Abstract
Many international and national asthma guidelines are now available in large parts of the world, but they are not yet implemented appropriately. There is a gap between scientific evidence-based medicine and real clinical practice. Implementation of guidelines is highly complex. Special strategies are needed to encourage guideline-based, high-quality care. It is important to understand the contents, the format, and the learning strategies which physicians prefer for the dissemination of guidelines. Physicians prefer more concise and immediately available guidelines that are practical to use. Thus, asthma guidelines should be disseminated as convenient and easily accessible tools. Various education programs and decision-support tools have been designed and applied to the clinical management of asthma to solve these challenging problems. Many of them have been shown to be effective at increasing physicians' knowledge and adherence to asthma guidelines and improving patients' clinical outcomes. These educational and decision-support tools are expected to contribute to a narrowing of the gap between asthma guidelines and practice/implementation of the guidelines.
Asthma is a global health problem with an increasing prevalence and an enormous disease burden [1, 2]. It is responsible for significant morbidity and mortality in both developed and developing countries [1]. Asthma treatment has seen great progress in recent decades. However, many patients with asthma still have frequent, uncontrolled symptoms and do not receive optimal care [3]. The translation of medical progress into high-quality practice and improved health outcomes is a big challenge for the near future.
Clinical practice guidelines (CPGs) are systematically developed statements designed to help practitioners and healthcare providers make appropriate decisions under specific medical circumstances [4]. Asthma-management guidelines have been developed since the late 1980s [5]. Many international and national guidelines in different languages are now available in large parts of the world, but they are not yet implemented appropriately [6-9]. Effective guideline dissemination requires that healthcare professionals be provided with adequate education and knowledge about self-management skills. Various educational programs and interventions have been performed to deliver evidence-based recommendations and improve physicians' knowledge about and attitude toward asthma management. Implementation of guidelines is highly complex, and special strategies are needed to encourage guideline-based, high-quality care [10]. In this article, recent progress in the development of educational and decision-support tools for asthma management will be reviewed, and effective strategies for disseminating and implementing guidelines will be discussed.
Since the initial guidelines were published in the late 1980s, asthma guidelines have taken on both regional approach and global approaches [5]. Local guidelines such as the Australian [11], Canadian [12], and British guidelines [13] were developed almost simultaneously between the late 1980s and early 1990s, and the National Asthma Education and Prevention Program (NAEPP) of the National Heart, Lung, and Blood Institute (NHLBI) of the US published the first expert panel report as a set of practical, comprehensive guidelines in 1991 [14]. During the same period, the Global Initiative for Asthma (GINA) program started to raise international awareness of asthma. The GINA program was launched as a collaboration between the World Health Organization (WHO) and the NHLBI, and its mission was to develop international asthma-management guidelines that could be customized or adapted to meet the needs and resources of local healthcare systems [15]. Owing to these global efforts, evidence-based asthma guidelines have been established and updated during the last two decades. Furthermore, many other countries have developed national guidelines written in their own languages and reflecting specific local circumstances and medical environments.
There have been many efforts to disseminate and implement guidelines at both global and local levels. GINA dissemination and implementation programs consist of multifaceted strategies that aim to reduce worldwide asthma mortality and morbidity [10, 16]. They include the GINA website, World Asthma Day, the GINA Assembly, regional initiatives, and GINA/WHO collaborations such as Global Alliance against Chronic Respiratory Diseases [16]. Locally adapted guidelines have been widely disseminated in multiple venues and using multiple formats, for example, publication in professional journals and books, lectures at multidisciplinary symposia, workshops, conferences attended by local experts and professionals, online information via websites, and efforts by the mass media to raise awareness of the key messages [16]. Recently, in diverse regions of the world, national asthma-management programs and projects have been carried out to achieve the global goal of controlling asthma through the dissemination and implementation of evidence-based guidelines [17, 18]. Furthermore, innovative interventions such as interactive educational programs were tested at the individual level [19, 20]. These interventions were reported to be effective for the dissemination of guidelines and delivery of adequate asthma care.
Despite these efforts, current implementation of asthma guidelines falls short of the optimal level and remains a challenge worldwide [3, 17]. There is a gap between scientific evidence-based medicine and real clinical practice, especially in primary care. Clinical practice guidelines have limited effects on general practitioners' behavior [21]. Many potential barriers exist. Accessibility of affordable drugs, costs of management, financial problems, local healthcare systems and infrastructures, reimbursement systems, local customs, and patients' and doctors' beliefs may affect the asthma care provided by healthcare providers [10, 21].
The GINA guidelines have adopted a control-based approach as a goal of asthma care and recommend that management should be based on achieving and maintaining complete asthma control [16]. The Gaining Optimal Asthma Control study and several other studies have demonstrated that good asthma control can be achieved through adequate pharmacological treatment in most patients [22-25]. However, an increasing body of evidence indicates that asthma is undertreated and uncontrolled in large numbers of patients in many parts of the world. Asthma insight and reality surveys around the world have shown that asthma care in the real world is far from ideal [3, 7, 26-29]. The first Asthma Insights and Reality survey in the Asia-Pacific region (AIRIAP) found that levels of control in the Asia-Pacific region fall markedly short of the goals of the GINA guidelines and that the guidelines were generally not being followed [30]. During the following 6 years, the situation did not change. The AIRIAP phase II survey showed that only 2.9% of patients had controlled asthma and that the majority of subjects did not reach the optimal control status [31].
To achieve the ultimate asthma-treatment goal, guideline-based management through, for example, regular monitoring of control status and adjustment of controller medication is needed. Physicians should be aware of the key concepts of guidelines and should adhere to the appropriate recommendations. It is not easy to increase physicians' knowledge or change their behavior [21, 32]. Continuous medical education and special educational strategies to encourage healthcare providers to follow the guidelines are essential to facilitate the dissemination and implementation of guidelines.
It is important for the dissemination of guidelines that the contents, format, and learning strategies that physicians prefer be understood. In our previous study [33], physicians were found to prefer immediately available information that described asthma medication, disease classification according to level of control, methods of patient evaluation, treatment, and monitoring, and management of acute exacerbation. These preferences reflect the need to facilitate rapid decision making in the clinical setting. Physicians required the guidelines to be presented in a practical and concise format such as algorithms, flowcharts, or flow diagrams. They preferred the guidelines to be presented on plastic sheets, in electronic medical records, and as pocket-sized cards. These findings indicate that the contents of asthma guidelines should be summarized and disseminated as convenient and easily accessible tools [33].
Continuing medical education (CME), such as lecture programs and discussions with colleagues, is an important learning strategy that physicians prefer and that helps to promote understanding of the recommendations [33]. Although few reports have described physicians' preference for guidelines, studies conducted by Stone et al. [34, 35] for pediatric asthma and other diseases revealed similar results to those noted above. Physicians seem to prefer more concise and immediately available guidelines that are practical to use.
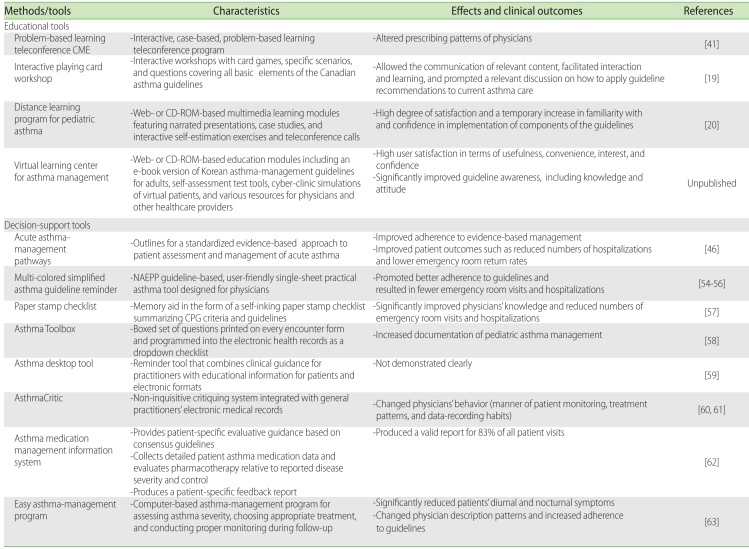
Asthma guideline education has positive effects on quality of asthma care and improves clinical outcomes [36]. However, compliance by primary care physicians with asthma guidelines and related education programs is known to be very low [37]. Many methods and strategies have been proposed to improve the efficiency of and compliance with education. The usefulness of various materials and tools developed for physician education has been assessed (Table 1). CME lectures, symposia, and seminars are classic educational methods that most physicians prefer [10, 38]. They afford good opportunities to deliver information on guideline-recommended diagnosis and treatment approaches and experts' opinions and recommendations [39, 40]. However, problem-based learning has been advocated as an approach to CME that is more effective than the traditional didactic lecture [41, 42]. Davis et al. [41] evaluated the effectiveness of an interactive, case-based, problem-based learning teleconference program for primary care physicians. This program significantly altered the prescribing patterns of physicians such that they adhered more closely to asthma guidelines. Problem-based learning facilitates better integration and rapid recall of information and leads to improvements in physicians' behavior and abilities.
Interactive and multifaceted education is known to be the most effective intervention among the various methods available [43, 44]. The ideal learning materials are customized to the specific needs of practitioners and are used in a way that is relevant to physicians' background and resources. Interactive education tools in various formats, such as card games [19], simulations [45], and computer-based programs [20], have been tested for their effectiveness in the dissemination of guideline-based asthma care. Boulet et al. [19] developed a card game that includes all the basic elements of the Canadian asthma guidelines and assessed its utility by inviting family physicians to an interactive card-playing workshop. This educational method allowed the communication of relevant content, facilitated interaction and learning, and prompted relevant discussion on how to apply guideline recommendations to current asthma care. It was well received by participants and improved knowledge transfer to caregivers [19].
As IT technology has advanced, new educational modalities based on the internet, computer programs, and IT communication have been developed. For example, Some CME programs [20] are being provided with internet-based, interactive modules or CD-ROM-based programs. Unlike traditional face-to-face or didactic lecture-type CME, internet or computer program-based CME offers opportunities to access CME remotely and to complete the education programs at one's own pace. Physicians have a greater choice of topics, content and settings and can access the information when they want. Le et al. [20] conducted a randomized controlled trial to assess the acceptability of a distance learning program for pediatric asthma and its effects on physician knowledge, attitude, and treatment practices. The program was composed of web- or CD-ROM-based multimedia learning modules and two teleconference calls. The modules featured narrated presentations, case studies, and interactive self-estimation exercises dealing with an overview of the NHLBI asthma guidelines and practical instructions for the treatment and management of patients with asthma. This pilot study revealed that pediatricians using this distance asthma learning program expressed a high degree of satisfaction and that the program was associated with a temporary increase in familiarity with and confidence in implementing components of the guidelines [20].
Recently, we developed a new interactive, virtual asthma guideline e-learning program named Virtual Learning Center for Asthma Management (VLCAM) (Fig. 1). VLCAM provides several education modules, including an e-book of Korean asthma-management guidelines for adults, self-assessment test tools, cyber-clinic simulations with virtual patients, and various resources for physicians and other healthcare providers. The most featured part of this program is the cyber-clinic simulations, which allow physicians to experience various clinical situations relating to the diagnosis, treatment, and monitoring of patients with asthma and management of acute asthma exacerbation in virtual patients. In our pilot survey of internal medicine resident trainees, user satisfaction with this program in terms of usefulness, convenience, interest, and confidence was high. All categories of guideline awareness, including knowledge, attitude, and practice, were significantly improved after learning with this program (unpublished work, in submission). Users can access this program by visiting several internet sites (www.kaaf.org, www.copd-asthma.co.kr) or by using a CD-ROM. It is expected to facilitate the dissemination of asthma guidelines and to contribute to improvements in knowledge and skills relating to asthma patient care in primary care physicians.
It is well documented that there is a large gap between knowledge of asthma care and actual clinical practice [3, 10, 17, 46]. Enhancing physicians' adherence to guidelines is important for the implementation of guidelines. Various tools to support the translation of knowledge into best practice have been designed and utilized (Table 1). The acute asthma-management pathway in the emergency department is a representative decision-support tool for guideline-based asthma management [46]. Clinical care maps and clinical pathways are tools that outline standardized, evidence-based approaches to patient assessment and management [46]. They can improve the continuity of care and effectively make management behavior more appropriate [47]. Numerous studies have shown that clinical pathways for acute asthma management improve adherence to evidence-based management as well as patient outcomes such as reduced hospitalization and lower emergency room return rates [48-52]. It has also been demonstrated that clinical pathways are useful tools for knowledge transfer and guideline implementation in both pediatric and adult asthma [49, 53].
Reminders and preprinted orders in various formats have also been used to improve adherence to asthma guidelines. Multi-Colored Simplified Asthma Guideline Reminder (MSAGR) is a NAEPP guideline-based, user-friendly single-sheet practical asthma tool designed for physicians [54]. Utilization of MSAGR promoted better adherence to guidelines and resulted in fewer emergency room visits and hospitalizations [55, 56]. Renzi et al. [57] introduced a new clinical tool: a memory aid in the form of a self-inking paper stamp checklist summarizing CPG criteria and guidelines for assessing patient control and therapy. They evaluated the knowledge of primary care physicians regarding CPGs and patient outcomes before and after the intervention. This tool significantly improved physicians' knowledge and reduced numbers of emergency room visits and hospitalizations. Additionally, reminders in other formats, including the Asthma Toolbox [58], and an asthma desktop tool [59], were used as decision-support tools for asthma management and were reported to improve the quality of care.
AsthmaCritic is another decision-support system that operates within a computer system with electronic medical records [60, 61]. It reviews physicians' treatment in the light of current guidelines and the knowledge base and generates patient-specific feedback in the form of critical comments. AsthmaCritic was developed to use routinely recorded data, to be integrated with daily practice, and to be part of a physician's working environment. This tool was shown to change the manner in which physicians monitored their patients as well as their treatment patterns and data-recording habits [60].
Many computer-assisted asthma-management programs have recently been developed [62, 63]. An automated asthma medication-management information system (MMIS) was implemented in a primary care setting as a patient-specific evaluative guidance tool [62]. MMIS collected patients' detailed asthma medication data and evaluated pharmacotherapy based on disease severity and symptom control. The program compares actual medication to a guideline-based medication index and produces a patient-specific feedback report on the appropriateness of their prescriptions.
Asthma is predominately managed by primary care physicians. Thus, asthma guidelines should be easily accessible and understandable for physicians. Previous studies have shown that general medical practice may achieve favorable clinical outcomes by more efficiently using computer-based disease management systems [64, 65]. Electronic medical record (EMR) systems have become popular. Thus, integrating computer-based decision-support tools with EMR systems can be an effective strategy for implementing asthma guidelines in clinical practice. In Korea, our group devised a practical and simple computer-based program named Easy Asthma Management (EAM), which is focused on asthma treatment and monitoring [63]. Using this program, we evaluated whether physicians' use of and adherence to asthma guidelines were improved when the guideline were presented in a computer-based format. Interestingly, clinical outcomes such as patients' asthma symptoms were improved after intervention using the EAM program, and the prescription patterns of physicians were changed such that they more closely reflected recommendations in the guidelines. This computer-assisted asthma-management program can be a useful tool for increasing the adherence of physicians to guidelines.
Dissemination and implementation of asthma guidelines are key issues for the translation of scientific knowledge into real practice and the realization of evidence-based medicine in asthma patient care. Various education programs and decision-support tools have been designed and applied to the clinical management of asthma to solve these challenging problems. Many of them have been shown to be effective at increasing physicians' knowledge and adherence to asthma guidelines and improving patients' clinical outcomes. Educational and decision-support tools are expected to contribute to a narrowing of the gap between asthma guidelines and practice/implementation of the guidelines. Further studies and novel attempts to overcome guideline implementation issues and improve actual asthma care are needed in the future.
ACKNOWLEDGEMENTS
This study was supported by a grant of the Korea Healthcare technology R&D Project, Ministry of Health and Welfare, Republic of Korea (A102065).
References
2. Masoli M, Fabian D, Holt S, Beasley R. The global burden of asthma: executive summary of the GINA Dissemination Committee report. Allergy. 2004; 59:469–478. PMID: 15080825.

3. Rabe KF, Adachi M, Lai CK, Soriano JB, Vermeire PA, Weiss KB, Weiss ST. Worldwide severity and control of asthma in children and adults: the global asthma insights and reality surveys. J Allergy Clin Immunol. 2004; 114:40–47. PMID: 15241342.

5. Myers TR. Guidelines for asthma management: a review and comparison of 5 current guidelines. Respir Care. 2008; 53:751–767. PMID: 18501029.
6. Fuhlbrigge AL, Adams RJ, Guilbert TW, Grant E, Lozano P, Janson SL, Martinez F, Weiss KB, Weiss ST. The burden of asthma in the United States: level and distribution are dependent on interpretation of the national asthma education and prevention program guidelines. Am J Respir Crit Care Med. 2002; 166:1044–1049. PMID: 12379546.
7. Rabe KF, Vermeire PA, Soriano JB, Maier WC. Clinical management of asthma in 1999: the Asthma Insights and Reality in Europe (AIRE) study. Eur Respir J. 2000; 16:802–807. PMID: 11153575.

8. Vermeire PA, Rabe KF, Soriano JB, Maier WC. Asthma control and differences in management practices across seven European countries. Respir Med. 2002; 96:142–149. PMID: 11905548.

9. Zainudin BM, Lai CK, Soriano JB, Jia-Horng W, De Guia TS. Asthma control in adults in Asia-Pacific. Respirology. 2005; 10:579–586. PMID: 16268910.

10. Tan WC, Aït-Khaled N. Dissemination and implementation of guidelines for the treatment of asthma. Int J Tuberc Lung Dis. 2006; 10:710–716. PMID: 16848330.
11. Woolcock A, Rubinfeld AR, Seale JP, Landau LL, Antic R, Mitchell C, Rea HH, Zimmerman P. Thoracic society of Australia and New Zealand. Asthma management plan, 1989. Med J Aust. 1989; 151:650–653. PMID: 2593911.
12. Hargreave FE, Dolovich J, Newhouse MT. The assessment and treatment of asthma: a conference report. J Allergy Clin Immunol. 1990; 85:1098–1111. PMID: 2355155.

13. Guidelines for management of asthma in adults: I--Chronic persistent asthma. Statement by the British Thoracic Society, Research Unit of the Royal College of Physicians of London, King's Fund Centre, National Asthma Campaign. BMJ. 1990; 301:651–653. PMID: 1977482.
14. Expert panel report 1: Guidelines for the diagnosis and management of asthma. 1991. Bethesda: National Institutes of Health, National Asthma Education and Prevention Program.
15. Lung and Blood Institute: National Institute of Health. Global Strategy for Asthma Management and Prevention. WHO/NHLBI workshop report. 1995.
16. Global Initiative for Asthma (GINA). Global Strategy for Asthma Management and Prevention. Revised 2006. Available from: http://www.seicap.es/documentos/archivos/GINA2006general.pdf.
17. Lalloo UG, Walters RD, Adachi M, de Guia T, Emelyanov A, Fritscher CC, Hong J, Jimenez C, King GG, Lin J, Loaiza A, Nadeau G, Neffen H, Sekerel BE, Yorgancıoğlu A, Zar HJ. Asthma programmes in diverse regions of the world: challenges, successes and lessons learnt. Int J Tuberc Lung Dis. 2011; 15:1574–1587. PMID: 21888756.

18. Kim YY. Past, present, and future of allergy in Korea. Allergy Asthma Immunol Res. 2010; 2:155–164. PMID: 20592913.

19. Boulet LP, Borduas F, Bouchard J, Blais J, Hargreave FE, Rouleau M. Playing cards on asthma management: a new interactive method for knowledge transfer to primary care physicians. Can Respir J. 2007; 14:480–484. PMID: 18060093.

20. Le TT, Rait MA, Jarlsberg LG, Eid NS, Cabana MD. A randomized controlled trial to evaluate the effectiveness of a distance asthma learning program for pediatricians. J Asthma. 2010; 47:245–250. PMID: 20394510.

21. Freeman AC, Sweeney K. Why general practitioners do not implement evidence: qualitative study. BMJ. 2001; 323:1100–1102. PMID: 11701576.

22. Bateman ED, Boushey HA, Bousquet J, Busse WW, Clark TJ, Pauwels RA, Pedersen SE. Can guideline-defined asthma control be achieved? The Gaining Optimal Asthma ControL study. Am J Respir Crit Care Med. 2004; 170:836–844. PMID: 15256389.
23. Bateman ED, Bousquet J, Busse WW, Clark TJ, Gul N, Gibbs M, Pedersen S. Stability of asthma control with regular treatment: an analysis of the Gaining Optimal Asthma controL (GOAL) study. Allergy. 2008; 63:932–938. PMID: 18588561.

24. Bateman ED, Reddel HK, Eriksson G, Peterson S, Ostlund O, Sears MR, Jenkins C, Humbert M, Buhl R, Harrison TW, Quirce S, O'Byrne PM.the relationship between current control and future risk. J Allergy Clin Immunol. 2010; 125:600–608. 608.e1–608.e6. PMID: 20153029.
25. Buhl R, Vogelmeier C. Budesonide/formoterol maintenance and reliever therapy: a new treatment approach for adult patients with asthma. Curr Med Res Opin. 2007; 23:1867–1878. PMID: 17605896.

26. Neffen H, Fritscher C, Schacht FC, Levy G, Chiarella P, Soriano JB, Mechali D. Asthma control in Latin America: the Asthma Insights and Reality in Latin America (AIRLA) survey. Rev Panam Salud Publica. 2005; 17:191–197. PMID: 15826399.

27. Adachi M, Ohta K, Morikawa A, Nishima S, Tokunaga S, Disantostefano RL. Changes in asthma insights and reality in Japan (AIRJ) in 2005 since 2000. Arerugi. 2008; 57:107–120. PMID: 18349585.
28. Bourdin A, Doble A, Godard P. The Asthma Insights and Reality in the Maghreb (AIRMAG) study: perspectives and lessons. Respir Med. 2009; 103(Suppl 2):S38–S48. PMID: 20122628.

29. Cho SH, Kim YK, Chang YS, Kim SS, Min KU, Kim YY. Asthma insights and reality in Korea. Korean J Med. 2006; 70:69–77.
30. Lai CK, De Guia TS, Kim YY, Kuo SH, Mukhopadhyay A, Soriano JB, Trung PL, Zhong NS, Zainudin N, Zainudin BM. Asthma control in the Asia-Pacific region: the Asthma Insights and Reality in Asia-Pacific Study. J Allergy Clin Immunol. 2003; 111:263–268. PMID: 12589343.

31. Lai CK, Ko FW, Bhome A, DE Guia TS, Wong GW, Zainudin BM, Nang AN, Boonsawat W, Cho SH, Gunasekera KD, Hong JG, Hsu JY, Viet NN, Yunus F, Mukhopadhyay A. Relationship between asthma control status, the Asthma Control Test™ and urgent health-care utilization in Asia. Respirology. 2011; 16:688–697. PMID: 21362102.

32. Boulet LP, Becker A, Bowie D, Hernandez P, McIvor A, Rouleau M, Bourbeau J, Graham ID, Logan J, Légaré F, Ward TF, Cowie RL, Drouin D, Harris SB, Tamblyn R, Ernst P, Tan WC, Partridge MR, Godard P, Herrerias CT, Wilson JW, Stirling L, Rozitis EB, Garvey N, Lougheed D, Labrecque M, Rea R, Holroyde MC, Fagnan D, Dorval E, Pogany L, Kaplan A, Cicutto L, Allen ML, Moraca S, FitzGerald JM, Borduas F. Implementing practice guidelines: a workshop on guidelines dissemination and implementation with a focus on asthma and COPD. Can Respir J. 2006; 13(Suppl A):5–47. PMID: 16552449.

33. Kang MK, Kim BK, Kim TW, Kim SH, Kang HR, Park HW, Chang YS, Kim SS, Min KU, Kim YY, Cho SH. Physicians' preferences for asthma guidelines implementation. Allergy Asthma Immunol Res. 2010; 2:247–253. PMID: 20885909.

34. Stone TT, Schweikhart SB, Mantese A, Sonnad SS. Guideline attribute and implementation preferences among physicians in multiple health systems. Qual Manag Health Care. 2005; 14:177–187. PMID: 16027596.

35. Stone TT, Kivlahan CH, Cox KR. Evaluation of physician preferences for guideline implementation. Am J Med Qual. 1999; 14:170–177. PMID: 10452134.

36. Sullivan SD, Lee TA, Blough DK, Finkelstein JA, Lozano P, Inui TS, Fuhlbrigge AL, Carey VJ, Wagner E, Weiss KB. A multisite randomized trial of the effects of physician education and organizational change in chronic asthma care: cost-effectiveness analysis of the Pediatric Asthma Care Patient Outcomes Research Team II (PAC-PORT II). Arch Pediatr Adolesc Med. 2005; 159:428–434. PMID: 15867115.
37. Sarrell EM, Mandelberg A, Cohen HA, Kahan E. Compliance of primary care doctors with asthma guidelines and related education programs: the employment factor. Isr Med Assoc J. 2002; 4:403–406. PMID: 12073408.
38. Davis DA, Thomson MA, Oxman AD, Haynes RB. Evidence for the effectiveness of CME. A review of 50 randomized controlled trials. Jama. 1992; 268:1111–1117. PMID: 1501333.

39. Lougheed MD, Moosa D, Finlayson S, Hopman WM, Quinn M, Szpiro K, Reisman J. Impacts of a provincial asthma guidelines continuing medical education project: The Ontario Asthma Plan of Action's Provider Education in Asthma Care Project. Can Respir J. 2007; 14:111–117. PMID: 17372639.
40. Davis D, O'Brien MA, Freemantle N, Wolf FM, Mazmanian P, Taylor-Vaisey A. Impact of formal continuing medical education: do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes. JAMA. 1999; 282:867–874. PMID: 10478694.
41. Davis RS, Bukstein DA, Luskin AT, Kailin JA, Goodenow G. Changing physician prescribing patterns through problem-based learning: an interactive, teleconference case-based education program and review of problem-based learning. Ann Allergy Asthma Immunol. 2004; 93:237–242. PMID: 15478382.

42. White M, Michaud G, Pachev G, Lirenman D, Kolenc A, FitzGerald JM. Randomized trial of problem-based versus didactic seminars for disseminating evidence-based guidelines on asthma management to primary care physicians. J Contin Educ Health Prof. 2004; 24:237–243. PMID: 15709563.

43. Davis DA, Thomson MA, Oxman AD, Haynes RB. Changing physician performance. A systematic review of the effect of continuing medical education strategies. JAMA. 1995; 274:700–705. PMID: 7650822.

44. Bero LA, Grilli R, Grimshaw JM, Harvey E, Oxman AD, Thomson MA. Closing the gap between research and practice: an overview of systematic reviews of interventions to promote the implementation of research findings. The Cochrane Effective Practice and Organization of Care Review Group. BMJ. 1998; 317:465–468. PMID: 9703533.
45. Van Sickle D, Singh RB. A video-simulation study of the management of asthma exacerbations by physicians in India. Clin Respir J. 2008; 2:98–105. PMID: 20298314.

46. Lougheed MD, Olajos-Clow JG. Asthma care pathways in the emergency department. Curr Opin Allergy Clin Immunol. 2010; 10:181–187. PMID: 20431367.

47. Allen D, Gillen E, Rixson L. Systematic review of the effectiveness of integrated care pathways: what works, for whom, in which circumstances? Int J Evid Based Healthc. 2009; 7:61–74. PMID: 21631848.
48. Wazeka A, Valacer DJ, Cooper M, Caplan DW, DiMaio M. Impact of a pediatric asthma clinical pathway on hospital cost and length of stay. Pediatr Pulmonol. 2001; 32:211–216. PMID: 11536450.

49. Norton SP, Pusic MV, Taha F, Heathcote S, Carleton BC. Effect of a clinical pathway on the hospitalisation rates of children with asthma: a prospective study. Arch Dis Child. 2007; 92:60–66. PMID: 16905562.

50. Guttmann A, Zagorski B, Austin PC, Schull M, Razzaq A, To T, Anderson G. Effectiveness of emergency department asthma management strategies on return visits in children: a populationbased study. Pediatrics. 2007; 120:e1402–e1410. PMID: 18055658.

51. Dalcin Pde T, da Rocha PM, Franciscatto E, Kang SH, Menegotto DM, Polanczyk CA, Barreto SS. Effect of clinical pathways on the management of acute asthma in the emergency department: five years of evaluation. J Asthma. 2007; 44:273–279. PMID: 17530525.
52. Bailey R, Weingarten S, Lewis M, Mohsenifar Z. Impact of clinical pathways and practice guidelines on the management of acute exacerbations of bronchial asthma. Chest. 1998; 113:28–33. PMID: 9440564.

53. Lougheed MD, Olajos-Clow J, Szpiro K, Moyse P, Julien B, Wang M, Day AG. Multicentre evaluation of an emergency department asthma care pathway for adults. CJEM. 2009; 11:215–229. PMID: 19523270.

54. Ting S. Multi-colored simplified asthma guideline reminder: why pragmatic asthma tools are needed in real-world practice. Clin Rev Allergy Immunol. 2004; 27:133–145. PMID: 15576897.

55. Ting S. Multicolored simplified asthma guideline reminder (MSAGR) for better adherence to national/global asthma guidelines. Ann Allergy Asthma Immunol. 2002; 88:326–330. PMID: 11926628.

56. O'Laughlen MC, Hollen P, Ting S. An intervention to change clinician behavior: Conceptual framework for the multicolored simplified asthma guideline reminder (MSAGR). J Am Acad Nurse Pract. 2009; 21:417–422. PMID: 19689437.
57. Renzi PM, Ghezzo H, Goulet S, Dorval E, Thivierge RL. Paper stamp checklist tool enhances asthma guidelines knowledge and implementation by primary care physicians. Can Respir J. 2006; 13:193–197. PMID: 16779463.

58. Shapiro A, Gracy D, Quinones W, Applebaum J, Sarmiento A. Putting guidelines into practice: improving documentation of pediatric asthma management using a decision-making tool. Arch Pediatr Adolesc Med. 2011; 165:412–418. PMID: 21536955.
59. Campbell J, Campbell S, Woodward G. Getting evidence into practice using an asthma desktop tool. Aust Fam Physician. 2006; 35:32–33. PMID: 16489383.
60. Kuilboer MM, van Wijk MA, Mosseveld M, van der Does E, de Jongste JC, Overbeek SE, Ponsioen B, van der Lei J. Computed critiquing integrated into daily clinical practice affects physicians' behavior--a randomized clinical trial with AsthmaCritic. Methods Inf Med. 2006; 45:447–454. PMID: 16964364.
61. Kuilboer MM, van Wijk MA, Mosseveld M, van der Does E, Ponsioen BP, de Jongste JC, Overbeek SE, van der Lei J. Feasibility of AsthmaCritic, a decision-support system for asthma and COPD which generates patient-specific feedback on routinely recorded data in general practice. Fam Pract. 2002; 19:442–447. PMID: 12356691.

62. Twiggs JE, Fifield J, Jackson E, Cushman R, Apter A. Treating asthma by the guidelines: developing a medication management information system for use in primary care. Dis Manag. 2004; 7:244–260. PMID: 15669584.

63. Cho SH, Jeong JW, Park HW, Pyun BY, Chang SI, Moon HB, Kim YY, Choi BW. Effectiveness of a computer-assisted asthma management program on physician adherence to guidelines. J Asthma. 2010; 47:680–686. PMID: 20632781.

64. Hunt DL, Haynes RB, Hanna SE, Smith K. Effects of computer-based clinical decision support systems on physician performance and patient outcomes: a systematic review. JAMA. 1998; 280:1339–1346. PMID: 9794315.
65. Shiffman RN, Liaw Y, Brandt CA, Corb GJ. Computer-based guideline implementation systems: a systematic review of functionality and effectiveness. J Am Med Inform Assoc. 1999; 6:104–114. PMID: 10094063.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download