Abstract
Background
Th2 cells are crucially important in allergic disease and the possible involvement of Treg and Th17 cells has not been clearly identified.
Objective
To identify the mRNA expression of T cell transcription factors in nasal mucosa in patients with allergic rhinitis (AR) and to reveal their correlations with clinical features.
Methods
Eighteen patients with AR and 12 controls with turbinate hypertrophy were included. mRNA expression of the following transcriptional factors in nasal mucosa were measured by quantitative polymerase chain reaction; T-bet (Th1), GATA3 (Th2), retinoic acid-related orphan receptor C (RORC; Th17), and forkhead box P3 (Foxp3; Treg). mRNA expression was compared among groups and correlation between mRNA expression level and clinical features (rhinitis symptoms, eosinophil count, and IgE) were also investigated.
Results
GATA3 and RORC were significantly increased and Foxp3 was significantly decreased in the AR group. Moderate-to-severe AR group also had increased expression of GATA3 and RORC than mild AR group, suggesting severity of AR influence expression of transcription factors. Correlation analysis showed that none of these transcription factors were associated with severity of clinical symptoms, eosinophil counts and skin prick test severity and that IgE level was significantly correlated with expression level of GATA3 and RORC, suggesting an association of IgE production with Th2 and Th17 cells.
Allergic rhinitis (AR) is a disease characterized by rhinorrhea, itching sneezing and nasal obstruction. Its impact on quality of life is unequivocal. The role of T cells in AR has been amply investigated and the crucial role of T cells in the pathogenesis of allergic diseases including AR has been established.
Until recently T helper cells were classified into Th1 and Th2 cells according to their releasing cytokines. Mutual regulation between Th1 and Th2 cells (Th1/Th2 balance) has been considered to be important for the homeostasis of the body's immune regulation and dysregulation of the Th1/Th2 balance leads to excessive Th1 or Th2 cell activation, resulting in autoimmune disease or allergic diseases, respectively. This Th1/Th2 paradigm has been widely accepted for the past two decades.
Recently a new emerging T helper cell subset, Th17 was identified and characterized. Th17 cells are known to be involved with autoimmune disease and neutrophil infiltration [1]. The discovery of Th17 added additional complexity to the existing Th1/Th2 balance paradigm. The role of Th17 cells in AR is not clear and still controversial.
Another important T cell subset is a regulatory T cells (Treg), which modulate immunologic reactions by releasing inhibitory cytokines such as transforming growth factor-β and interleukin (IL)-10 [2]. The role of Treg in AR is also unclear and debatable.
This study was undertaken to evaluate mRNA expression of each T cell subset by measuring mRNA expression of each transcription factor and to analyze the correlations of each transcription factor with clinical features in patients with AR.
From March 2010 through September 2010, 12 nonallergic controls with turbinate hypertrophy and 18 patients with AR sensitive to house dust mite were included in this study. Out of 18 in AR group, 9 subjects were monosensitized to house dust mite and 9 subjects were polysensitized to both house dust mite and several different kinds of pollens. The mucosa of inferior turbinate were obtained during turbinoplasty and preserved in liquid nitrogen until use. Mean age of the patients (21 males, 9 females) was 24.8 ± 14.1 years. All subjects completed a questionnaire, underwent a skin prick test, and contributed a sample for laboratory analyses of parameters including serum IgE level and eosinophil count. AR was confirmed by presence of typical symptoms and result of skin prick test. This study was approved by the Internal Review Board of Dankook University Hospital.
The questionnaire included a list of nine symptoms that were generally characteristic of AR or rhinoconjunctivitis: runny nose, sneezing, blocked nose, itchy nose, itchy eye and skin, skin eczema, dyspnea, wheezing and overall discomfort. The patients rate these symptoms by severity on a 6-point visual analogue scale from 0 (absent) to 5 (severe).
Skin prick test for 50 common aeroallergens were performed as part of the evaluation, with histamine phosphate (histamine base concentration, 1 mg/mL) and glycerinated phenol saline as controls. All tests were performed by a standard single-headed lancet technique and test results were read by a single experienced technician who was blinded to the clinical symptoms. The aeroallergens included house dust mite (mix), mixed feathers, cockroach, cat, dog, molds (Aspergillus, Alternaria, Mucor, Rhizopus, Trichophyton and Penicillium) and pollens common to the country (tree pollens - B3, Alder, Elder, Hazel, Poplar, Elm, Willow, Ash, Birch, Beech, Oak and Plane; grass pollens - B2, Cocksfoot, Maize, Ryegrass, Orchard and Timothy; and weeds - Dandelion, Mugwort, Ragweed, Plantain and Hop Japanese). For each allergen, the largest diameter of the wheal and the diameter orthogonal to it were measured, and the mean was calculated. A positive reaction was defined as a mean weal diameter more than or equal to that of histamine (positive control). All the saline controls were negative. Patients were considered allergic if they had at least one positive skin prick test to any of the allergens tested and we selected patients who were sensitive to house dust mite.
Total RNA was prepared from the nasal mucosa of the inferior turbinate with TriZol Reagent (Invitrogen, Carlsbad, CA, USA). Complementary DNA (cDNA) was synthesized using Superscript reverse transcriptase (Invitrogen) and oligo (dT) primers (Fermentas, Burlington, ON, Canada). For analysis of transcriptional factors, the following TaqMan® primers and probes were purchased from Applied Biosystems (Foster City, CA, USA), GATA-3 (Hs00231122_m1), T-bet (Hs00203436_m1), forkhead box P3 (Foxp3; Hs01085834_m1), RAR-related orphan receptor C (RORC; Hs01076112_m1), glyceraldehyde 3-phosphate dehydrogenase (GAPDH; Hs03929097_g1) and Pre-Developed Assay Reagent. Amplification of GATA-3, T-bet, Foxp3, RORC and GAPDH cDNA was carried out in MicroAmp optical 96-well reaction plates (Applied Biosystems). The reaction was performed using an ABI StepOnePlus Sequence Detection System (Applied Biosystems). The average transcript levels of genes were then normalized to GAPDH.
mRNA expression levels were compared between the control and allergy groups, and between mild and moderate-to-severe groups. Clinical data such as severity of allergic symptoms, IgE levels, eosinophil counts and grade of skin prick test were compared with mRNA expression levels of transcription factors using correlation analysis. Mann-Whitney test was used to analyze differences between groups and correlation analysis was performed to evaluate the relationship between transcription factors and other clinical features. All parametric results were expressed as mean ± standard deviation. A statistical significance was assumed as p < 0.05 for all parameters.
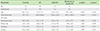
The patient characteristics are shown in Table 1. There were 12 control subjects and 18 subjects with AR. Of the latter 18, eight subjects had mild AR and 10 had moderate-to-severe AR according to the Allergic Rhinitis and its Impact on Asthma (ARIA) classification. Only 1 subject had intermittent AR and 17 had persistent AR. There were no significant differences in age and male-to-female ratio among groups, although control subjects had higher mean age than AR subjects. Total IgE level showed significant differences between control and AR group (p < 0.001) and between mild AR and moderate-to-severe AR group (p < 0.001). The symptom score also showed significant differences among groups except nasal obstruction. The control subjects had lower symptom scores in rhinorrhea, sneezing and itching than AR group and mild AR group, had lower symptoms than the moderate-to-severe AR group, as expected (Table 1).
The average mRNA expression level of T-bet in the control and AR groups were 1.25 ± 1.59 and 1.73 ± 1.42, respectively, with no significant difference between them (p = 0.31). The expression levels of the Th2 transcription factor, GATA3, were 0.27 ± 0.42 (control group) and 0.62 ± 0.68 (AR group); the difference was significant (p = 0.024). With regard to the Th17 transcription factor, RORC, the control group displayed a significantly lower expression level (0.16 ± 0.18) compared to the AR group (0.39 ± 0.41), and the difference was significant (p = 0.043). The expression levels of Foxp3, the Treg transcription factor, were 2.39 ± 1.32 in the control group and 1.25 ± 0.56 in the AR group; the difference was significant (p = 0.039) (Fig. 1).
The gene expression levels between mild AR and moderate to severe AR group were also analyzed. The expression levels in GATA3 and RORC between those two groups showed significant differences (p = 0.032 and p = 0.049). However, the expression level of T-bet did not show any significant difference between two groups (p = 0.13), although moderate-to-severe AR group had higher gene expression level. The expression level in Foxp3 between mild and moderate to severe AR group did not show a significant difference (p = 0.73) (Fig. 2).
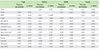
Correlation analysis was per formed to investigate the relationship between transcriptional factors and clinical findings. All the transcriptional factors did not show any significant correlations with clinical symptoms such as sneezing, nasal obstruction, nasal itching, rhinorrhea, dyspnea, wheezing and nasal discomfort. One significant finding was that GATA3 and RORC expression were significantly correlated with each other (p < 0.001, r = 0.94) and with total IgE level (p = 0.001, r = 0.62 and p = 0.002, r = 0.56 respectively, Table 2), suggesting that Th2 and Th17 transcription factors might play an important role in production of IgE. Another interesting finding was the correlation of Foxp3 and blood white blood cell count (p = 0.005, r = 0.56).
The recently recognized Th17 and Treg cell subsets were known to play an important role in autoimmune disease. In this study, we tried to reveal the role of these T cell subsets in AR. The results indicate the possibility of the involvement of Th2, Th17 and Treg cell subsets in pathogenesis of AR.
Before the discovery of the Th17 subset, Th2 cells or the Th1/Th2 balance were recognized as being important in the pathogenesis of allergic disease. The discovery of Th17 and Treg cells expanded the understanding of pathogenesis of immunologic diseases including AR. Th17 cells were first identified as IL-17 producing cells in 2000 [3] and its transcriptional factor of mouse, RORγt, was discovered in 2006 [4]. Its major role in autoimmune disease has been extensively studied and its contribution in allergic disease is still under investigation. In asthmatic patients, expression of IL-17 mRNA and proteins are increased in the lungs, sputum, bronchoalveolar lavage fluid and sera [5-7], and RORC mRNA expression is increased in peripheral blood mononuclear cells (PBMC) [8], implying a contribution of Th17 subset to the pathogenesis of allergic diseases.
In terms of AR, although several studies indicated the possibility of involvement of Th17 cells in the pathogenesis of AR [1], the role of Th17 cells is still controversial in the absence of detailed data. A recent study reported increased serum IL-17 levels in the most severe cases of birch allergy, which were significantly related to clinical symptoms of AR [9, 10], suggesting a possible association of the Th17 cell subset with AR pathogenesis. Presently, the RORC level of nasal mucosa was increased in the AR group compared with the control group, in a manner that was consistent with other allergic diseases such as asthma or atopic dermatitis. However, another recent study reported that RORC expression of the nasal mucosa did not differ between control and AR subjects, although RORC levels were higher in the persistent AR group [11]. The loss of statistical significance in the previous study may have reflected the lower sample numbers in their study. In addition, the expression level of RORC was different in terms of severity of AR and there was no significant difference between control and mild AR group in our study. Only severe AR group had increased expression of RORC, suggesting a broad overlap of transcriptional level of RORC between control and AR group. A better designed study will be needed to resolve the discrepancy in findings.
Presently, Foxp3 mRNA expression in AR subjects was decreased. These findings are consistent with a prior report of decreased Foxp3 mRNA expression both in nasal tissue and PBMCs in AR patients [12] and the decreased expression of Foxp3 mRNA in nasal secretions from patients with AR [13]. Several studies from asthmatic patients also reported decreased Foxp3 expression and fewer Treg in asthmatics [14-16], implying a critical role of Treg in dampening allergic response.
mRNA expression of transcriptional factors were compared between mild group and moderate to severe group according to ARIA classification. Expressions of GATA3 and RORC showed significant differences according to severity of AR, whereas expressions of T-bet and Foxp3 did not show any significant differences between severity groups. In mild group, expression of T-bet, GATA3 and RORC were almost similar to that of control group, suggesting that the severity of AR influence expression of transcriptional factors.
The comparison of clinical parameters with mRNA expression level revealed several interesting findings. One was the correlation between GATA3 and RORC. Both Th2 and Th17 subsets play important roles in allergic disease, and GATA3 and RORC share the common transcriptional factor, IRF4 [17], implying that plasticity between the development and maintenance of Th2 and Th17 cells may exist. Supporting this, it has been reported that Th2 cells that produce IL-17 cytokine exist with co-expression of GATA3 and RORC [18]. These findings suggest a close relationship between Th2 and Th17 cells, including the possibility that the cell types might change with each other under some circumstances. These findings support our data that the expression level of GATA3 and RORC correlate with each other and provide some clues in the interpretation of our data.
The other finding of note is the correlation of RORC with the IgE level, which also can be interpreted in the context of correlation between GATA3 and RORC. In allergic asthma, some studies showed that patients with hyper-IgE syndrome have impaired Th17 differentiation [19, 20], indicating an association of Th17 cells with serum levels of IgE.
This study, however, has some limitations. First, limited numbers of subjects were included. Therefore, a more sophisticated study will be needed to draw a more detailed conclusion. Second, we used nonallergic patients with turbinate hypertrophy as control subjects. Since it was difficult to obtain samples from normal subjects without symptoms, nonallergic controls were used instead. Third, the age of control group was significantly higher than those of AR group and it might influence the results of this study, although it is less likely. In spite of these limitations, the present study provides novel information about activation of transcription factors of T cell subsets in AR and helps to understand the pathophysiology of AR in terms of T cell subsets.
In conclusion, increased mRNA expression of GATA3 (Th2) and RORC (Th17), and decreased expression of Foxp3 (Treg) might play important roles in pathogenesis of AR, and both GATA3 and RORC may be closely related with IgE production.
Figures and Tables
 | Fig. 1mRNA levels for GATA-3, Foxp3, RORC and T-bet transcription factors measured in nasal tissues of control and patients with AR. mRNA concentrations were standardized against the levels of GAPDH housekeeping gene. The significance level was set at a value of 0.05.
*p < 0.05.
Foxp3, forkhead box P3; RORC, retinoic acid-related orphan receptor C; AR, allergic rhinitis; GAPDH, glyceraldehyde 3-phosphate dehydrogenase.
|
 | Fig. 2mRNA levels for GATA-3, Foxp3, RORC and T-bet transcription factors measured in nasal tissues of control, patients with mild AR (mild) and moderate-to-severe AR (severe). mRNA concentrations were standardized against the levels of b-actin housekeeping gene. The significance level was set at a value of 0.05.
*p < 0.05.
Foxp3, forkhead box P3; RORC, retinoic acid-related orphan receptor C; AR, allergic rhinitis.
|
ACKNOWLEDGEMENTS
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (No. 2011-0013964).
References
2. Nouri-Aria KT, Durham SR. Regulatory T cells and allergic disease. Inflamm Allergy Drug Targets. 2008; 7:237–252.

3. Infante-Duarte C, Horton HF, Byrne MC, Kamradt T. Microbial lipopeptides induce the production of IL-17 in Th cells. J Immunol. 2000; 165:6107–6115.

4. Ivanov II, McKenzie BS, Zhou L, Tadokoro CE, Lepelley A, Lafaille JJ, Cua DJ, Littman DR. The orphan nuclear receptor RORgammat directs the differentiation program of proinflammatory IL-17+ T helper cells. Cell. 2006; 126:1121–1133.
5. Wong CK, Ho CY, Ko FW, Chan CH, Ho AS, Hui DS, Lam CW. Proinflammatory cytokines (IL-17, IL-6, IL-18 and IL-12) and Th cytokines (IFN-gamma, IL-4, IL-10 and IL-13) in patients with allergic asthma. Clin Exp Immunol. 2001; 125:177–183.
6. Molet S, Hamid Q, Davoine F, Nutku E, Taha R, Pagé N, Olivenstein R, Elias J, Chakir J. IL-17 is increased in asthmatic airways and induces human bronchial fibroblasts to produce cytokines. J Allergy Clin Immunol. 2001; 108:430–438.

7. Barczyk A, Pierzchala W, Sozañska E. Interleukin-17 in sputum correlates with airway hyperresponsiveness to methacholine. Respir Med. 2003; 97:726–733.

8. Zhao Y, Yang J, Gao YD, Guo W. Th17 immunity in patients with allergic asthma. Int Arch Allergy Immunol. 2010; 151:297–307.

9. Ciprandi G, De Amici M, Murdaca G, Fenoglio D, Ricciardolo F, Marseglia G, Tosca M. Serum interleukin-17 levels are related to clinical severity in allergic rhinitis. Allergy. 2009; 64:1375–1378.

10. Ciprandi G, Fenoglio D, De Amici M, Quaglini S, Negrini S, Filaci G. Serum IL-17 levels in patients with allergic rhinitis. J Allergy Clin Immunol. 2008; 122:650–651.e2.

11. Liu F, Zhang J, Liu Y, Zhang N, Holtappels G, Lin P, Liu S, Bachert C. Inflammatory profiles in nasal mucosa of patients with persistent vs intermittent allergic rhinitis. Allergy. 2010; 65:1149–1157.
12. Xu G, Mou Z, Jiang H, Cheng L, Shi J, Xu R, Oh Y, Li H. A possible role of CD4+CD25+ T cells as well as transcription factor Foxp3 in the dysregulation of allergic rhinitis. Laryngoscope. 2007; 117:876–880.

13. Lee SM, Gao B, Dahl M, Calhoun K, Fang D. Decreased FoxP3 gene expression in the nasal secretions from patients with allergic rhinitis. Otolaryngol Head Neck Surg. 2009; 140:197–201.

14. Akdis M, Verhagen J, Taylor A, Karamloo F, Karagiannidis C, Crameri R, Thunberg S, Deniz G, Valenta R, Fiebig H, Kegel C, Disch R, Schmidt-Weber CB, Blaser K, Akdis CA. Immune responses in healthy and allergic individuals are characterized by a fine balance between allergen-specific T regulatory 1 and T helper 2 cells. J Exp Med. 2004; 199:1567–1575.

15. Shi HZ, Li S, Xie ZF, Qin XJ, Qin X, Zhong XN. Regulatory CD4+CD25+ T lymphocytes in peripheral blood from patients with atopic asthma. Clin Immunol. 2004; 113:172–178.

16. Ling EM, Smith T, Nguyen XD, Pridgeon C, Dallman M, Arbery J, Carr VA, Robinson DS. Relation of CD4+CD25+ regulatory T-cell suppression of allergen-driven T-cell activation to atopic status and expression of allergic disease. Lancet. 2004; 363:608–615.

17. Brüstle A, Heink S, Huber M, Rosenplänter C, Stadelmann C, Yu P, Arpaia E, Mak TW, Kamradt T, Lohoff M. The development of inflammatory T(H)-17 cells requires interferon-regulatory factor 4. Nat Immunol. 2007; 8:958–966.

18. Wang YH, Voo KS, Liu B, Chen CY, Uygungil B, Spoede W, Bernstein JA, Huston DP, Liu YJ. A novel subset of CD4(+) T(H)2 memory/effector cells that produce inflammatory IL-17 cytokine and promote the exacerbation of chronic allergic asthma. J Exp Med. 2010; 207:2479–2491.

19. Milner JD, Brenchley JM, Laurence A, Freeman AF, Hill BJ, Elias KM, Kanno Y, Spalding C, Elloumi HZ, Paulson ML, Davis J, Hsu A, Asher AI, O'Shea J, Holland SM, Paul WE, Douek DC. Impaired T(H)17 cell differentiation in subjects with autosomal dominant hyper-IgE syndrome. Nature. 2008; 452:773–776.

20. Al Khatib S, Keles S, Garcia-Lloret M, Karakoc-Aydiner E, Reisli I, Artac H, Camcioglu Y, Cokugras H, Somer A, Kutukculer N, Yilmaz M, Ikinciogullari A, Yegin O, Yüksek M, Genel F, Kucukosmanoglu E, Baki A, Bahceciler NN, Rambhatla A, Nickerson DW, McGhee S, Barlan IB, Chatila T. Defects along the T(H)17 differentiation pathway underlie genetically distinct forms of the hyper IgE syndrome. J Allergy Clin Immunol. 2009; 124:342–348. 348.e1–348.e5.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download