This article has been
cited by other articles in ScienceCentral.
Abstract
Background
Intravenous immunoglobulin (IVIG) is a biological product with adverse effects that appears to vary considerably among different IVIG preparations.
Objectives
To describe the adverse events of patients given intravenous immunoglobulin infusions.
Method
Data was collected on all patients receiving IVIG infusion at a tertiary hospital from January 2001 to December 2010. Descriptive statistics was used.
Results
77 patients (45 males, 32 females) received IVIG infusions. Thirty two percent (n = 25) experienced adverse reactions. The most common indication was Kawasaki disease (85.7%) followed by immunodeficiency disorders (7.8%). Majority of the patients were children, with the highest frequency of infusions among those aged 2 to 8 years old (52%). 36 infusions were associated with occurrence of adverse effects. Fever was the most common adverse event (n = 11, 30.6%), followed by rash (n = 8, 22.2%) and chills (n = 7, 19.4%). Other adverse events were cyanosis (n = 3, 8.3%), hypotension (n = 2, 5.6%), hypothermia (n = 2, 5.6%), irritability (n = 1, 2.8%), vomiting (n = 1, 2.8%), and chest pain (n = 1, 2.8%). Adverse events were observed to occur most frequently within 1 to 6 h from onset of IVIG infusion. Among the various IVIG preparations available locally (Gammagard, Kiovig, Gamimune, Veno-S & IV Globulin S), Gammagard was the brand frequently used (50.7%). It also has the most number of adverse events, with 17 out of 41 (41.5%) infusions resulting in adverse reactions. Most of the reactions occurred with fast infusion rates, and clinical manifestations subsided when the rate of infusion was reduced.
Conclusion
In this study, thirty two percent of patients given IVIG infusions experienced adverse events. Fever was the most common manifestation. Symptoms occurred within 1 to 6 h from onset of infusion, were affected by fast infusion rates, and managed by reducing the rate of infusion.
Keywords: Intravenous immunoglobulins, Retrospective study, Side effects
INTRODUCTION
Immunoglobulin preparations were first used during the 1950s as a replacement therapy for primary immunodeficiency disorders [
1]. Initially, these were administered by intramuscular injection; however, in the early 1980s, highly purified monomeric suspensions of immunoglobulin G (IgG) for intravenous use became available, and these intravenous immunoglobulins (IVIG) are manufactured by different companies, and are at the disposal of the clinician [
2]. These preparations are mainly used as replacement therapy for immunodeficiency, and immunomodulatory therapy in autoimmune and inflammatory conditions [
3].
Intravenous immunoglobulin is a preparation of highly purified IgG derived from large pools of human plasma via ethanol fractionation with additional steps to remove immunoglobulin aggregates. Preparations are stabilized using substances such as human albumin, glycine, polyethylene glycol, or sugars such as sucrose, maltose or glucose. As a result of these processes, reactions may occur to either the immunoglobulin aggregates or the stabilizing agent [
3].
IVIG has been used successfully in different types of diseases. In primary immunodeficiencies, it is given at a dose of 400 mg/kg/month every 3-4 weeks. Patients with idiopathic thrombocytopenic purpura are given IVIG at a dose of 400 mg/kg daily for 5 days, or 1 g/kg/day for 2 days. Kawasaki disease patients are given a single dose of 2 g/kg.
As a replacement therapy for primary and secondary immunodeficiencies, intravenous administration of immune globulins is the usual way to provide IgG. A dose of 400-600 mg/kg/month given every 3 to 4 weeks is needed to increase the IgG level by 250 mg/dL for every 100 mg/kg infused. Its trough level increases slowly after a 6-month period with continued infusions, resulting in the saturation of the interstitial spaces with Ig [
4].
Different mechanisms have been described for the immune modulation and anti-inflammatory actions of IVIG. In Kawasaki disease, the effects of IVIG may be related to the neutralizing antibody activity in IVIG against proinflammatory cytokines and bacterial enterotoxins, such as Staphylococcal enterotoxins which are said to be responsible for the inflammatory and immunologic manifestations in patients with Kawasaki disease. It was also postulated by Leung and colleagues that cytokines in these patients can stimulate local inflammatory responses of blood vessels and IVIG could modulate the cytokine-mediated endothelial cell activation by neutralizing the effects of cytokines, inhibiting endothelial cell responses to cytokines, or inhibiting the production of cytokines and growth factors [
5].
Although not stated as an indication for IVIG use, a lot of clinicians give IVIG for patients who have sepsis or septic shock. Studies have been done, and some authors stressed the potential of IVIG as treatment for immunocompromised patients. Examples are neonates who have immunoglobulin and complement deficiencies, and intensive care unit patients who develop immunodepression secondary to severe underlying illnesses, surgery or chemotherapy [
6]. Proposed mechanisms of action include: preventing the harmful consequences induced by the lipid-A component of the endotoxin molecule by neutralization of the endotoxin in the patient's circulation; and bacterial opsonization, antigen neutralization and cytokine modulation resulting in suppression of pro-inflammatory responses in patients with severe Group A streptococcal infection. A Cochrane review by Alejandria and colleagues showed that polyclonal IVIG reduced mortality among adults with sepsis, however, no reduction of mortality was seen in neonates. The review stated that most of the trials were small and the totality of evidence is insufficient to support a conclusion of benefit [
6].
The rate of IVIG infusions should be low at the beginning and increased every 15-30 min, based on the patient's tolerance. A 5% solution of IVIG is initially infused at a rate of 0.5 mL/kg/h. If this is tolerated, infusion rate is gradually increased to a maximum of 4 mL/kg/h. Infusion of a standard dose (e.g. 400 mg/kg) may take up to 8 h in some patients. Studies have also been done showing that IVIG could be infused over a 3-h period, but a faster rate of infusion is poorly tolerated [
2].
Adverse events following IVIG infusions may be classified as immediate (occurring during the infusion itself) or delayed (occurring after the infusion has ceased) [
3]. These adverse events may be due to the relative "impurity" of the commercial preparations, or the undesirable effects of its active component (IgG) [
2]. The most common adverse effects occur soon after infusions and can include headache, flushing, chills, myalgia, wheezing, tachycardia, lower back pain, nausea, and hypotension [
3].
Intravenous immunoglobulin is a biological product, and potentially important product-manufacturing differences may exist. It is perhaps for this reason that adverse effects appear to vary considerably among different IVIG preparations available in the market. This study aims to determine the incidence and type of adverse events following the infusion of different IVI preparations among various types of patients. Knowledge of the common side effects in our local setting, and the IVIG preparations commonly involved, will be important in the care of patients who are receiving IVIG.
Objectives
General: To describe the adverse events of patients given IVIG infusions
Specific:
To describe the demographics (age, gender, family history of atopy, personal history of atopy, indication for IVIG treatment, inpatient or outpatient setting, presence of comorbidities) of patients who had adverse reactions to intravenous immunoglobulin therapy
To describe the incidence of adverse reactions among patients given immunoglobulin therapy
-
To describe the specific adverse events or clinical manifestations of patients given IVIG as to:
Onset of IVIG infusion
Specific reactions or manifestations
IVIG preparation, dose and infusion rate
Management done (slowing down the infusion rate, stopping the infusion temporarily, symptomatic treatment, premedication)
MATERIALS AND METHODS
This is a retrospective study. Charts of patients given IVIG at the ward and at the outpatient department from January 2001 to December 2010 at Dr. Fe del Mundo Medical Center were reviewed. Demographic data such as age, sex, indication for IVIG treatment, inpatient or outpatient setting, and comorbidities were taken from the charts of all patients. Once patients with adverse reactions have been identified, the following data were taken and reviewed: specific type of adverse reaction to IVIG; time interval between onset of IVIG infusion and appearance of adverse reactions; IVIG preparation, dose and infusion rate; and medical management done during the adverse event. Descriptive statistics was used to analyze and interpret the data.
Operational definition of variables
IVIG - a blood product given intravenously that contains pooled IgG antibodies from the plasma of approximately a thousand or more blood donors
Adverse events - undesirable effects that occur immediately (within 30-60 min) after the onset of IVIG infusion, or delayed until a few days after infusion
Generalized adverse reactions - mild, self-limited reactions that begin 30-60 min after onset of infusion and include the following: nausea, vomiting, chills, heachache, myalgia, low back pain, and flushing
Hypersensitivity and anaphylactic reactions -appearance of skin rash and severe or even fatal anaphylactoid reactions; this usually occurs among IgA deficient patients treated with IVIG
Comorbidities - other diseases present in the patient treated with IVIG; includes cardiovascular diseases, diabetes, and preexisting renal insufficiency
RESULTS
General patient characteristics
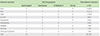
A total of 77 patients, 45 males (58.4%) and 32 females (41.6%) aged 2 months to 53 years, received intravenous immunoglobulin infusions from 2001-2010. Majority of these patients were diagnosed with Kawasaki disease (n = 66, 85.7%) and were admitted at the hospital. There were 4 patients who had associated comorbidities: one had congenital heart disease (atrial septal defect with small ventricular septal defect), another had osteomyelitis, one had cerebral palsy, and one had idiopathic thrombocytopenic purpura. A review of the family history revealed that 46 patients had a positive family history of atopy. Four patients, on the other hand, had a personal history of atopy, with 2 patients having bronchial asthma and 2 patients with food allergy. Data are shown in
Table 1.
Patient characteristics of those with adverse reactions
Table 1 also shows the demographics of patients who experienced adverse events while receiving IVIG transfusion. Twenty-five patients (14 males, 11 females) had adverse reactions, with majority belonging to the 2-8 y/o age group (n = 12, 48%). Most patients who had adverse events were admitted patients given IVIG for Kawasaki disease (n = 23, 92%). In addition, 16 patients who had adverse events have a family history of atopy.
Adverse events
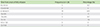
There were 36 adverse events reported during IVIG transfusions, with some patients experiencing more than one adverse reaction. As seen in
Table 2, the top 3 adverse effects were fever, skin rash and chills.
Among the various IVIG preparations available locally, Gammagard was the brand most frequently used (n = 41, 50.7%), as seen in
Fig. 1. It also has the most number of adverse events, with 17 out of 41 infusions (41.5%) resulting in adverse reactions. This is followed by Gamimmune (4 out of 18; 22.2%) and IV-Globulin S (3 out of 20; 15%).
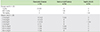
Adverse events were noted to occur most frequently within 1 to 6 h from onset of IVIG infusion (see
Table 3). Out of the 25 patients who had adverse reactions, there were 2 patients who had recurring episodes of reactions during the transfusion. The first patient developed fever at 2½ h - and had hypothermia at 13 h - from onset of IVIG infusion. The second patient, on the other hand, had 3 reactions during transfusion: from onset of infusion, he developed a skin rash at 30 min, then complained of chest pain and dyspnea 4½ h later, after which he again developed a rash at 18 h.
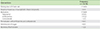
The most common indication for IVIG infusion as previously stated was Kawasaki disease. Hence, the dosage most commonly associated with adverse effects is the dose used for this disease, which is 2 g/kg (23 out of 25 infusions, 92%). One patient given IVIG at a dose of 763 mg/kg for septic shock also had an adverse reaction, as well as one patient given IVIG at a dose of 600 mg/kg for T cell deficiency (see
Table 4).
Upon observing an adverse reaction, different interventions were done to stop the reactions. Most physicians slow down the infusion rate and give medications such as paracetamol, antihistamines and corticosteroids (n = 17, 36.9%). Oxygen and intravenous fluid hydration were also given to some patients with reactions. One patient had hypotension on the 5th h of IVIG infusion and a fast drip of plain lactated Ringer's solution was given. Afterwards, this patient was shifted to another brand, and the rest of the infusion was unremarkable. Once the patient is already stable and IVIG infusion is to be continued, some physicians premedicate. There were two patients who were premedicated with hydrocortisone and diphenhydramine after an adverse reaction to IVIG infusion, one patient who was premedicated with diphenhydramine alone, and one patient who was premedicated with hydrocortisone alone. The patient given diphenhydramine alone still had an episode of low-grade fever after resuming the IVIG infusion. The infusion rate was then slowed down, and no recurrence of adverse events occurred (see
Table 5).
DISCUSSION
In our study, 44% of IVIG infusions had adverse events, from common reactions such as fever, rash and chills to rare ones such as hypothermia and chest pain with dyspnea. The most common adverse reactions to IVIG are nonanaphylactic reactions, which usually occurs in the first 30 min of administration and occurs in approximately 5% of infusions [
4]. These include fever, chills, mild nausea and/or vomiting, backache, abdominal pain, myalgia, headache and even some vasomotor and cardiovascular manifestations marked by changes in blood pressure and tachycardia. These reactions are probably due to aggregated immunoglobulin molecules which cause the complement system to be activated, antigen-antibody reactions, possible contaminants or even stabilizers that may have been used during the manufacturing process. Patients with hypersensitivity reactions, on the other hand, may have clinical manifestations due to IgA deficiency. The pathogenesis of other adverse reactions is still unknown [
2]. These adverse reactions can be managed by slowing down the infusion rate and giving of medications such as antihistamines, paracetamol and corticosteroids.
This study shows that despite the numerous precautions taken during IVIG infusions, patients still experience adverse effects. One reason is that IVIG is a biological product derived from blood products; hence, some adverse reactions are still expected to occur with its administration [
7].
There are IVIG components that may affect its properties and consequently play a role in a patient's tolerability [
8]. Major determinants include sodium content, sugar content and osmolality [
9]. The characteristics of the locally-available IVIG preparations are presented in
Supplement 1.
The sodium content of an IVIG determines the osmolality of the infused solution, which in turn can affect tolerability and occurrence of adverse effects. Patients with hypertension and renal impairment may be affected by a high-sodium content solution. Sugars such as sorbitol, sucrose and glucose are added to some IVIG preparations as stabilizers which will prevent aggregate formation. However, there seems to be an association between these sugars and the development of acute renal failure or insufficiency in treated patients [
9]. The preparations reviewed in this study showed only minimal amounts of sodium and sugar, and none of the patients given IVIG developed any renal complications.
The total number of osmotically active particles in a solution is referred to as the solution's osmolality. It is also equal to the sum of the molalities of all solutes present in a solution, and some of these solutes include sodium, sugars, and amino acids. Physiologic osmolality is 280-296 mOsm/kg; IVIG solutions may range in osmolality from physiologic values to greater than 1,000 mOsm. Sugar-stabilized solutions, such as Gammagard and IV Globulin-S tend to have higher osmolality compared to the sugar-free preparations like Gamimmune and Kiovig. The hyperosmolar solutions may cause fluid shifts when given intravenously, and this may result in hemodynamic changes leading to infusion-related adverse effects [
9].
There are also minor determinants that can affect the properties of IVIG. The pH of many IVIG products is in the range of 6-7; however, in order to prevent aggregation, it must be at a pH of 4-4.5. Hence, an IVIG with a pH greater than 4.5 needs agents that can maintain its stability and its ability to prevent aggregation, as seen in Gammagard. On the other hand, IVIG with low-pH preparations are easily neutralized by the buffering action of blood [
8,
9]. The IgA content of a solution is significant for patients with IgA deficiency, or those with anti-IgA antibodies of the IgG and IgE isotypes. These patients are more likely to develop severe and sometimes fatal anaphylactoid reactions [
2]. The content of IgA varies among different IVIG preparations. However, using a preparation that is low in IgA does not guarantee an adverse reaction-free infusion. Screening for anti-IgA antibodies is not recommended by the NIH consensus conference on IVIG; however, screening is still done in some countries [
9]. In our local setting, screening is not done because of financial constraints; most families would rather concentrate their resources on purchasing IVIG-which is very expensive-when it is indicated for a family member's illness.
The ability to tolerate the effects of IVIG infusion without experiencing adverse effects varies from one person to another and from one IVIG preparation to another as well. The rate of infusion, which influences the occurrence of adverse reactions, is also affected by the osmolality and sugar content of a preparation. The higher the osmolality and the sugar content, the slower should be the infusion rate [
9]. In our study, most of the adverse effects occurred at the recommended infusion rate of the IVIG preparation (Gammagard, at 4 mL/kg/h).
In conclusion, thirty two percent of patients given IVIG infusions experienced adverse events. Fever was the most common manifestation, followed by skin rash and chills. Symptoms occurred within 1 to 6 h from onset of infusion, were affected by fast infusion rates, and managed by reducing the rate of infusion and giving of medications such as paracetamol, antihistamines and steroids. IVIG preparations differ in their composition and properties, and these can contribute to its efficacy and tolerability.
ACKNOWLEDGEMENTS
The authors would like to thank the staff of the Medical Records Section of the Dr. Fe del Mundo Medical Center for their invaluable help.
References
1. IVIG Guideline Development Group of the IVIG Expert Group. Clinical guidelines for the use of intravenous immunoglobulin. 2nd ed. London: Department of Health (UK);2008.
2. Duhem C, Dicato MA, Ries F. Side-effects of intravenous immune globulins. Clin Exp Immunol. 1994; 97:Suppl 1. 79–83.
3. Singh-Grewal D, Kemp A, Wong M. A prospective study of the immediate and delayed adverse events following intravenous immunoglobulin infusions. Arch Dis Child. 2006; 91:651–654.

4. Stiehm ER, Ochs HD, Winkelstein JA. Immunodeficiency disorders: general considerations. In : Stiehm ER, Ochs HD, Winkelstein JA, editors. Immunologic disorders in infants and children. 5th ed. Philadelphia: W.B. Saunders;2004. p. 289–345.
5. Ballow M. The IgG molecule as a biological immune response modifier: mechanisms of action of intravenous immune serum globulin in autoimmune and inflammatory disorders. J Allergy Clin Immunol. 2011; 127:315–323.

6. Alejandria MM, Lansang MA, Dans LF, Mantaring JB. Intravenous immunoglobulin for treating sepsis, severe sepsis and septic shock. Cochrane Database Syst Rev. 2002; CD001090.

7. Dashti-Khavidaki S, Aghamohammadi A, Farshadi F, Movahedi M, Parvaneh N, Pouladi N, Moazzami K, Cheraghi T, Mahdaviani SA, Saghafi S, Heydari G, Abdollahzade S, Rezaei N. Adverse reactions of prophylactic intravenous immunoglobulin; a 13-year experience with 3004 infusions in Iranian patients with primary immunodeficiency diseases. J Investig Allergol Clin Immunol. 2009; 19:139–145.
8. Purisima BC, Garcia RD, Leus A. A retrospective study on the efficacy of Gammagard S/D IVIG versus Vizcarra IVIG in the treatment of Kawasaki disease in Makati Medical Center from 1998-2003. Philippine J Pediatr. 2009; 57:11–16.
9. Lemm G. Composition and properties of IVIg preparations that affect tolerability and therapeutic efficacy. Neurology. 2002; 59:S28–S32.

Supplementary Material
Supplement 1
Characteristics of different intravenous immunoglobulin (IVIG) preparations [
8-
10]




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download