). 2009; 37:193–197. PMID:
19775797.

40. Fontaine C, Mayorga C, Bousquet PJ, Arnoux B, Torres MJ, Blanca M, Demoly P. Relevance of the determination of serum-specific IgE antibodies in the diagnosis of immediate beta-lactam allergy. Allergy. 2007; 62:47–52. PMID:
17156341.
41. Blanca M, Mayorga C, Torres MJ, Reche M, Moya MC, Rodriguez JL, Romano A, Juarez C. Clinical evaluation of Pharmacia CAP System RAST FEIA amoxicilloyl and benzylpenicilloyl in patients with penicillin allergy. Allergy. 2001; 56:862–870. PMID:
11551251.
42. Legere HJ 3rd, Palis RI, Rodriguez Bouza T, Uluer AZ, Castells MC. A safe protocol for rapid desensitization in patients with cystic fibrosis and antibiotic hypersensitivity. J Cyst Fibros. 2009; 8:418–424. PMID:
19740711.

43. Ghosal S, Taylor CJ. Intravenous desensitization to ceftazidime in cystic fibrosis patients. J Antimicrob Chemother. 1997; 39:556–557. PMID:
9145836.

44. Madaan A1, Li JT. Cephalosporin allergy. Immunol Allergy Clin North Am. 2004; 24:463–476. PMID:
15242721.

45. Wendel GD Jr, Stark BJ, Jamison RB, Molina RD, Sullivan TJ. Penicillin allergy and desensitization in serious infections during pregnancy. N Engl J Med. 1985; 312:1229–1232. PMID:
3921835.

46. Solensky R. Drug desensitization. Immunol Allergy Clin North Am. 2004; 24:425–443. PMID:
15242719.

47. Naclerio R, Mizrahi EA, Adkinson NF Jr. Immunologic observations during desensitization and maintenance of clinical tolerance to penicillin. J Allergy Clin Immunol. 1983; 71:294–301. PMID:
6826989.

48. García Núñez I, Barasona Villarejo MJ, Algaba Marmol MA, Moreno Aguilar C, Guerra Pasadas F. Diagnosis of patients with immediate hypersensitivity to beta-lactams using retest. J Investig Allergol Clin Immunol. 2012; 22:41–47.
49. Goossens H, Ferech M, Vander Stichele R, Elseviers M. ESAC Project Group. Outpatient antibiotic use in Europe and association with resistance: a cross-national database study. Lancet. 2005; 365:579–587. PMID:
15708101.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download