Abstract
Background
Identifying toddlers at increased risk of developing persistent wheeze provides an opportunity for risk-reducing interventions. House dust mite (HDM) allergen sensitization might identify this group of high-risk children.
Objective
We examined whether a positive skin prick test (SPT) to at least 1 of the 3 HDMs in wheezing toddlers, would serve as a predictor for persistent wheeze at age 8 to 14 years old.
Methods
A cohort of 78 children, who had wheezing episodes, and underwent SPT to 3 HDMs between the ages of 2 to 5 years old, were enrolled. SPT results were obtained from the National University Hospital database. Four to 9 years later, the children, currently between 8 to 14 years old, were re-assessed for persistence of asthma symptoms and other atopic disorders via a telephone interview. A validated questionnaire on current wheezing and asthma, developed by the International Study of Asthma and Allergies in Childhood, was used. Fisher's exact test was used to evaluate the association between persistence of asthma and a positive SPT.
Results
Of the 78 children who participated in the study, 42 (53.8%) had a positive SPT and 36 (46.2%) had a negative SPT. Of these, 18 (42.9%) of SPT positive and 7 (19.4%) of SPT negative children had persistence of asthma symptoms. There is a significant association between a positive SPT during the preschool years, and persistence of asthma (p = 0.0314 [<0.05]).
Parents of wheezy infants and toddlers often ask, "When will my child ever grow out of his or her asthmatic symptoms?" This is a question that many physicians involved would like to be able to answer. Wheezing is one of the most common symptoms in preschoolers. Previous studies done in Singapore showed that 25% of toddlers had wheezing before the age of two years [1]. Other population studies have also demonstrated that approximately one in three children have at least one episode of wheezing before the age of 3 years, and that the cumulative prevalence of wheeze is almost 50% at the age of 6 years [2]. However, in spite of the high prevalence, there is little evidence regarding the pathophysiology and treatment of preschool wheezing [3].
In preschool children, not only are there different phenotypes of wheezing, the etiology of wheeze is also heterogeneous. Two major distinct phenotypes have been distinguished in previous studies: virus-induced wheezing (i.e. non-atopic), and multi-trigger (i.e. atopic) wheezing. Virus-induced wheezing, which makes up about two-thirds of all preschool wheezing, is an intermittent form of recurrent airway obstruction with normal pre-morbid lung function and asymptomatic periods between attacks. These children have a favorable prognosis, and usually only need supportive treatment. On the other hand, multi-trigger wheezing is associated with an underlying allergic constitution, and is less prevalent in preschool children. This form of wheezing tends to occur during and between episodes and is more likely to persist beyond early childhood, with associated significant deficits in lung growth up to 11 years of age [3, 4].
There is great value in being able to distinguish the persistent wheezers from the transient ones amongst preschool children for the sake of better disease management. This is because a longer duration of wheeze is associated with an increase in disease severity and more troublesome disease [5].
Studies that have been done so far have given a clinical profile of preschool children who were at increased risk of developing persistent wheeze. These factors include gender (male>female), positive atopic status, previous respiratory syncytial virus infection and the lack of anti-inflammatory treatment, especially inhaled corticosteroids. However, these factors still require further investigation and are still insufficient in helping us predict the prognosis of the disease in this age group [6].
There is general consensus among various studies that other atopic conditions, such as allergic rhinitis, atopic eczema and food allergy; and family history of atopy are factors associated with persistent wheeze [7-10]. Furthermore, in a large cohort study performed in Germany, it was demonstrated that any allergic sensitization in early life significantly increased the risk of becoming asthmatic at an older age [11]. Clinical and objective measurement of allergic sensitization can be achieved via two methods - skin prick test (SPT) or serum immunoglobulin E (IgE) testing. Although there is concordance among various studies that increased serum IgE is associated with persistence of asthma [12, 13], a clear relationship between positive SPT and asthma persistence is difficult to establish [10, 14, 15].
Thus, the objective of this study is to determine the association of a positive SPT to house dust mites (HDMs) on wheezing preschool children in Singapore and persistent wheezing at age of 8 to 14 years old.
This is a prospective cohort study investigating the use of a positive skin prick test as a predictor for persistent wheezing in a group of children between 8 and 14 years old via a telephone interview.
Singaporean children aged between 2 and 5 years, who had at least one wheezing episode and a skin prick test done between January 2002 and December 2006, were recruited in the study. Between 4 to 9 years after the skin prick tests were done, the children who were between the ages of eight to fourteen now, were reassessed for the persistence of asthmatic symptoms and presence of other atopic co-morbidities (i.e. chronic rhinitis, eczema, food allergies) via a telephone interview.
According to the literature [16], it is estimated that about 20% of SPT negative and 80% of SPT positive preschool children will develop persistent wheezing. To achieve a statistical significance at 95% confidence interval with the power set at 80%, the total number of patients needed for the study is 80 (40 on each arm).
Ethics approval was obtained from the Singapore domain specific review board (DSRB B/2011/01843).
All skin prick tests results between January 2002 and December 2006 were collected. The medical records of the children were obtained, and information regarding the clinical condition at the time of SPT were likewise retrieved.
All participating subjects underwent skin prick testing at ages two to five years old. Three types of common house dust mites in Singapore were tested: Blomia tropicalis, Dermatophagoides pteronyssinus, and Dermatophagoides farinae [17]. These were performed on the volar surface of the forearm. Histamine phosphate (1 mg/mL) and physiologic saline were used as positive and negative controls respectively. The results were read at 15 min, and the mean wheal size was represented as (X + x)/2 (X is the maximum diameter, and x is the perpendicular diameter). Mean wheal size of greater than or equal to 3 mm was regarded as positive.
A validated questionnaire on current wheezing and asthma was used. This was based on the core questionnaires developed by the International Study of Asthma and Allergies in Childhood (ISAAC) for persistent wheeze, rhinitis, and eczema. Parents of the children recruited in the study completed these questionnaires via a telephone interview conducted by two of the authors, who were medical students. The interviewers were trained prior to the interview and familiarised with the study algorithm.
All statistical analyses were performed using SPSS ver. 17.0 (SPSS, USA). Baseline differences between the positive and negative SPT groups were evaluated with Pearson's chi-square, Fisher's exact and Mann-Whitney U tests. Associations between persistence of wheeze, rhinitis and eczema with a positive SPT were evaluated with Fisher's exact test. A p value of <0.05 was considered statistically significant. Relative risks, along with the 95% confidence intervals, of developing persistent wheeze, rhinitis and eczema with a positive SPT were also calculated
Of the 78 children who participated in the study, 42 (53.8%) out of the 78 children had a positive SPT to at least one HDM and 36 (46.2%) of them had a negative SPT.
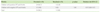
Baseline demographics of children with positive SPT were compared against the baseline demographics of children with negative SPT. Baseline demographics used for comparison included gender, ethnicity, concomitant atopic conditions (allergic rhinitis, atopic dermatitis, allergic conjunctivitis, food allergies), frequency of wheezing during the first two year after SPT, age when SPT was done, number of previous hospitalizations due to wheezing episodes during the first two years after SPT, number of courses of oral prednisolone during the first two years after SPT and usage of maintenance steroid inhalers during the first two years after SPT. Differences in baseline demographics between the two groups were found to be statistically insignificant (p value > 005) using Pearson's chi-square, Fisher's exact and Mann-Whitney U tests (Table 1).
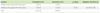
Of the 42 children with a positive SPT, 18 (42.9%) still had wheezing episodes. Seven (19.4%) out of the 36 children with a negative SPT still had wheezing episodes. The association of a positive SPT with the persistence of wheezing is statistically significant, as two-tailed p value using the Fisher's exact test is 0.0314 (Table 2). Children with positive SPT were 2.20 times as likely as children with negative SPT to continue to have wheezing episodes 4 to 9 years after the SPT was done (95% CI: 1.04-4.67).
30 out of 42 children with positive SPT had allergic rhinitis at the time of SPT. 29 out of the 30 continued to have allergic rhinitis after four to nine years. 25 out of 36 children with negative SPT had chronic rhinitis when the SPT was done. All of them still had chronic rhinitis at the time of interview. The association of a positive SPT with the persistence of rhinitis is not statistically significant, as p value using Fisher's exact test is 1.00 (Table 3).
16 out of 42 children with positive SPT had atopic eczema at the time of SPT. 13 out of the 16 continued to have atopic eczema at the time of interview. Of the 36 children with negative SPT, 14 had chronic eczema at the time of SPT. Nine out of the 14 still had chronic eczema at the time of interview. The association of a positive SPT with the persistence of eczema symptoms is not statistically significant, as p value using Fisher's exact test is 0.226 (Table 4).
The study shows that HDM sensitization, demonstrated by a positive SPT to HDM at an early age in Singaporean children, is associated with persistence of wheeze at age 8 to 14 years old. This suggests that children who have a positive SPT to at least one of the three HDM have an increased risk of maintaining their asthma after 4 to 9 years, than those with a negative test for HDM. Thus, the findings propose the use of SPT as an objective tool to prognosticate the persistence of wheeze in toddlers, age two to five years old, presenting with recurrent wheeze.
At present, there are several theories explaining the pathogenesis of atopic wheeze, which usually results in persistent wheeze. For decades, the primary assumption is that allergy is caused by overactive immunological responses against allergens, driven by activated Th2 cells and due to aberrant T-regulatory cells [18, 19]. Recently, Turi et al postulated that the impaired epithelial barrier function that allows aeroallergens to trigger the overactive immunological responses could be a direct result of proteolytic activities of aeroallergens, including HDM [20]. The current hypothesis is that Der p1 m, the major allergen in HDM, causes injury to the epithelium and enters the tissue to induce inflammation via Toll-like receptor 4 [21, 22]. Another allergen found in HDM, Der p 2 also activates respiratory epithelial cells aggravating and resulting in a more prolonged and persistent wheeze [23].
However, as to whether HDM is causal in its relationship with atopic wheeze, resulting in persistent wheeze, it is still a common consensus that HDM sensitization is one of the strongest and most consistent associations with persistence of wheeze in various types of studies from different populations across different time periods and age groups [24-27]. Holt et al. [24], in a population where HDM was the dominant allergen, had similar findings and found that specific IgE to HDM at age two years to be a strong predictive factor of persistent wheeze by age five years (12.7% risk). The Manchester Asthma and Allergy Study group, which studied the sensitization to HDM at age 1, 3, 5, and 8 years, also established that early sensitization to HDM carries the greatest risk of persistent wheeze [27]. Similarly, the Multi-Centre Allergy Study group concluded that those with early (1 year) inhalant sensitization to be a high-risk group for asthma at age 7 years [28].
This makes a positive SPT to HDM, which demonstrates HDM sensitization, an important marker of potentially difficult and persistent wheeze in children, as it is the most common allergy in children in Singapore.
In this study, however, the association between HDM sensitization and current eczema or rhinitis was not demonstrated. Further studies, with larger population are suggested.
The differences in baseline demographics between the SPT positive and SPT negative groups were found to be statistically insignificant (p < 0.05) (Table 1). Thus, there are no potential confounding factors that may affect the results.
In conclusion, our findings have clinical implications. In areas of high HDM prevalence such as Singapore, HDM sensitization status demonstrated by a positive SPT could be used as an objective marker to identify toddlers at risk of persistent wheeze. Therefore, a positive SPT to HDM demonstrating HDM sensitization in young children with early wheeze would allow for more informed discussions between physicians and parents about subsequent risk of persistent wheeze, allowing for better management.
The limitation of this study is that all the participants were recruited from a high-risk group and therefore may differ from the general population in the prevalence of atopic and allergic disease. Further exploration can be done in populations who are not at similar risk.
Figures and Tables
ACKNOWLEDGEMENTS
The authors would like to thank Ms Siti Dahlia Bte Mohd Dali and Mr Jerome Rex Cruz for their assistance in retrieving skin prick tests results from the database.
References
1. Tan TN, Lim DLC, Chong YS, Lee BW, Van Bever HP. Prevalence of eczema symptoms in the second year of life. J Allergy Clin Immunol. 2004. 113:1078.
2. Bisgaard H, Szefler S. Prevalence of asthma-like symptoms in young children. Pediatr Pulmonol. 2007. 42:723–728.

3. Van Bever HP, Han E, Shek L, Yi Chng S, Goh D. An approach to preschool wheezing: to label as asthma. World Allergy Organiz J. 2010. 3:253–257.

4. Martinez FD. What have we learned from the Tucson Children's Respiratory Study? Paediatr Respir Rev. 2002. 3:193–197.

5. Zeiger RS, Dawson C, Weiss S. Relationships between duration of asthma and asthma severity among children in the Childhood Asthma Management Program (CAMP). J Allergy Clin Immunol. 1999. 103:376–387.

6. Van Bever HP, Desager KN, Hagendorens M. Critical evaluation of prognostic factors in childhood asthma. Pediatr Allergy Immunol. 2002. 13:77–83.

7. Martinez FD, Wright AL, Taussig LM, Holberg CJ, Halonen M, Morgan WJ. The Group Health Medical Associates. Asthma and wheezing in the first six years of life. N Engl J Med. 1995. 332:133–138.

8. Castro-Rodríguez JA, Holberg CJ, Wright AL, Martinez FD. A clinical index to define risk of asthma in young children with recurrent wheezing. Am J Respir Crit Care Med. 2000. 162:1403–1406.

9. Csonka P, Kaila M, Laippala P, Kuusela AL, Ashorn P. Wheezing in early life and asthma at school age: predictors of symptom persistence. Pediatr Allergy Immunol. 2000. 11:225–229.

11. Lau S, Nickel R, Niggemann B, Grüber C, Sommerfeld C, Illi S, Kulig M, Forster J, Wahn U, Groeger M, Zepp F, Kamin W, Bieber I, Tacke U, Wahn V, Bauer CP, Bergmann R, von Mutius E. The development of childhood asthma: lessons from the German Multicentre Allergy Study (MAS). Paediatr Respir Rev. 2002. 3:265–272.

12. Sigurs N, Bjarnason R, Sigurbergsson F, Kjellman B, Björkstén B. Asthma and immunoglobulin E antibodies after respiratory syncytial virus bronchiolitis: a prospective cohort study with matched controls. Pediatrics. 1995. 95:500–505.

13. Kotaniemi-Syrjänen A, Reijonen TM, Romppanen J, Korhonen K, Savolainen K, Korppi M. Allergen-specific immunoglobulin E antibodies in wheezing infants: the risk for asthma in later childhood. Pediatrics. 2003. 111:e255–e261.

14. Kaleyias J, Papaioannou D, Manoussakis M, Syrigou E, Tapratzi P, Saxoni-Papageorgiou P. Skin-prick test findings in atopic asthmatic children: a follow-up study from childhood to puberty. Pediatr Allergy Immunol. 2002. 13:368–374.

15. Brooke AM, Lambert PC, Burton PR, Clarke C, Luyt DK, Simpson H. The natural history of respiratory symptoms in preschool children. Am J Respir Crit Care Med. 1995. 152:1872–1878.

16. Chan EY, Dundas I, Bridge PD, Healy MJ, McKenzie SA. Skin-prick testing as a diagnostic aid for childhood asthma. Pediatr Pulmonol. 2005. 39:558–562.

17. Chew FT, Zhang L, Ho TM, Lee BW. House dust mite fauna of tropical Singapore. Clin Exp Allergy. 1999. 29:201–206.

18. Palomares O, Yaman G, Azkur AK, Akkoc T, Akdis M, Akdis CA. Role of Treg in immune regulation of allergic diseases. Eur J Immunol. 2010. 40:1232–1240.

19. Ray A, Khare A, Krishnamoorthy N, Qi Z, Ray P. Regulatory T cells in many flavors control asthma. Mucosal Immunol. 2010. 3:216–229.

20. Turi GJ, Ellis R, Wattie JN, Labiris NR, Inman MD. The effects of inhaled house dust mite on airway barrier function and sensitivity to inhaled methacholine in mice. Am J Physiol Lung Cell Mol Physiol. 2011. 300:L185–L190.

21. Hammad H, Chieppa M, Perros F, Willart MA, Germain RN, Lambrecht BN. House dust mite allergen induces asthma via Toll-like receptor 4 triggering of airway structural cells. Nat Med. 2009. 15:410–416.

22. Hongjia L, Qingling G, Meiying L, Weixuan W, Lihong Z, Yongsheng G, Yanli L, Jinxiang W, Liang D. House dust mite regulate the lung inflammation of asthmatic mice through TLR4 pathway in airway epithelial cells. Cell Biochem Funct. 2010. 28:597–603.

23. Osterlund C, Grönlund H, Polovic N, Sundström S, Gafvelin G, Bucht A. The non-proteolytic house dust mite allergen Der p 2 induce NF-kappaB and MAPK dependent activation of bronchial epithelial cells. Clin Exp Allergy. 2009. 39:1199–1208.
24. Holt PG, Rowe J, Kusel M, Parsons F, Hollams EM, Bosco A, McKenna K, Subrata L, de Klerk N, Serralha M, Holt BJ, Zhang G, Loh R, Ahlstedt S, Sly PD. Toward improved prediction of risk for atopy and asthma among preschoolers: a prospective cohort study. J Allergy Clin Immunol. 2010. 125:653–659. 659.e1–659.e7.

25. Voorhorst R, Spieksma FT, Varekamp H, Leupen MJ, Lyklema AW. The house-dust mite (Dermatophagoides pteronyssinus) and the allergens it produces. Identity with the house-dust allergen. J Allergy. 1967. 39:325–339.

26. Sporik R, Chapman MD, Platts-Mills TA. House dust mite exposure as a cause of asthma. Clin Exp Allergy. 1992. 22:897–906.

27. Simpson A, Tan VY, Winn J, Svensén M, Bishop CM, Heckerman DE, Buchan I, Custovic A. Beyond atopy: multiple patterns of sensitization in relation to asthma in a birth cohort study. Am J Respir Crit Care Med. 2010. 181:1200–1206.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download