1. Schildcrout JS, Sheppard L, Lumley T, Slaughter JC, Koenig JQ, Shapiro GG. Ambient air pollution and asthma exacerbations in children: an eight-city analysis. Am J Epidemiol. 2006; 164:505–517. PMID:
16798793.

2. Samoli E, Nastos PT, Paliatsos AG, Katsouyanni K, Priftis KN. Acute effects of air pollution on pediatric asthma exacerbation: evidence of association and effect modification. Environ Res. 2011; 111:418–424. PMID:
21296347.

3. Chauhan AJ, Johnston SL. Air pollution and infection in respiratory illness. Br Med Bull. 2003; 68:95–112. PMID:
14757711.

4. Goings SA, Kulle TJ, Bascom R, Sauder LR, Green DJ, Hebel JR, Clements ML. Effect of nitrogen dioxide exposure on susceptibility to influenza A virus infection in healthy adults. Am Rev Respir Dis. 1989; 139:1075–1081. PMID:
2712434.

5. Holloway JW, Savarimuthu Francis S, Fong KM, Yang IA. Genomics and the respiratory effects of air pollution exposure. Respirology. 2012; 17:590–600. PMID:
22404320.

6. Koppelman GH, Nawijn MC. Recent advances in the epigenetics and genomics of asthma. Curr Opin Allergy Clin Immunol. 2011; 11:414–419. PMID:
21841472.

7. Crompton P, Wu Y. Energy consumption in China: past trends and future directions. Energy Economics. 2005; 27:195–208.

8. Mishra V. Effect of indoor air pollution from biomass combustion on prevalence of asthma in the elderly. Environ Health Perspect. 2003; 111:71–78. PMID:
12515681.

9. Modig L, Torén K, Janson C, Jarvholm B, Forsberg B. Vehicle exhaust outside the home and onset of asthma among adults. Eur Respir J. 2009; 33:1261–1267. PMID:
19251785.

10. Shah SD, Cocker DR 3rd, Miller JW, Norbeck JM. Emission rates of particulate matter and elemental and organic carbon from in-use diesel engines. Environ Sci Technol. 2004; 38:2544–2550. PMID:
15180049.

11. Riedl M, Diaz-Sanchez D. Biology of diesel exhaust effects on respiratory function. J Allergy Clin Immunol. 2005; 115:221–228. PMID:
15696072.

12. Takafuji S, Suzuki S, Koizumi K, Tadokoro K, Miyamoto T, Ikemori R, Muranaka M. Diesel-exhaust particulates inoculated by the intranasal route have an adjuvant activity for IgE production in mice. J Allergy Clin Immunol. 1987; 79:639–645. PMID:
2435776.

13. Diaz-Sanchez D, Tsien A, Casillas A, Dotson AR, Saxon A. Enhanced nasal cytokine production in human beings after in vivo challenge with diesel exhaust particles. J Allergy Clin Immunol. 1996; 98:114–123. PMID:
8765825.
14. Sasaki Y, Ohtani T, Ito Y, Mizuashi M, Nakagawa S, Furukawa T, Horii A, Aiba S. Molecular events in human T cells treated with diesel exhaust particles or formaldehyde that underlie their diminished interferon-gamma and interleukin-10 production. Int Arch Allergy Immunol. 2009; 148:239–250. PMID:
18849615.

15. Gilmour MI, Jaakkola MS, London SJ, Nel AE, Rogers CA. How exposure to environmental tobacco smoke, outdoor air pollutants, and increased pollen burdens influences the incidence of asthma. Environ Health Perspect. 2006; 114:627–633. PMID:
16581557.

16. Gupta D, Aggarwal AN, Chaudhry K, Chhabra SK, D'Souza GA, Jindal SK, Katiyar SK, Kumar R, Shah B, Vijayan VK. Household environmental tobacco smoke exposure, respiratory symptoms and asthma in non-smoker adults: a multicentric population study from India. Indian J Chest Dis Allied Sci. 2006; 48:31–36. PMID:
16482949.
17. Feng Y, Kong Y, Barnes PF, Huang FF, Klucar P, Wang X, Samten B, Sengupta M, Machona B, Donis R, Tvinnereim AR, Shams H. Exposure to cigarette smoke inhibits the pulmonary T-cell response to influenza virus and Mycobacterium tuberculosis. Infect Immun. 2011; 79:229–237. PMID:
20974820.
18. Hogan AE, Corrigan MA, O'Reilly V, Gaoatswe G, O'Connell J, Doherty DG, Lynch L, O'Shea D. Cigarette smoke alters the invariant natural killer T cell function and may inhibit anti-tumor responses. Clin Immunol. 2011; 140:229–235. PMID:
21684213.

19. Crinnion WJ. Do environmental toxicants contribute to allergy and asthma? Altern Med Rev. 2012; 17:6–18. PMID:
22502619.
20. Zheng L, Dong GH, Zhang YH, Liang ZF, Jin YH, He QC. Type 1 and Type 2 cytokines imbalance in adult male C57BL/6 mice following a 7-day oral exposure to perfluorooctanesulfonate (PFOS). J Immunotoxicol. 2011; 8:30–38. PMID:
21299352.

21. Bornehag CG, Sundell J, Weschler CJ, Sigsgaard T, Lundgren B, Hasselgren M, Hägerhed-Engman L. The association between asthma and allergic symptoms in children and phthalates in house dust: a nested case-control study. Environ Health Perspect. 2004; 112:1393–1397. PMID:
15471731.

22. Newton AP, Cadena SM, Rocha ME, Carnieri EG, Martinelli de Oliveira MB. Effect of triclosan (TRN) on energy-linked functions of rat liver mitochondria. Toxicol Lett. 2005; 160:49–59. PMID:
16023799.

23. Lehmann I, Rehwagen M, Diez U, Seiffart A, Rolle-Kampczyk U, Richter M, Wetzig H, Borte M, Herbarth O. Enhanced in vivo IgE production and T cell polarization toward the type 2 phenotype in association with indoor exposure to VOC: results of the LARS study. Int J Hyg Environ Health. 2001; 204:211–221. PMID:
11833293.

24. Duramad P, Harley K, Lipsett M, Bradman A, Eskenazi B, Holland NT, Tager IB. Early environmental exposures and intracellular Th1/Th2 cytokine profiles in 24-month-old children living in an agricultural area. Environ Health Perspect. 2006; 114:1916–1922. PMID:
17185285.

25. Reichrtová E, Ciznár P, Prachar V, Palkovicová L, Veningerová M. Cord serum immunoglobulin E related to the environmental contamination of human placentas with organochlorine compounds. Environ Health Perspect. 1999; 107:895–899. PMID:
10544157.

26. Whalen MM, Loganathan BG, Yamashita N, Saito T. Immunomodulation of human natural killer cell cytotoxic function by triazine and carbamate pesticides. Chem Biol Interact. 2003; 145:311–319. PMID:
12732457.

27. Eder W, Ege MJ, von Mutius E. The asthma epidemic. N Engl J Med. 2006; 355:2226–2235. PMID:
17124020.

28. Lipsett M, Hurley S, Ostro B. Air pollution and emergency room visits for asthma in Santa Clara County, California. Environ Health Perspect. 1997; 105:216–222. PMID:
9105797.

29. Gauderman WJ, Avol E, Lurmann F, Kuenzli N, Gilliland F, Peters J, McConnell R. Childhood asthma and exposure to traffic and nitrogen dioxide. Epidemiology. 2005; 16:737–743. PMID:
16222162.

30. Tunnicliffe WS, Burge PS, Ayres JG. Effect of domestic concentrations of nitrogen dioxide on airway responses to inhaled allergen in asthmatic patients. Lancet. 1994; 344:1733–1736. PMID:
7997002.

31. Strand V, Svartengren M, Rak S, Barck C, Bylin G. Repeated exposure to an ambient level of NO2 enhances asthmatic response to a nonsymptomatic allergen dose. Eur Respir J. 1998; 12:6–12. PMID:
9701406.
32. Lin S, Liu X, Le LH, Hwang SA. Chronic exposure to ambient ozone and asthma hospital admissions among children. Environ Health Perspect. 2008; 116:1725–1730. PMID:
19079727.

33. Meng YY, Rull RP, Wilhelm M, Lombardi C, Balmes J, Ritz B. Outdoor air pollution and uncontrolled asthma in the San Joaquin Valley, California. J Epidemiol Community Health. 2010; 64:142–147. PMID:
20056967.

34. Gent JF, Triche EW, Holford TR, Belanger K, Bracken MB, Beckett WS, Leaderer BP. Association of low-level ozone and fine particles with respiratory symptoms in children with asthma. JAMA. 2003; 290:1859–1867. PMID:
14532314.

35. Just J, Ségala C, Sahraoui F, Priol G, Grimfeld A, Neukirch F. Short-term health effects of particulate and photochemical air pollution in asthmatic children. Eur Respir J. 2002; 20:899–906. PMID:
12412681.

36. Penttinen P, Vallius M, Tiittanen P, Ruuskanen J, Pekkanen J. Source-specific fine particles in urban air and respiratory function among adult asthmatics. Inhal Toxicol. 2006; 18:191–198. PMID:
16399661.

37. Pan G, Zhang S, Feng Y, Takahashi K, Kagawa J, Yu L, Wang P, Liu M, Liu Q, Hou S, Pan B, Li J. Air pollution and children's respiratory symptoms in six cities of Northern China. Respir Med. 2010; 104:1903–1911. PMID:
20801627.

38. Zhao Z, Zhang Z, Wang Z, Ferm M, Liang Y, Norbäck D. Asthmatic symptoms among pupils in relation to winter indoor and outdoor air pollution in schools in Taiyuan, China. Environ Health Perspect. 2008; 116:90–97. PMID:
18197305.

39. Park JK, Kim YK, Lee SR, Cho SH, Min KU, Kim YY. Repeated exposure to low levels of sulfur dioxide (SO2) enhances the development of ovalbumin-induced asthmatic reactions in guinea pigs. Ann Allergy Asthma Immunol. 2001; 86:62–67. PMID:
11206242.

40. McCreanor J, Cullinan P, Nieuwenhuijsen MJ, Stewart-Evans J, Malliarou E, Jarup L, Harrington R, Svartengren M, Han IK, Ohman-Strickland P, Chung KF, Zhang J. Respiratory effects of exposure to diesel traffic in persons with asthma. N Engl J Med. 2007; 357:2348–2358. PMID:
18057337.

41. Kim SY, O'Neill MS, Lee JT, Cho Y, Kim J, Kim H. Air pollution, socioeconomic position, and emergency hospital visits for asthma in Seoul, Korea. Int Arch Occup Environ Health. 2007; 80:701–710. PMID:
17357797.

42. Jeong SH, Kim JH, Son BK, Hong SC, Kim SY, Lee GH, Lim DH. Comparison of air pollution and the prevalence of allergy-related diseases in Incheon and Jeju City. Korean J Pediatr. 2011; 54:501–506. PMID:
22323906.

43. Kim SH, Son JY, Lee JT, Kim TB, Park HW, Lee JH, Kim TH, Sohn JW, Shin DH, Park SS, Yoon HJ. Effect of air pollution on acute exacerbation of adult asthma in Seoul, Korea: A case-crossover study. Korean J Med. 2010; 78:450–456.
44. Chen CH, Xirasagar S, Lin HC. Seasonality in adult asthma admissions, air pollutant levels, and climate: a population-based study. J Asthma. 2006; 43:287–292. PMID:
16809242.

45. Chen BY, Chan CC, Lee CT, Cheng TJ, Huang WC, Jhou JC, Han YY, Chen CC, Guo YL. The association of ambient air pollution with airway inflammation in schoolchildren. Am J Epidemiol. 2012; 175:764–774. PMID:
22408045.

46. Wong GW, Ko FW, Lau TS, Li ST, Hui D, Pang SW, Leung R, Fok TF, Lai CK. Temporal relationship between air pollution and hospital admissions for asthmatic children in Hong Kong. Clin Exp Allergy. 2001; 31:565–569. PMID:
11359423.

47. Ko FW, Tam W, Wong TW, Lai CK, Wong GW, Leung TF, Ng SS, Hui DS. Effects of air pollution on asthma hospitalization rates in different age groups in Hong Kong. Clin Exp Allergy. 2007; 37:1312–1319. PMID:
17845411.

48. Cai H, Xie S. Traffic-related air pollution modeling during the 2008 Beijing Olympic Games: the effects of an odd-even day traffic restriction scheme. Sci Total Environ. 2011; 409:1935–1948. PMID:
21353290.

49. Li Y, Wang W, Kan H, Xu X, Chen B. Air quality and outpatient visits for asthma in adults during the 2008 Summer Olympic Games in Beijing. Sci Total Environ. 2010; 408:1226–1227. PMID:
19959207.

50. Romieu I, Barraza-Villarreal A, Escamilla-Nuez C, Almstrand AC, Diaz-Sanchez D, Sly PD, Olin AC. Exhaled breath malondialdehyde as a marker of effect of exposure to air pollution in children with asthma. J Allergy Clin Immunol. 2008; 121:903–909.e906. PMID:
18234317.

51. Brauer M, Hoek G, Smit HA, de Jongste JC, Gerritsen J, Postma DS, Kerkhof M, Brunekreef B. Air pollution and development of asthma, allergy and infections in a birth cohort. Eur Respir J. 2007; 29:879–888. PMID:
17251230.

52. Ryan PH, Bernstein DI, Lockey J, Reponen T, Levin L, Grinshpun S, Villareal M, Hershey GK, Burkle J, LeMasters G. Exposure to traffic-related particles and endotoxin during infancy is associated with wheezing at age 3 years. Am J Respir Crit Care Med. 2009; 180:1068–1075. PMID:
19745206.

53. Gehring U, Wijga AH, Brauer M, Fischer P, de Jongste JC, Kerkhof M, Oldenwening M, Smit HA, Brunekreef B. Traffic-related air pollution and the development of asthma and allergies during the first 8 years of life. Am J Respir Crit Care Med. 2010; 181:596–603. PMID:
19965811.

54. Künzli N, Bridevaux PO, Liu LJ, Garcia-Esteban R, Schindler C, Gerbase MW, Sunyer J, Keidel D, Rochat T. Traffic-related air pollution correlates with adult-onset asthma among never-smokers. Thorax. 2009; 64:664–670. PMID:
19359271.

55. Bråbäck L, Forsberg B. Does traffic exhaust contribute to the development of asthma and allergic sensitization in children: findings from recent cohort studies. Environ Health. 2009; 8:17. PMID:
19371435.

56. Watts J. Doctors blame air pollution for China's asthma increases. Lancet. 2006; 368:719–720. PMID:
16938905.

57. Hwang BF, Lee YL, Lin YC, Jaakkola JJ, Guo YL. Traffic related air pollution as a determinant of asthma among Taiwanese school children. Thorax. 2005; 60:467–473. PMID:
15923246.

58. Shima M, Nitta Y, Ando M, Adachi M. Effects of air pollution on the prevalence and incidence of asthma in children. Arch Environ Health. 2002; 57:529–535. PMID:
12696649.

59. Shima M, Nitta Y, Adachi M. Traffic-related air pollution and respiratory symptoms in children living along trunk roads in Chiba Prefecture, Japan. J Epidemiol. 2003; 13:108–119. PMID:
12675120.

60. Ho WC, Hartley WR, Myers L, Lin MH, Lin YS, Lien CH, Lin RS. Air pollution, weather, and associated risk factors related to asthma prevalence and attack rate. Environ Res. 2007; 104:402–409. PMID:
17316602.

61. Guo YL, Lin YC, Sung FC, Huang SL, Ko YC, Lai JS, Su HJ, Shaw CK, Lin RS, Dockery DW. Climate, traffic-related air pollutants, and asthma prevalence in middle-school children in Taiwan. Environ Health Perspect. 1999; 107:1001–1006. PMID:
10585904.

62. Mösges R, Klimek L. Today's allergic rhinitis patients are different: new factors that may play a role. Allergy. 2007; 62:969–975. PMID:
17686101.

63. Morgenstern V, Zutavern A, Cyrys J, Brockow I, Gehring U, Koletzko S, Bauer CP, Reinhardt D, Wichmann HE, Heinrich J. Respiratory health and individual estimated exposure to traffic-related air pollutants in a cohort of young children. Occup Environ Med. 2007; 64:8–16. PMID:
16912084.

64. Morgenstern V, Zutavern A, Cyrys J, Brockow I, Koletzko S, Kärmer U, Behrendt H, Herbarth O, von Berg A, Bauer CP, Wichmann HE, Heinrich J. Atopic diseases, allergic sensitization, and exposure to traffic-related air pollution in children. Am J Respir Crit Care Med. 2008; 177:1331–1337. PMID:
18337595.

65. Bernstein DI. Diesel exhaust exposure, wheezing and sneezing. Allergy Asthma Immunol Res. 2012; 4:178–183. PMID:
22754710.

66. Hwang BF, Jaakkola JJ, Lee YL, Lin YC, Guo YL. Relation between air pollution and allergic rhinitis in Taiwanese schoolchildren. Respir Res. 2006; 7:23. PMID:
16469096.

67. Lee YL, Shaw CK, Su HJ, Lai JS, Ko YC, Huang SL, Sung FC, Guo YL. Climate, traffic-related air pollutants and allergic rhinitis prevalence in middle-school children in Taiwan. Eur Respir J. 2003; 21:964–970. PMID:
12797489.

68. Anderson HR, Ruggles R, Pandey KD, Kapetanakis V, Brunekreef B, Lai CK, Strachan DP, Weiland SK. Ambient particulate pollution and the world-wide prevalence of asthma, rhinoconjunctivitis and eczema in children: Phase One of the International Study of Asthma and Allergies in Childhood (ISAAC). Occup Environ Med. 2010; 67:293–300. PMID:
19819866.

69. Yura A, Shimizu T. Trends in the prevalence of atopic dermatitis in school children: longitudinal study in Osaka Prefecture, Japan, from 1985 to 1997. Br J Dermatol. 2001; 145:966–973. PMID:
11899151.

70. Lee JH, Kim J, Lee SW, Suh J, Yu JS, Park E, Lee J, Kim H, Lee KS, Chang EY, Cho JB, Kim KB, Han Y, Ahn K, Lee SI. The clinical effects of hospitalization in a low pollutant room on atopic dermatitis. Asia Pac Allergy. 2011; 1:87–92. PMID:
22053302.

71. Kim J, Kim EH, Oh I, Jung K, Han Y, Cheong HK, Ahn K. Symptoms of atopic dermatitis are influenced by outdoor air pollution. J Allergy Clin Immunol. 2013; [Epub ahead of print].

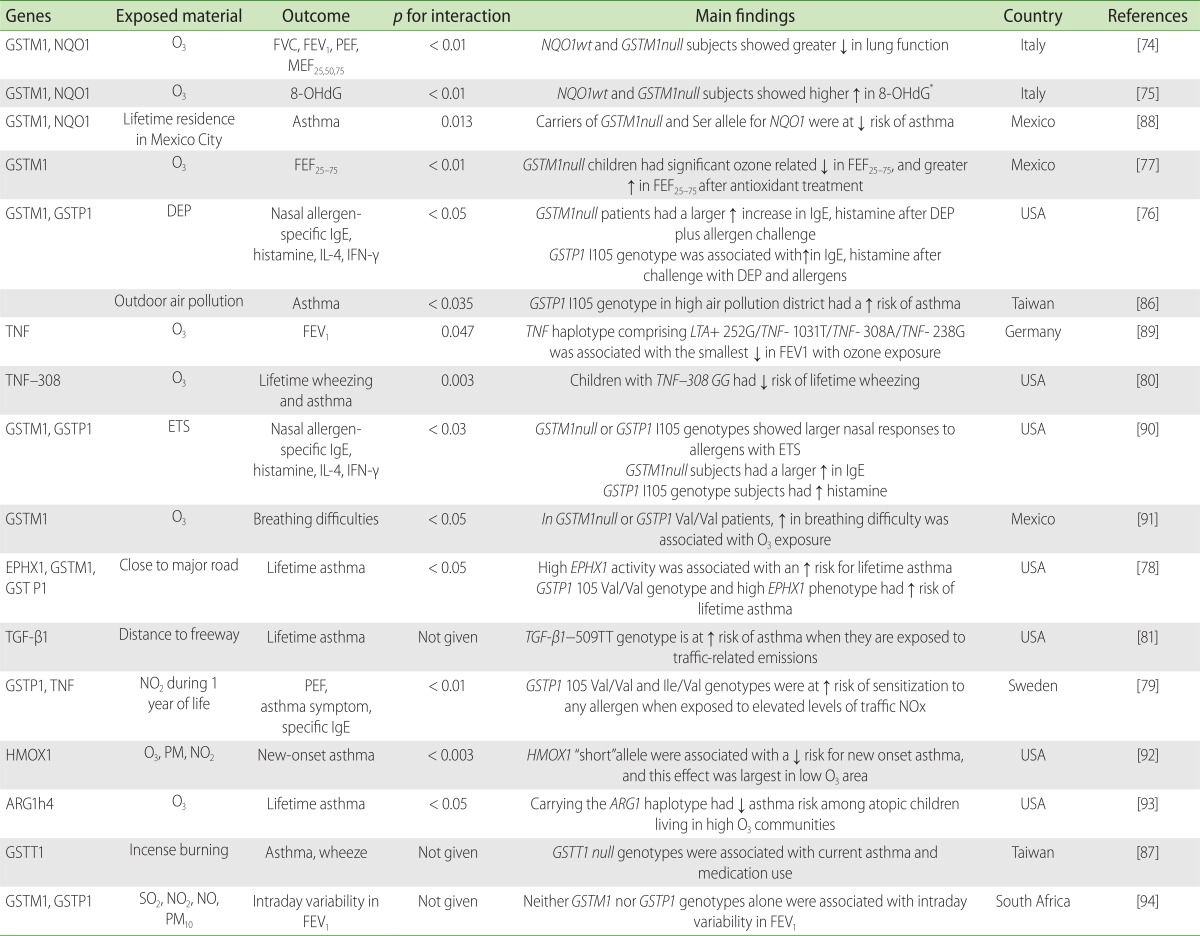
72. Carlsten C, Melén E. Air pollution, genetics, and allergy: an update. Curr Opin Allergy Clin Immunol. 2012; 12:455–460. PMID:
22885891.
73. Romieu I, Moreno-Macias H, London SJ. Gene by environment interaction and ambient air pollution. Proc Am Thorac Soc. 2010; 7:116–122. PMID:
20427582.

74. Bergamaschi E, De Palma G, Mozzoni P, Vanni S, Vettori MV, Broeckaert F, Bernard A, Mutti A. Polymorphism of quinone-metabolizing enzymes and susceptibility to ozone-induced acute effects. Am J Respir Crit Care Med. 2001; 163:1426–1431. PMID:
11371413.

75. Corradi M, Alinovi R, Goldoni M, Vettori M, Folesani G, Mozzoni P, Cavazzini S, Bergamaschi E, Rossi L, Mutti A. Biomarkers of oxidative stress after controlled human exposure to ozone. Toxicol Lett. 2002; 134:219–225. PMID:
12191881.

76. Gilliland FD, Li YF, Saxon A, Diaz-Sanchez D. Effect of glutathione-S-transferase M1 and P1 genotypes on xenobiotic enhancement of allergic responses: randomised, placebo-controlled crossover study. Lancet. 2004; 363:119–125. PMID:
14726165.

77. Romieu I, Sienra-Monge JJ, Ramírez-Aguilar M, Moreno-Macías H, Reyes-Ruiz NI, Estela del Río-Navarro B, Hernández-Avila M, London SJ. Genetic polymorphism of GSTM1 and antioxidant supplementation influence lung function in relation to ozone exposure in asthmatic children in Mexico City. Thorax. 2004; 59:8–10. PMID:
14694237.
78. Salam MT, Lin PC, Avol EL, Gauderman WJ, Gilliland FD. Microsomal epoxide hydrolase, glutathione S-transferase P1, traffic and childhood asthma. Thorax. 2007; 62:1050–1057. PMID:
17711870.

79. Melén E, Nyberg F, Lindgren CM, Berglind N, Zucchelli M, Nordling E, Hallberg J, Svartengren M, Morgenstern R, Kere J, Bellander T, Wickman M, Pershagen G. Interactions between glutathione S-transferase P1, tumor necrosis factor, and traffic-related air pollution for development of childhood allergic disease. Environ Health Perspect. 2008; 116:1077–1084. PMID:
18709160.
80. Li YF, Gauderman WJ, Avol E, Dubeau L, Gilliland FD. Associations of tumor necrosis factor G-308A with childhood asthma and wheezing. Am J Respir Crit Care Med. 2006; 173:970–976. PMID:
16456144.

81. Salam MT, Gauderman WJ, McConnell R, Lin PC, Gilliland FD. Transforming growth factor- 1 C-509T polymorphism, oxidant stress, and early-onset childhood asthma. Am J Respir Crit Care Med. 2007; 176:1192–1199. PMID:
17673695.
82. Runyon RS, Cachola LM, Rajeshuni N, Hunter T, Garcia M, Ahn R, Lurmann F, Krasnow R, Jack LM, Miller RL, Swan GE, Kohli A, Jacobson AC, Nadeau KC. Asthma discordance in twins is linked to epigenetic modifications of T cells. PLoS One. 2012; 7:e48796. PMID:
23226205.

83. Breton CV, Byun HM, Wenten M, Pan F, Yang A, Gilliland FD. Prenatal tobacco smoke exposure affects global and gene-specific DNA methylation. Am J Respir Crit Care Med. 2009; 180:462–467. PMID:
19498054.

84. Liu J, Ballaney M, Al-alem U, Quan C, Jin X, Perera F, Chen LC, Miller RL. Combined inhaled diesel exhaust particles and allergen exposure alter methylation of T helper genes and IgE production in vivo. Toxicol Sci. 2008; 102:76–81. PMID:
18042818.

85. Sofer T, Baccarelli A, Cantone L, Coull B, Maity A, Lin X, Schwartz J. Exposure to airborne particulate matter is associated with methylation pattern in the asthma pathway. Epigenomics. 2013; 5:147–154. PMID:
23566092.

86. Lee YL, Lin YC, Lee YC, Wang JY, Hsiue TR, Guo YL. Glutathione S-transferase P1 gene polymorphism and air pollution as interactive risk factors for childhood asthma. Clin Exp Allergy. 2004; 34:1707–1713. PMID:
15544594.

87. Wang IJ, Tsai CH, Chen CH, Tung KY, Lee YL. Glutathione S-transferase, incense burning and asthma in children. Eur Respir J. 2011; 37:1371–1377. PMID:
21109554.

88. David GL, Romieu I, Sienra-Monge JJ, Collins WJ, Ramirez-Aguilar M, del Rio-Navarro BE, Reyes-Ruiz NI, Morris RW, Marzec JM, London SJ. Nicotinamide adenine dinucleotide (phosphate) reduced:quinone oxidoreductase and glutathione S-transferase M1 polymorphisms and childhood asthma. Am J Respir Crit Care Med. 2003; 168:1199–1204. PMID:
12969868.

89. Yang IA, Holz O, Jörres RA, Magnussen H, Barton SJ, Rodríguez S, Cakebread JA, Holloway JW, Holgate ST. Association of tumor necrosis factor-alpha polymorphisms and ozone-induced change in lung function. Am J Respir Crit Care Med. 2005; 171:171–176. PMID:
15486341.
90. Gilliland FD, Li YF, Gong H Jr, Diaz-Sanchez D. Glutathione s-transferases M1 and P1 prevent aggravation of allergic responses by secondhand smoke. Am J Respir Crit Care Med. 2006; 174:1335–1341. PMID:
17023730.
91. Romieu I, Ramirez-Aguilar M, Sienra-Monge JJ, Moreno-Macas H, del Rio-Navarro BE, David G, Marzec J, Hernndez-Avila M, London S. GSTM1 and GSTP1 and respiratory health in asthmatic children exposed to ozone. Eur Respir J. 2006; 28:953–959. PMID:
16870661.

92. Islam T, McConnell R, Gauderman WJ, Avol E, Peters JM, Gilliland FD. Ozone, oxidant defense genes, and risk of asthma during adolescence. Am J Respir Crit Care Med. 2008; 177:388–395. PMID:
18048809.

93. Salam MT, Islam T, Gauderman WJ, Gilliland FD. Roles of arginase variants, atopy, and ozone in childhood asthma. J Allergy Clin Immunol. 2009; 123:596–602. 602.e1–602.e8. PMID:
19281908.

94. Reddy P, Naidoo RN, Robins TG, Mentz G, Li H, London SJ, Batterman S. GSTM1 and GSTP1 gene variants and the effect of air pollutants on lung function measures in South African children. Am J Ind Med. 2012; 55:1078–1086. PMID:
22228263.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download