Abstract
Background
A herbal preparation, known as RMIT Chinese Medicine 102 (RCM-102) consisting of eight herbs which demonstrates inhibition of the release of key inflammatory mediators associated with seasonal allergic rhinitis (SAR) was used. This study evaluated the efficacy and safety of RCM-102 for SAR.
Methods
This randomised placebo-controlled trial involved subjects aged between 18 and 65 who were randomly assigned to either RCM-102 or a placebo group. After a two-week baseline period, all subjects took either RCM-102 or placebo capsules (two capsules each time, three times daily with a four hour interval) for a period of eight weeks. The primary end-points were the Five-Point Scale symptom scores. Rhinoconjunctivitis Quality of Life Questionnaire, relief medication usage, adverse events, kidney and liver function tests and full blood examination were secondary end-points. Intention-to-treat analysis was applied.
Results
One hundred and four subjects were randomised with 52 in each group. Ninety-five subjects (47 and 48 subjects in RCM-102 and placebo groups) completed the trial. Nine subjects withdrew from the study prior to the end of the second treatment week. At the end of the trial, there were no significant differences between the two groups with respect to all outcome measures. There were no liver or kidney function abnormalities reported.
Herbal medicine (HM) has a long history in China for treating clinical conditions including allergy. Over several decades, it has gained popularity in developed countries [1, 2]. The general principle in Chinese medicine is to modify response to allergic triggers such as pollens. It is anticipated that once the bodily functions are improved, quality of life should be enhanced.
Traditionally, individual Chinese herbs are used in combination guided by its unique theory on maintaining and restoring body balance [3]. Traditional understanding of herb-herb interactions such as synergism and antagonism are considered during the formulation process [4]. Consequently, numerous herbal formulae are documented in the HM literature and are used in everyday practice.
This traditional form of practice is largely anecdotal and is subject to scientific scrutiny for its clinical efficacy and mechanisms of action [1, 2]. A number of traditional formulae have demonstrated effectiveness of CHMs for allergic rhinitis (AR) but their action mechanisms are yet to be elucidated [1, 2].
The Western pharmacological approach to HM identified a number of active components leading to drug discoveries but were unsuccessful for traditional medicine practice [3]. Consequently, Tang et al. [5] recommended investigating pharmacological actions only after demonstration of clinical efficacy of HM. This approach avoids unnecessary basic research into ineffective therapy.
We have used a combined approach: we chose a herbal formula that consists of 18 herbs known to be effective for treatment of AR [6]. In vitro investigations revealed the effects of the ingredients of this formula on key inflammatory mediators relevant to the pathophysiology of AR [7-9]. This led to identification of seven of the 18 herbs from the original formulation with one additional ingredient (Scutellaria baicalensis georgi.) totalling eight herbs in this new formulation, RCM-102. When tested it showed significant inhibitory pharmacological effects on inflammatory mediators relevant to rhinitis [10]. In this clinical trial, we explored whether RCM-102 is efficacious and safe for symptom management and improving quality of life for seasonal AR (SAR) patients.
The trial was approved by the RMIT University Human Research Ethics Committee. Application (2003/70) was filed with the Clinical Trials Branch under its Clinical Trial Notification Scheme, Therapeutic Goods Administration (TGA), Department for Health and Ageing, Canberra, Australia. This clinical trial also has been registered with Australian and New Zealand Clinical Trial Registry (ACTRN12612000209897).
The study was conducted from September to December 2003 during the pollen season in Melbourne, Australia. Daily pollen counts were provided by School of Botany, University of Melbourne. There were two clinical sites for this trial, at the City Campus and Bundoora Campus of RMIT University.
During August and September 2003, subjects were recruited through newspapers and radio. Inclusion criteria were: (a) age between 18 to 65 years with two or more symptoms for at least two years with a total nasal symptom score of at least six; (b) a positive pollen skin prick test (SPT).
Subjects with any of the following conditions were excluded from the study: (a) initiated immunotherapy since last SAR season; (b) HIV positive; (c) other active respiratory disease within 30 days of study; (d) receiving oral corticosteroid treatment; (e) pregnancy or lactation; (f) nasal polyposis; and (g) unable to read or understand English.
All subjects provided informed consent prior to the trial and were free to withdraw at any time. Subjects were advised to continue with pre-existing treatment for rhinitis or concomitant illnesses providing details of medication usage were recorded in the medication record form.
Questionnaires were used to obtain subjects' demographic data. The primary outcome measure for assessing severity of SAR symptoms was a Five-Point Scale (0 = absent, 1 = mild, 2 = moderate, 3 = severe, 4 = very severe) [11]. Nasal symptoms included sneezing, nasal discharge, nasal itch, and nasal obstruction while non-nasal symptoms included eye itch, watery eye and red eye, itch of palate and or throat were recorded daily. Rhinoconjunctivitis Quality of Life Questionnaire (RQLQ) was used as a secondary outcome measure (QOL Technologies, UK). RQLQ has 28 items in seven domains, namely, activity limitations, sleep impairments, non-nose/eye symptoms, practical problems, nasal symptoms, eye symptoms, and emotional functions [12]. This self-administered instrument assessed the impact of SAR symptoms on the subjects' quality of life. The self-assessment was based on a seven-point scale ranging from not troubled (0) to extremely troubled (6). To monitor medication intake, subjects recorded details of daily Western medication intake during the trial. The relief medication score was calculated using the following scoring system: Nasal spray or eye drop (Over the Counter, OTC): each daily dose = 1 point; OTC antihistamines: each daily dose = 2 points; Oral Corticosteroid or nasal sprays: each daily dose = 3 points [6].
This randomised, double-blind, placebo-controlled trial was conducted over a period of 10 weeks (two-week baseline and an eight-week treatment).
During screening, inclusion and exclusion criteria were checked and subjects fully briefed. Informed consent was obtained prior to SPT followed by examination by an ear, nose and throat (ENT) specialist. A SPT for seven-grass mix (Kentucky blue, Meadow Fescue, Orchid, Perennial Rye, Red top, Sweet Vernal & Timothy, Bermuda), Birch, Bermuda, Plantain, Cypress, Ragweed, Negative control (Saline) and positive control (Histamine: 10 mg/mL) (Richards Thomson Pty Ltd., Australia) were completed. A wheal reaction measuring 3 mm or larger than diluent control was considered positive [6]. For safety parameters, blood samples were taken for liver, kidney function and full blood examination (FBE) tests at the beginning and end of trial. Random allocation of subjects to treatment groups occurred using statistical software by the School of Mathematical and Geospatial Sciences, RMIT. The randomisation codes were broken only after data analysis by the blinded statistician [6]. Subjects attended one of the two clinics fortnightly for collection of capsules and assessment. They evaluated the effectiveness of the blinding process on study completion by answering the question "What treatment did you receive through the study?" All trial medication bottles were collected and left-over capsules counted fortnightly for compliance monitoring.
Subjects were required to take two capsules each time, three times daily (with 4 h interval) for a period of eight weeks. Each capsule contained 500 mg of a mixture of granules of either herbal medicine (Koda Internationals Pty Ltd., Australia) or placebo ingredient (rice starch; Sigma Pharmaceuticals Pty Ltd., Australia). The capsules were prepared by a TGA approved Good Manufacturing Practice (GMP) certified manufacturer (GMP Pharmaceuticals Pty Ltd., Australia). The two types of capsules were identical in weight and appearance.
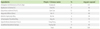
All ingredients of RCM-102 (Table 1) were TGA approved listed substances for human consumption. To comply with Australian Guidelines for Good Clinical Practice (1991), the capsule contents and known side effects of each individual ingredient were disclosed to all subjects in the trial information booklet as part of the informed consent process.
All unexpected events were recorded during the treatment period, including details of signs and severity of symptoms, duration and any actions taken to resolve them. FBE was done by the RMIT School of Medical Sciences. The liver and kidney function tests were done by Dorevitch Pathology Pty Ltd. in Melbourne, Australia prior to and after the trial.
Based on findings of a previous study [6] , the nasal symptom score for the treatment group was statistically significantly different compared to the placebo group (F = 6.118, p = 0.017). This yielded an effect size estimate of 0.66. For 80% power using a two-sided significance level of 5%, the required sample size is 38 per group. To allow for dropouts, we used a sample size of 52 per group.
All data were analysed using the Statistical Package for the Social Sciences (windows version 11.5; SPSS, USA) for Windows by a statistician blinded to the allocation of treatments to groups. When comparing measures at the end of the study for the two groups, ANCOVA was used with the baseline as covariate. The data from non-repeated measures such as blood tests was analysed using t-tests. Outcome measures with nominal responses were analysed using χ2 tests. All p-values were obtained via 2-sided tests and were assessed at α = 0.05. The age variable was used as a covariate for outcome analyses as the two treatment groups were not comparable on this variable. Intention to treat was employed in all relevant data analyses.
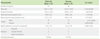
One hundred and four subjects were randomly assigned to either the RCM-102 or the placebo group. Ninety-five subjects completed the trial and nine subjects withdrew from the study (RCM-102: n = 5; placebo: n = 4) within the first two weeks of the treatment period (Fig. 1, Table 2). Of the nine subjects who withdrew, two did so due to personal circumstances, four due to work commitments and three due to adverse events from either RCM-102 or placebo capsules. Except for age, all demographic data were comparable between the two groups (Table 2).
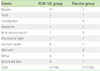
Diary documented self-assessment nasal and non-nasal symptom scores at baseline and end of the treatment period are presented in Fig. 2, with no significant differences between the groups on the severity of these symptoms. There were no significant differences between the two groups in all domains of the fortnightly RQLQ scores throughout the study (Table 3).
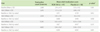
There were no statistically significant differences in mean relief medication score within or between the RCM-104 and placebo groups between the baseline and the final visit (Table 4). Based on responses to the type of treatment received, there was no significant difference in the responses (χ2 = 2.03, p = 0.363) between the two groups.
The majority of adverse events occurred during the first two weeks of treatment. Fifteen subjects reported adverse events (RCM-102: n = 6; placebo: n = 9). Throughout the trial none of the subjects experienced serious adverse events (Table 2). There were no significant differences between the two groups on renal, liver function and FBE tests before and after the treatment period.
This study showed no statistically significant difference with respect to SAR symptom scores in subjects receiving RCM-102 compared with placebo. These findings are inconsistent with in vitro results that showed significant inhibitory effects of RCM-102 on various inflammatory mediators [13]. It is important to note that RCM-102 is not an existing herbal formulation, unlike most of the traditional herbal formulae that have been used in clinical practice for an extended period of time. In contrast, this formula was developed by selecting seven out of the 18 individual herbal ingredients that were demonstrated to be beneficial for SAR symptoms using a comparable RCT design (11). The selection of the seven herbs was based on limited experimental studies that investigated the effect of some but not all inflammatory mediators. Thus, the process of selection might have been inadequate in identifying beneficial ingredients demonstrated by Xue et al. [6]. Furthermore, the investigation team added another herbal ingredient, Scutellaria baicalensis georgi, which possesses anti-inflammatory properties [14] for strengthening the anti-allergic effects of the seven herbs selected from Xue et al. [6]. However, this herb is not commonly used in traditional medicine practice on SAR patients.
Unlike recent reviews that demonstrate a positive trend in a number of traditional formulae for the management of AR [1, 2] this study, however, showed no benefit of RCM-102 for symptom scores and quality of life for SAR patients.
HM has been used to treat allergic diseases such as AR bronchial asthma and dermatitis for several centuries and with substantial evidence of clinical benefit [15]. As this study did not test a traditionally used herbal formula, a number of factors might have contributed to the lack of efficacy of RCM-102: The biological activities of a herbal formula might be an outcome of a mixture of different active ingredients rather than from an individual chemical entity or specific pathways [3]. This is supported by a number of studies such as using Radix Angelicae alone was not effective for menopausal syndrome despite its frequent clinical use [16]. In contrast, Gui Zhi Er Yue Bi Yi Tang (TJS-064) significantly protected influenza A2-infected mice whereas the individual ingredients exhibited no effect [17]. These results may suggest that complex interactions among individual ingredients or their synergistic effects in the formula of the 18 herbs (Xue et al. [6]) were not thoroughly investigated. This may have compromised the selection of the seven out of the 18 herbs that were used in RCM-102.
Furthermore, there are a number of reported cases that failed to translate laboratory findings on Chinese herbal medicine into clinical efficacy [3]. These discrepancies between clinical studies and in vitro or in vivo animal studies provide a clear warning when accepting laboratory data as the basis for determining clinical effects. For example, Shosaiko-to demonstrated beneficial effects on viral hepatitis in animal studies but failed to reach significance in the clinical trial [17]. Dang Gui Nian Tong Tang inhibited enzyme β-glucuronidase by 42% and lysozyme release from neutrophils but was not clinically effective for patients with gouty arthritis [18]. A Chinese herbal formula for dermatitis, Zemaphyte, demonstrated no benefit to Chinese patients with recalcitrant atopic dermatitis in a clinical trial [19] despite its inhibitory effects on IL4-induced low affinity receptor, IgE serum complexes and peripheral monocytes [20].
With regard to safety, the formula was well tolerated by all subjects with the exception of minor adverse events. However, there was no significant difference between the two groups with respect to frequency and severity of these events. Unlike previous reports on Chinese herbal medicine on liver and renal functions [21, 22], liver and kidney function monitoring tests showed that there were no clinically relevant changes.
RCM-102, a non-traditional herbal formula that was newly formulated based on partial understanding of SAR mechanism was well tolerated but did not show clinical efficacy based on clinical symptom scores. Additionally, these results suggest that caution be exercised in predicting clinical results from a multi-herb formulation based on basic research of its individual ingredients.
Figures and Tables
Fig. 2
Two-week mean total nasal (NSS) and non-nasal symptom scores (NNSS) with total fortnight pollen counts during the trial. Line graphs: Data plotted means ± SEM of fortnightly total NSS of RCM-102 (♦) and placebo (◊) groups, RCM-102 fortnightly total NNSS of RCM-102 (▪) and placebo (□) groups. The vertical bars show the fortnightly pollen counts. Baseline: day 14, Visit 1: day 28, Visit 2: day 42, Visit 3: day 56 and Visit 4: day 70.

ACKNOWLEDGEMENTS
This study was supported by Dr Lenon's Australian Postgraduate Award and RMIT University Research Investment Grant led by Professor Charlie Changli Xue (VRII_43, Xue et al. 2002-2005). The authors would like to thank all participants, the ENT specialists, nurses, doctors and research assistants. We acknowledge the School of Botany, University of Melbourne for supplying daily pollen count data during the trial.
References
1. Xue CC, Hügel HM, Li CG, Story DF. Efficacy, chemistry and pharmacology of Chinese herbal medicine for allergic rhinitis. Curr Med Chem. 2004. 11:1403–1421.

2. Xue CC, Li CG, Hügel HM, Story DF. Does acupuncture or Chinese herbal medicine have a role in the treatment of allergic rhinitis? Curr Opin Allergy Clin Immunol. 2006. 6:175–179.

3. Yuan R, Lin Y. Traditional Chinese medicine: an approach to scientific proof and clinical validation. Pharmacol Ther. 2000. 86:191–198.

4. Wang M, Lamers RJ, Korthout HA, van Nesselrooij JH, Witkamp RF, van der Heijden R, Voshol PJ, Havekes LM, Verpoorte R, van der Greef J. Metabolomics in the context of systems biology: bridging traditional Chinese medicine and molecular pharmacology. Phytother Res. 2005. 19:173–182.

5. Tang JL, Leung PC. An efficacy-driven approach to the research and development of traditional Chinese medicine. Hong Kong Med J. 2001. 7:375–380.
6. Xue CC, Thien FC, Zhang JJ, Da Costa C, Li CG. Treatment for seasonal allergic rhinitis by Chinese herbal medicine: a randomized placebo controlled trial. Altern Ther Health Med. 2003. 9:80–87.
7. Lenon GB, Li CG, Xue CC, Thien FC, Story DF. Inhibition of release of vasoactive and inflammatory mediators in airway and vascular tissues and macrophages by a chinese herbal medicine formula for allergic rhinitis. Evid Based Complement Alternat Med. 2007. 4:209–217.

8. Lenon GB, Li CG, Xue CC, Thien FC, Story DF. Inhibition of inducible nitric oxide production and iNOS protein expression in lipopolysaccharide-stimulated rat aorta and Raw 264.7 macrophages by ethanol extract of a Chinese herbal medicine formula (RCM-101) for allergic rhinitis. J Ethnopharmacol. 2008. 116:547–553.

9. Lenon GB, Xue CC, Story DF, Thien FC, McPhee S, Li CG. Inhibition of release of inflammatory mediators in primary and cultured cells by a Chinese herbal medicine formula for allergic rhinitis. Chin Med. 2007. 2:2.
10. Lenon GB, Xue CC, Story DF, Thien FC, Li CG. Inhibition of release of inflammatory mediators in rat peritoneal mast cells and murine macrophages by a Chinese herbal medicine formula (RCM-102). Phytother Res. 2009. 23:1270–1275.

11. Whitcup SM, Bradford R, Lue J, Schiffman RM, Abelson MB. Efficacy and tolerability of ophthalmic epinastine: a randomized, double-masked, parallel-group, active- and vehicle-controlled environmental trial in patients with seasonal allergic conjunctivitis. Clin Ther. 2004. 26:29–34.

12. Juniper EF, Thompson AK, Ferrie PJ, Roberts JN. Development and validation of the mini Rhinoconjunctivitis Quality of Life Questionnaire. Clin Exp Allergy. 2000. 30:132–140.

13. Lenon GB, Xue CL, Li CG. Pharmacological actions of Chinese herbal formula (RCM-102). 2004. Sydney: The Australian Health & Medical Research Congress.
14. Kimata M, Shichijo M, Miura T, Serizawa I, Inagaki N, Nagai H. Effects of luteolin, quercetin and baicalein on immunoglobulin E-mediated mediator release from human cultured mast cells. Clin Exp Allergy. 2000. 30:501–508.

15. But P, Chang C. Chinese herbal medicine in the treatment of asthma and allergies. Clin Rev Allergy Immunol. 1996. 14:253–269.

16. Hirata JD, Swiersz LM, Zell B, Small R, Ettinger B. Does dong quai have estrogenic effects in postmenopausal women? A double-blind, placebo-controlled trial. Fertil Steril. 1997. 68:981–986.

17. Borchers AT, Sakai S, Henderson GL, Harkey MR, Keen CL, Stern JS, Terasawa K, Gershwin ME. Shosaiko-to and other Kampo (Japanese herbal) medicines: a review of their immunomodulatory activities. J Ethnopharmacol. 2000. 73:1–13.

18. Chou CT, Kuo SC. The anti-inflammatory and anti-hyperuricemic effects of Chinese herbal formula danggui-nian-tong-tang on acute gouty arthritis: a comparative study with indomethacin and allopurinol. Am J Chin Med. 1995. 23:261–271.

19. Fung AY, Look PC, Chong LY, But PP, Wong E. A controlled trial of traditional Chinese herbal medicine in Chinese patients with recalcitrant atopic dermatitis. Int J Dermatol. 1999. 38:387–392.

20. Latchman Y, Banerjee P, Poulter LW, Rustin M, Brostoff J. Association of immunological changes with clinical efficacy in atopic eczema patients treated with traditional Chinese herbal therapy (Zemaphyte). Int Arch Allergy Immunol. 1996. 109:243–249.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download