Abstract
Background
Latex allergy and its clinical presentation are rising in prevalence across the globe, especially amongst patients with spina bifida (SB). While studies have been well-established in Europe and America, data from Asia are limited.
Methods
35 subjects with SB, aged 5 to 32 years answered a questionnaire and underwent skin prick test (SPT) using a latex solution, 3 common house dust mites and 3 commonly cross-reacting food allergens (banana, kiwi and avocado). We also noted the relation between latex sensitization with atopy and doctor-diagnosed allergy. The prevalence of cross-reactivity with fruits was also studied.
Results
Sensitization to latex (i.e. a positive SPT) was found in 16 (46%, 95% confidence interval 29%-63%) of the subjects. Only 5 (31%) of the subjects who were sensitized to latex had clinical manifestations. Atopy (i.e. positive SPT to house dust mites) was present in 23 (66%) of the subjects and 13 (57%) of them was also sensitized to latex. There was a positive trend between latex sensitization and atopy (81.2% vs. 52.6%, p = 0.076), as well as latex sensitization with those having both atopy and doctor-diagnosed allergy (i.e. asthma, allergic rhinitis, eczema, drug allergy) (93.8% vs. 63.2%, p = 0.032). Only 6 (38%) subjects had allergy to the food allergens tested.
Conclusion
Almost half of the SB patients in Singapore are sensitized to latex. This number is comparable to that in Europe and America. Positive trend between latex sensitization and those with both atopy and doctor-diagnosed allergy (p = 0.032) is suggestive of a possible cause-effect relationship.
Latex allergy in spina bifida (SB) patients has increasingly garnered interests from many countries as the numbers escalate over the last two decades in Europe and America.
While the incidence of latex allergy in the general population is 1% to 2% [1], SB patients are related to a markedly higher incidence of latex allergy, ranging from 20% to 70% [2-4], with risk of anaphylaxis in the operating theatre 500 times higher than that of control groups [4].
This is possibly due to early and repeated exposures to latex-containing products [2-5] in SB. Other factors found to have a positive correlation with development of such allergy include personal atopy [2, 3]. Strong cross-reactivity with several proteins from fruits and vegetables (kiwi, chestnut, avocado, tomato, potato and banana) have also been reported in SB who are sensitized to latex [4, 10], also often referred as latex-fruit syndrome [5, 6].
On the contrary, a study done in South African SB children in Cape Town showed a low overall prevalence of latex sensitization of 16.7% [7]. Similar findings have been seen in studies done in Turkey [8], Italy [5] and Venezuela [9]. Strict avoidance of latex exposure and a low frequency of surgical procedures have been suggested as the possible reasons behind this.
Data on latex allergy in children with SB in Asia has been limited and only one recent study in Singapore involving 7 children with SB, found the prevalence to be as high as 42% [7]. No larger studies are available to determine the true prevalence in Asia.
The aim of this study is to investigate the prevalence of latex sensitization, latex allergy and latex-food syndrome in SB patients in Singapore. We also aim to assess the relationship among latex sensitization, atopy and doctor-diagnosed allergy.
Thirty five patients with SB, including 18 males and 17 females, 5 to 32 years old (mean ± SD age: 19.5 ± 7.1) were studied (Table 1). The local ethics committee NHG Domain Specific Review Board approved the study. Patients and parents gave their informed consent to participate.
Questionnaires enquiring about past medical and surgical history, known allergies (food and drug allergy), personal and familial doctor-diagnosed allergy (asthma, eczema and allergic rhinitis) were administered. Past history of symptoms of allergy upon latex contact was likewise elicited.
A skin prick test (SPT) with a panel of 7 allergens, including latex (commercial latex preparation from Stallergenes, at concentration of 100 IR/mL); 3 commonly cross-reacting fruits like avocado, banana and kiwi; and the 3 most common house dust mites, Dermatophagoides pteronyssinus, Dermatophagoides farinae and Blomia tropicalis, were done.
Medications potentially interfering with the interpretation of SPT were discontinued for at least 48 hours prior to SPT.
A wheal of 3 mm or more, without any reaction to a negative control solution, was considered as positive reaction [10]. All 35 subjects underwent SPT.
Latex sensitization was defined as the presence of a positive SPT to latex preparation. The presence of latex sensitization with symptoms was defined as latex allergy. Any positive SPT to dust mites was referred as atopy; asthma, allergic rhinitis, eczema and drug allergy were classified as doctor-diagnosed allergy. Cross-reactivity with fruits was defined as SPT positive to food allergens in individuals sensitized to latex.
SPSS version 20.0 (IBM, Armonk, NY, USA) was used for statistical analysis. Association among latex sensitization, atopy and doctor-diagnosed allergy were assessed using Chi-square or Fisher's exact test. Statistical significance was set at p < 0.05.
The prevalence of latex sensitization in the 35 subjects with SB was 16 (46%, 95% confidence interval [CI] 29%-63%).
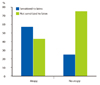
Only 5 (31%) of the subjects who were sensitized to latex had clinical manifestations. Fig. 1 shows individual symptoms.
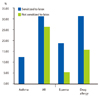
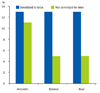
Atopy was present in 23 (66%) of the subjects, of which 13 (57%) had latex allergy (Fig. 2). The prevalence of asthma, allergic rhinitis and eczema among the subjects were 6%, 29% and 11% respectively. The prevalence of drug allergy is 23%. Fig. 3 illustrates the prevalence of latex sensitization in those with doctor-diagnosed allergy.
Only 6 (38%) subjects with latex sensitization had concomitant sensitization to the food allergen tested. Of the 35 subjects with SB, the prevalence of avocado, banana and kiwi allergy are 11%, 9% and 9% respectively (Fig. 4).
Although the prevalence is low, we noted a higher percentage of subjects with latex sensitization allergic to kiwi (12.5% vs. 5.3%, p = 0.45), avocado (12.5% vs. 10.5%, p = 0.86) and banana (12.5% vs. 5.3%, p = 0.45).
The prevalence of latex sensitization in the 35 Singapore patients with SB studied is 46% (95% CI 29%-63%). This is similar to that in Europe and America, where reported values ranged from 20%-70% [2-4]. It also corresponded with the previous study done in Singapore, where 7 subjects studied yield prevalence high at 42% [7].
There was a positive trend between latex sensitization and atopy (81.2% vs. 52.6%, p = 0.076), as well as latex sensitization with those having both atopy and doctor-diagnosed allergy (93.8% vs. 63.2%, p = 0.032).
The percentage of subjects with latex sensitization having doctor-diagnosed allergy was 56.2% (vs. 36.8%, p = 0.251).
In a study of 120 SB patients in Germany, Blumchen et al. [11] found the prevalence of atopy in SB after introduction of a primary latex-free prophylaxis to be 15%; as compared to SB patients 10 years ago with a prevalence of 35% (p = 0.001). Statistical significance remained even in the adjusted analysis.
The prevalence of atopy (15%) in SB with primary latex prophylaxis in place was comparable to that in the weighted German population sample of similar age. With SB patients having the same prevalence of atopy as the average paediatric population, genetic predisposition in SB for atopy or development of atopic diseases was less likely. Hence, Blumchen et al. [11] postulated that his data might suggest the potential for risk reduction in sensitization spreading and development of atopic diseases with the prevention of sensitization to latex.
Latex-fruit syndrome [5, 6], where latex allergy induces clinical reactions to plant-derived food, has been widely described [10, 11]. This was also demonstrated in our study where a higher percentage of patients with latex sensitization were allergic to kiwi, avocado and banana (Fig. 4).
The use of latex products in both the medical industry and community remains widespread. Given that latex allergy can result in a range of symptoms from urticaria to anaphylaxis and even death [6, 12], latex avoidance is an important step for both primary and secondary prevention.
While it is difficult to avoid latex products in the community, efforts to minimize latex contact in medical settings and increasing awareness of the individuals could potentially benefit our patients.
In conclusions, prevalence of latex sensitization in SB patients in Singapore was as high as 46% (95% CI 29%-63%).
There were also positive trends between latex sensitization and atopy and that with those having both atopy and doctor-diagnosed allergy, suggestive of possible cause-effect relationship.
It is thus important to take appropriate measures to ensure primary and secondary prevention of latex allergy.
Figures and Tables
References
2. Bernardini R, Novembre E, Lombardi E, Mezzetti P, Cianferoni A, Danti AD, Mercurella A, Vierucci A. Prevalence of and risk factors for latex sensitization in patients with spina bifida. J Urol. 1998. 160:1775–1778.

3. Valls A, Pascual CY, Caballero MT, Martín Esteban M. Latex allergy. Allergol Immunopathol (Madr). 2004. 32:295–305.
4. Beezhold DH, Sussman GL, Liss GM, Chang NS. Latex allergy can induce clinical reactions to specific foods. Clin Exp Allergy. 1996. 26:416–422.

7. Johar A, Lim DL, Arif SA, Hawarden D, Toit GD, Weinberg EG, Motala C, Fieggen G, Yeang HY, Potter PC. Low prevalence of latex sensitivity in South African spina bifida children in Cape Town. Pediatr Allergy Immunol. 2005. 16:165–170.

8. Gülbahar O, Demir E, Mete N, Ulman I, Can D, Sin A, Gülen F, Kokuludağ A, Tanaç R, Sebik F. Latex allergy and associated risk factors in a group of Turkish patients with spina bifida. Turk J Pediatr. 2004. 46:226–231.
9. Capriles-Hulett A, Sánchez-Borges M, Von-Scanzoni C, Medina JR. Very low frequency of latex and fruit allergy in patients with spina bifida from Venezuela: influence of socioeconomic factors. Ann Allergy Asthma Immunol. 1995. 75:62–64.
10. Niggemann B, Buck D, Michael T, Wahn U. Latex provocation tests in patients with spina bifida: who is at risk of becoming symptomatic? J Allergy Clin Immunol. 1998. 102:665–670.

11. Blumchen K, Bayer P, Buck D, Michael T, Cremer R, Fricke C, Henne T, Peters H, Hofmann U, Keil T, Schlaud M, Wahn U, Niggemann B. Effects of latex avoidance on latex sensitization, atopy and allergic diseases in patients with spina bifida. Allergy. 2010. 65:1585–1593.

12. Sussman GL, Beezhold DH. Latex allergy--a clinical perspective. J Long Term Eff Med Implants. 1994. 4:95–101.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download